Validating Epigenetic Biomarkers for Early Cancer Detection: From Discovery to Clinical Implementation
This article provides a comprehensive analysis of the validation pipeline for epigenetic biomarkers in early cancer detection, tailored for researchers and drug development professionals.
Validating Epigenetic Biomarkers for Early Cancer Detection: From Discovery to Clinical Implementation
Abstract
This article provides a comprehensive analysis of the validation pipeline for epigenetic biomarkers in early cancer detection, tailored for researchers and drug development professionals. We explore the foundational biology of DNA methylation and other epigenetic marks as promising cancer biomarkers, detailing advanced methodological approaches from bisulfite sequencing to AI-powered analysis. The content addresses critical troubleshooting aspects for overcoming technical and biological challenges in biomarker development and establishes rigorous frameworks for analytical and clinical validation. By synthesizing current evidence from multi-cancer early detection tests and novel epigenetic networks, this resource aims to bridge the gap between biomarker discovery and clinical implementation for precision oncology.
The Epigenetic Landscape in Cancer: Mechanisms and Biomarker Potential
Deoxyribonucleic acid (DNA) methylation represents a crucial epigenetic mechanism that regulates gene expression without altering the underlying DNA sequence. This process involves the addition of a methyl group to the 5-carbon position of cytosine rings, primarily within cytosine-phosphate-guanine (CpG) dinucleotides, resulting in 5-methylcytosine (5mC) [1]. In normal physiological conditions, DNA methylation plays fundamental roles in embryonic development, genomic imprinting, X-chromosome inactivation, and maintenance of genomic stability by suppressing transposable elements [1] [2]. The establishment and maintenance of methylation patterns are catalyzed by DNA methyltransferases (DNMTs), with DNMT3A and DNMT3B responsible for de novo methylation, and DNMT1 maintaining methylation patterns during DNA replication [1] [2].
Cancer cells exhibit profound disruptions in their DNA methylation patterns, characterized by two hallmark alterations: global genomic hypomethylation and focal CpG island hypermethylation [3] [4] [1]. Global hypomethylation promotes genomic instability and can activate oncogenes, while promoter-specific hypermethylation leads to the transcriptional silencing of tumor suppressor genes [4] [1] [2]. These alterations emerge early in tumorigenesis and remain stable throughout cancer progression, making them attractive targets for biomarker development [5] [4]. The dynamic interplay between normal methylation regulation and cancer-associated aberrations forms a critical foundation for understanding cancer biology and developing epigenetic-based diagnostic and therapeutic strategies.
Molecular Mechanisms and Technological Approaches
Enzymatic Regulation of DNA Methylation
The DNA methylation machinery consists of "writer" and "eraser" enzymes that establish and remove methylation marks, respectively. The DNMT family functions as writers, with DNMT3A and DNMT3B establishing new methylation patterns during development, while DNMT1 maintains these patterns during cell division by copying methylation marks to the daughter DNA strand [1] [2]. Active demethylation is primarily catalyzed by Ten-eleven translocation (TET) dioxygenases, which sequentially oxidize 5mC to 5-hydroxymethylcytosine (5hmC), 5-formylcytosine (5fC), and 5-carboxylcytosine (5caC) [1]. These enzymatic processes ensure the dynamic regulation of the epigenome in response to developmental and environmental signals.
In cancer, this precise regulation is disrupted. Aberrant DNMT activity leads to hypermethylation of tumor suppressor gene promoters, while impaired TET function contributes to global hypomethylation [1]. These changes create a permissive environment for malignant transformation by silencing genes involved in cell cycle control, DNA repair, and apoptosis, while simultaneously activating oncogenes and transposable elements [1] [2].
Analytical Technologies for DNA Methylation Assessment
Advances in methylation profiling technologies have revolutionized our ability to study epigenetic dynamics in cancer. These methods vary in resolution, throughput, cost, and application suitability, enabling researchers to select approaches aligned with their specific experimental goals.
Table 1: DNA Methylation Analysis Technologies
| Technology | Resolution | Throughput | Primary Applications | Key Advantages |
|---|---|---|---|---|
| Whole-Genome Bisulfite Sequencing (WGBS) | Single-base | High | Discovery, comprehensive methylome analysis | Gold standard for base-resolution whole methylome [5] [2] |
| Reduced Representation Bisulfite Sequencing (RRBS) | Single-base | Medium | Targeted discovery, CpG-rich regions | Cost-effective; focuses on CpG-dense regions [5] [6] |
| Methylation Microarrays | Single CpG site | High | Biomarker validation, large cohort studies | Cost-effective for population studies [5] [2] |
| Nanopore Sequencing | Single-base | High | Direct detection, long reads | No bisulfite conversion; detects modifications natively [5] [2] |
| Quantitative Methylation-Specific PCR (qMSP) | Locus-specific | Low | Clinical validation, targeted analysis | High sensitivity for low-abundance targets [5] [7] [2] |
| Pyrosequencing | Single CpG site | Low | Validation, quantitative analysis | Quantitative accuracy for specific CpG sites [2] |
The choice of methodology depends on research objectives, with WGBS and RRBS preferred for discovery-phase studies, while targeted approaches like qMSP and pyrosequencing are better suited for clinical validation of specific biomarkers [5] [2]. Emerging technologies such as nanopore sequencing offer particularly promising applications for liquid biopsies, as they enable direct methylation detection without chemical conversion, thereby preserving DNA integrity—a critical consideration when working with limited quantities of cell-free DNA (cfDNA) [5] [2].
DNA Methylation Biomarkers in Cancer Detection
Tissue-Based Methylation Biomarkers
Tumor tissue remains a valuable source for DNA methylation biomarker discovery and validation. Studies utilizing reduced representation bisulfite sequencing (RRBS) of breast cancer cohorts have revealed that methylation patterns in tumors follow global trends, including replication-linked hypomethylation and epigenomic instability characterized by either methylation gain (MG) or loss (ML) at CpG islands [6]. These patterns correlate with tumor grade, stage, TP53 mutations, and clinical outcomes [6]. After accounting for these global trends, researchers have identified hundreds of promoters and thousands of distal regulatory elements exhibiting cis-specific methylation-expression correlations, including established tumor suppressors and oncogenes [6].
Comprehensive methylation profiling of 1538 breast tumors identified six global trends affecting DNA methylation profiles: immune and stromal cell contamination, replication-linked hypomethylation clock, X-chromosome dosage compensation, and two processes of epigenomic instability at CpG islands [6]. This layered modeling approach demonstrates how global epigenetic instability can erode cancer methylomes and expose them to localized methylation aberrations that drive transcriptional changes in tumors [6].
Liquid Biopsy Approaches and Circulating DNA
Liquid biopsies—particularly analyses of cfDNA and circulating tumor DNA (ctDNA) in blood—offer a minimally invasive alternative to tissue biopsies for cancer detection and monitoring [5] [4]. Tumor-derived material shed into various body fluids provides a reservoir of cancer-specific biomarkers that reflect the entire tumor burden and molecular heterogeneity [5]. DNA methylation biomarkers are especially advantageous in liquid biopsy applications due to the inherent stability of DNA methylation patterns, their cancer-specific nature, and the relative enrichment of methylated DNA fragments in cfDNA due to nuclease protection [5].
Different bodily fluids offer varying advantages depending on cancer type. For urological cancers like bladder cancer, urine demonstrates superior sensitivity compared to blood (87% vs 7% for TERT mutations) due to direct contact with tumors [5]. Similarly, bile outperforms plasma for biliary tract cancers, stool for colorectal cancer, and cerebrospinal fluid for brain tumors [5]. This principle of "local" liquid biopsy sources often provides higher biomarker concentration and reduced background noise compared to systemic blood collection [5].
Table 2: Clinically Implemented DNA Methylation Biomarker Tests
| Test Name | Cancer Type | Biosample | Biomarker(s) | Regulatory Status |
|---|---|---|---|---|
| Epi proColon | Colorectal | Blood/Plasma | SEPT9 methylation | FDA-approved [4] [2] |
| Cologuard | Colorectal | Stool | Multiple methylation markers | FDA-approved [7] |
| Bladder EpiCheck | Bladder | Urine | 15 methylation markers | CE-IVD marked [4] |
| AssureMDx | Bladder | Urine | TWIST1, ONECUT2, OTX1 methylation | Commercially available [4] |
| Galleri | Multi-cancer | Blood | Genome-wide methylation patterns | FDA Breakthrough Device [5] |
| Shield | Colorectal | Blood | Methylation markers | FDA-approved [5] |
The translation of methylation biomarkers into clinical practice demonstrates their utility across the cancer care continuum, from early detection and diagnosis to prognosis and treatment monitoring. However, despite the identification of thousands of potential methylation biomarkers in research settings, only a limited number have achieved regulatory approval and routine clinical implementation [4]. This disparity highlights the significant challenges in biomarker validation and clinical translation.
Experimental Workflows in Methylation Biomarker Development
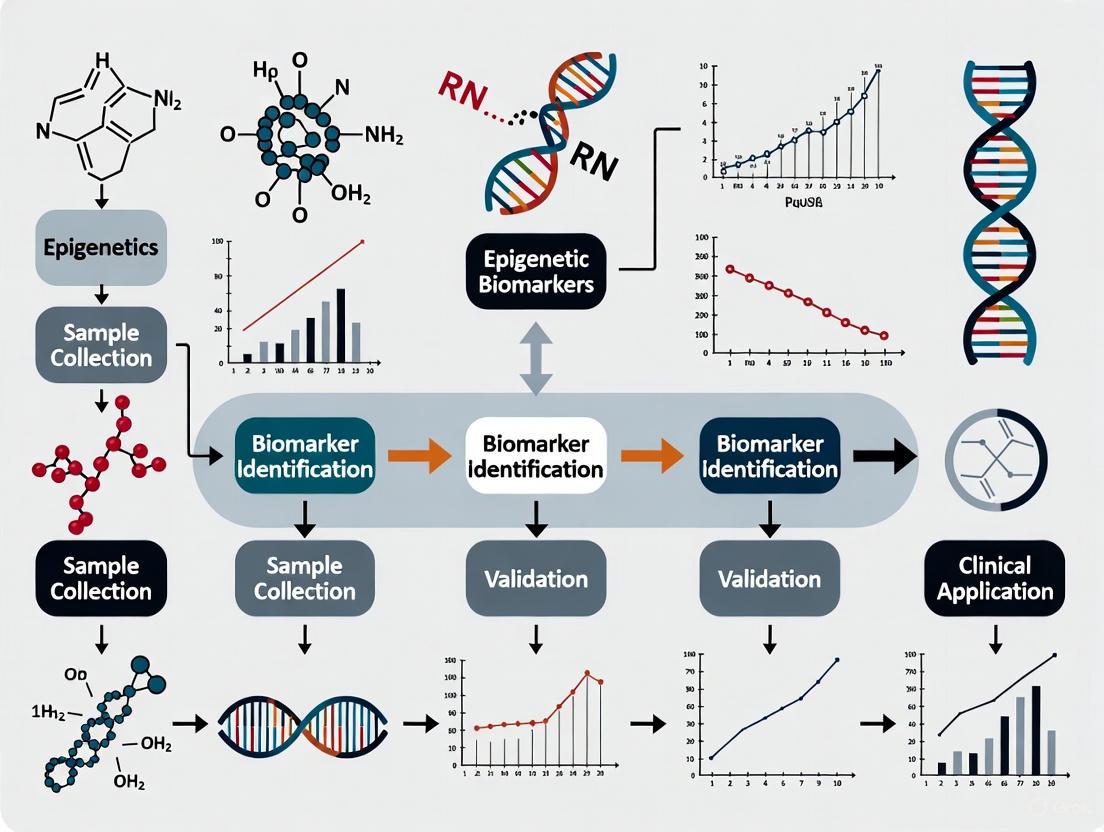
Biomarker Discovery and Validation Pipeline
The development of DNA methylation biomarkers follows a structured pipeline from discovery through clinical validation. Discovery phases typically utilize genome-wide approaches like WGBS or RRBS on tissue samples to identify differentially methylated regions between tumor and normal samples [5] [6]. Subsequent validation employs targeted methods such as qMSP or pyrosequencing in larger patient cohorts and liquid biopsy samples [5] [7]. This stepwise approach ensures that only the most promising biomarkers advance to costly clinical validation studies.
The Methylayer computational framework exemplifies a sophisticated approach to analyzing complex tumor methylation data [6]. This semi-supervised strategy integrates gene expression, genetic, and clinical information to computationally account for confounders like tumor microenvironment effects before inferring global methylation trends and identifying candidate loci for epigenetic cis-regulation [6]. Such integrative approaches are essential for distinguishing driver epigenetic events from passenger alterations in cancer.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for DNA Methylation Studies
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| Bisulfite Conversion Kits | EZ DNA Methylation kits, MethylEdge | Chemical conversion of unmethylated cytosines to uracils while preserving methylated cytosines [5] |
| DNA Methyltransferases | DNMT1, DNMT3A, DNMT3B | Enzymatic methylation establishment and maintenance; targets for epidrug development [3] [1] |
| Methyl-Sensitive Restriction Enzymes | HpaII, NotI, SmaI | Detection of methylation status at specific recognition sites [2] |
| Methylated DNA Immunoprecipitation Reagents | MeDIP kits, Methylated DNA Capture kits | Enrichment of methylated DNA fragments using 5mC-specific antibodies [5] |
| PCR Reagents for Methylation Analysis | Methylation-specific PCR primers, HotStart Taq polymerases | Amplification and detection of methylation patterns at specific loci [5] [7] |
| Whole Genome Amplification Kits | REPLI-g, GenomePlex | Amplification of limited DNA samples while preserving methylation patterns [7] |
| DNA Integrity Assessment Kits | Genomic DNA Quality Assessment, DV200 metrics | Quality control for fragmented DNA from FFPE or liquid biopsy samples [7] |
| Methylation Standards | Fully methylated and unmethylated control DNA | Quantification standards and assay controls [7] [2] |
Clinical Translation and Future Perspectives
Challenges in Biomarker Translation
Despite the identification of numerous promising DNA methylation biomarkers, their translation into clinical practice faces several significant challenges. The pre-analytical factors including sample collection, processing, and storage conditions can significantly impact methylation measurements, particularly in liquid biopsies where ctDNA concentrations are low [5] [7]. Analytical validation requires demonstrating robust performance across multiple sites and populations, while clinical utility must be established through large-scale prospective studies showing improved patient outcomes [5] [4].
Additional barriers include the need for standardized protocols, demonstration of cost-effectiveness, and navigation of regulatory pathways [4]. Even successfully translated tests like the SEPT9 methylation assay for colorectal cancer screening face limitations; while it shows good sensitivity for cancer detection (pooled sensitivity 0.71), its performance for detecting precancerous lesions is suboptimal, leading to recommendations against its use in some screening guidelines [2]. These challenges underscore the considerable gap between biomarker discovery and clinical implementation.
Emerging Applications and Future Directions
Future applications of DNA methylation biomarkers extend beyond cancer detection to include prognosis, therapy selection, and disease monitoring. Multi-cancer early detection tests (MCEDs), such as Galleri, which leverage genome-wide methylation patterns in cfDNA, represent a promising approach for population-level cancer screening [5]. The stability of cancer-specific methylation patterns and their enrichment in cfDNA make them particularly suitable for detecting minimal residual disease and early recurrence [5] [4].
The integration of machine learning approaches with DNA methylation data enables the development of sophisticated prediction models. Recent research demonstrates that machine learning algorithms can effectively analyze DNA methylation arrays and epigenetic biomarker datasets to build risk assessment models for cancer and other diseases [8]. These computational approaches can optimize risk prediction by combining clinical features with epigenetic biomarkers, potentially enabling early disease screening and personalized intervention [8].
The evolving landscape of DNA methylation research continues to provide insights into cancer biology while offering practical tools for clinical management. As technologies advance and our understanding of epigenetic mechanisms deepens, DNA methylation biomarkers are poised to play an increasingly prominent role in precision oncology, potentially enabling earlier detection, more accurate prognosis, and personalized therapeutic approaches for cancer patients.
The pursuit of early cancer detection has traditionally focused on genetic mutations—alterations in the DNA sequence of oncogenes and tumor suppressor genes that drive carcinogenesis. While these mutational signatures provide crucial insights, they represent only one component of the molecular machinery driving cancer development. In recent years, epigenetic biomarkers have emerged as powerful alternatives and complements to traditional genetic markers, offering distinct advantages for early cancer detection, diagnosis, and prognosis [9].
Epigenetic modifications, defined as heritable changes in gene expression without alterations to the underlying DNA sequence, include DNA methylation, histone modifications, and non-coding RNA expression. These modifications serve as critical regulatory mechanisms that can be influenced by environmental factors, lifestyle, and aging, potentially providing a more dynamic view of cancer risk and progression [10] [9]. This review systematically compares epigenetic and genetic biomarkers in the context of early cancer detection, highlighting the technical advantages, clinical validity, and practical benefits of epigenetic markers through current experimental data and methodological protocols.
Comparative Advantages of Epigenetic Biomarkers
Epigenetic biomarkers present several distinct technical and biological advantages over traditional genetic mutation-based approaches for early cancer detection, as summarized in the table below.
Table 1: Comparative Analysis of Genetic versus Epigenetic Biomarkers for Early Cancer Detection
| Feature | Genetic Biomarkers | Epigenetic Biomarkers |
|---|---|---|
| Molecular Basis | Changes in DNA sequence (mutations, translocations, deletions) [9] | Reversible modifications without DNA sequence change (methylation, histone mods) [9] |
| Frequency in Cancer | Varies by cancer type; often require specific mutations | Highly frequent and widespread; hyper/hypomethylation common early event [9] [11] |
| Tissue Specificity | Limited; often shared across cancer types | High; tissue-specific methylation patterns enable origin determination [12] |
| Dynamic Range | Static once mutated | Dynamic; reflects changing microenvironment and disease progression [10] [13] |
| Sample Compatibility | Requires sufficient tumor DNA | Compatible with fragmented DNA in blood; stable in circulation [12] [13] |
| Technical Detection | Requires high coverage to find rare variants | Amenable to amplification; sensitive detection of rare cell populations [12] |
| Influence Factors | Primarily inherited or random mutations | Modifiable by environment, lifestyle, and therapeutics [9] [14] |
The tissue-specific nature of epigenetic patterns provides a particular advantage for cancer detection. Unlike genetic mutations which may be similar across different cancers, DNA methylation patterns are highly tissue-specific, potentially allowing not just cancer detection but also identification of the tissue of origin [12]. Furthermore, epigenetic changes are often more frequent than genetic mutations in early carcinogenesis, with promoter hypermethylation of tumor suppressor genes occurring commonly across cancer types [9] [11].
Experimental Validation: Methodologies and Data
DNA Methylation Biomarkers in Ovarian Cancer
A 2025 clinical validation study demonstrates the prognostic utility of DNA methylation biomarkers in relapsed ovarian cancer [13]. The researchers developed and validated PLAT-M8, an 8-CpG blood-based methylation signature linked to chemoresistance and overall survival.
Table 2: PLAT-M8 Methylation Signature Performance in Relapsed Ovarian Cancer
| Parameter | Class 1 Methylation | Class 2 Methylation |
|---|---|---|
| Overall Survival | Shorter survival (HR: 2.50, 95% CI: 1.64-3.79) [13] | Longer survival |
| Platinum Sensitivity | Platinum-resistant [13] | Platinum-sensitive [13] |
| Clinical Features | Older age (>75), advanced stage, residual disease [13] | Higher complete response rates (RECIST) [13] |
| Carboplatin Monotherapy | Poor prognosis (adj. HR: 9.69, 95% CI: 2.38-39.47) [13] | Better prognosis |
Experimental Protocol:
- Sample Collection: Whole blood samples collected from patients at first relapse
- Cohorts: BriTROC-1 (n=47), OV04 (n=57), plus additional validation sets
- DNA Processing: Extracted DNA subjected to bisulfite conversion
- Methylation Analysis: Bisulfite pyrosequencing to quantify DNA methylation at 8 identified CpG sites
- Statistical Analysis: Consensus clustering to determine DNA methylation classes; Cox regression to assess overall survival concerning clinicopathological characteristics [13]
RNA Modification Analysis for Colorectal Cancer Detection
A novel approach for early colorectal cancer detection utilizes RNA modification patterns in blood samples through LIME-seq (low-input multiple methylation sequencing), published in Nature Biotechnology in 2025 [12].
Table 3: LIME-seq Performance in Colorectal Cancer Detection
| Metric | Performance |
|---|---|
| Sample Type | Blood plasma (liquid biopsy) |
| Target Analytes | tRNA methylation patterns, microbiome-derived signals |
| Study Population | 27 colon cancer patients vs. 36 healthy controls |
| Key Finding | Noticeable methylation changes in tRNA between cancer and control groups [12] |
| Advantage | Captures host microbiota activity reflecting tumor microenvironment [12] |
Experimental Protocol:
- Sample Preparation: Cell-free RNA isolated from blood plasma
- Library Preparation: LIME-seq uses HIV reverse transcriptase to create cDNA from cell-free RNA, with RNA-cDNA ligation strategy to capture short RNA species typically lost in commercial kits
- Sequencing: Simultaneous detection of RNA modifications at nucleotide resolution across multiple RNA species
- Analysis: Evaluation of tRNA-derived methylation signals and microbial genome-derived signals; comparison of methylation patterns between cancer patients and healthy controls [12]
The following diagram illustrates the LIME-seq experimental workflow:
Machine Learning Approaches for Epigenetic Biomarker Analysis
A 2025 study in Frontiers in Public Health utilized machine learning to analyze the relationship between 30 epigenetic biomarkers and cancer risk, demonstrating the power of computational approaches for epigenetic biomarker analysis [8].
Experimental Protocol:
- Data Source: NHANES database DNA methylation arrays and epigenetic biomarker datasets
- Algorithms: Nine machine learning algorithms tested (AdaBoost, GBM, KNN, LightGBM, MLP, RF, SVM, XGBoost, Logistic Regression)
- Validation: 5-fold cross-validation with grid search for parameter optimization
- Performance Metrics: Accuracy, MCC, Sensitivity, Specificity, AUC, F1 Score
- Feature Analysis: SHAP values to determine biomarker contribution to predictive models [8]
The study found that epigenetic age acceleration was strongly associated with cancer risk, with gender and smoking-related epigenetic biomarkers (PACKYRSMort) among the top contributing features [8].
Technical and Implementation Advantages
Enhanced Sensitivity in Liquid Biopsies
Epigenetic biomarkers offer practical advantages in liquid biopsy applications due to their chemical stability and abundance in circulation. Cell-free DNA methylation patterns remain stable in blood plasma, enabling detection of cancer-specific signals even at low concentrations [12] [13]. This addresses a key limitation of ctDNA mutation detection, which suffers from low concentration and high fragmentation in early-stage cancers [15].
The following diagram illustrates how epigenetic signals provide enhanced detection capabilities in liquid biopsies:
Dynamic Monitoring and Intervention Response
Unlike static genetic mutations, epigenetic marks are reversible and dynamic, allowing for monitoring of disease progression and treatment response. Studies have shown that epigenetic profiles change following therapeutic interventions, as demonstrated in studies of ketamine treatment for MDD and PTSD where reductions in epigenetic age were observed following treatment [14]. This dynamic nature provides opportunities for monitoring therapeutic efficacy and disease recurrence.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Essential Research Tools for Epigenetic Cancer Biomarker Investigation
| Tool Category | Specific Products/Platforms | Research Application |
|---|---|---|
| Methylation Arrays | Illumina Infinium HumanMethylationEPIC 850k BeadChip [14] [8] | Genome-wide methylation profiling at ~850,000 CpG sites |
| Bisulfite Conversion | EZ DNA Methylation Kit (Zymo Research) [14] | Chemical conversion of unmethylated cytosines for methylation analysis |
| Data Analysis Tools | Minfi R package [14], ENmix [14] | Preprocessing, normalization, and analysis of methylation array data |
| Epigenetic Clocks | GrimAge, PhenoAge, OMICmAge, DunedinPACE [14] [8] | Assessment of biological age acceleration from methylation data |
| Single-Cell Epigenomics | Single-cell RNA-sequencing, single-nucleus RNA-sequencing [10] | Resolution of intra-tumor heterogeneity and cell-specific states |
| Machine Learning | Scikit-learn, XGBoost, SHAP analysis [8] | Predictive model development and biomarker contribution analysis |
Epigenetic biomarkers represent a transformative approach to early cancer detection, offering significant advantages over traditional genetic mutation-based markers. Their tissue specificity, frequency in early carcinogenesis, chemical stability in circulation, and dynamic nature provide powerful capabilities for detecting cancer at its most treatable stages. The experimental data and methodologies reviewed here demonstrate the robust clinical validity of epigenetic signatures across multiple cancer types, while highlighting the importance of standardized protocols and analytical frameworks. As the field advances, integration of multimodal epigenetic data with machine learning approaches will further enhance the sensitivity and specificity of epigenetic biomarkers, ultimately improving early cancer detection and patient outcomes.
The transformation of a normal cell into a cancerous one is driven not only by genetic mutations but also by profound epigenetic alterations. Among these, DNA methylation changes are fundamental, characterized by two seemingly paradoxical hallmarks: global genomic hypomethylation and locus-specific hypermethylation [16] [17]. These changes occur early in carcinogenesis and continue to evolve throughout tumor progression and metastasis [17]. Global hypomethylation, the first epigenetic abnormality identified in human tumors, primarily affects repetitive DNA sequences and can lead to genomic instability and oncogene activation [16] [2]. Conversely, locus-specific hypermethylation frequently targets CpG islands in promoter regions, resulting in the transcriptional silencing of critical tumor suppressor genes [18] [17]. This review will objectively compare the experimental frameworks used to validate epigenetic biomarkers born from these hallmarks, providing a guide for their application in early cancer detection.
Molecular Mechanisms and Functional Consequences
The Dual Phenomena of DNA Methylation in Cancer
The core methylation changes in cancer are orchestrated by the DNA methyltransferase (DNMT) family of enzymes. DNMT1 is primarily responsible for maintaining existing methylation patterns after DNA replication, while DNMT3A and DNMT3B perform de novo methylation, establishing new methylation patterns [2] [19]. In cancer, the dysregulation of these enzymes leads to a widespread disruption of the normal epigenome.
- Global Hypomethylation: This phenomenon is largely driven by a genome-wide loss of methylation, particularly in repetitive DNA sequences such as satellite DNAs, LINE-1 elements, and Alu repeats [16]. This loss of methylation can cause chromosomal instability, reactivation of transposable elements, and loss of genomic imprinting, all of which contribute to a cellular environment permissive for malignant transformation [16] [2]. For instance, hypomethylation of the juxtacentromeric satellite DNA has been significantly associated with tumor grade in ovarian carcinomas and serves as a marker for risk of relapse and overall survival [16].
- Locus-Specific Hypermethylation: In parallel, specific CpG islands that are normally unmethylated become hypermethylated. This aberrant methylation predominantly affects promoter regions of genes involved in critical cellular pathways, including tumor suppression, cell cycle regulation, DNA repair, and apoptosis [18] [17]. Well-documented examples include the hypermethylation of the MGMT promoter in gliomas, which predicts a better response to temozolomide therapy, and the silencing of MLH1 in a subset of colorectal cancers, leading to microsatellite instability [18].
Integrated Pathway of Epigenetic Dysregulation in Tumorigenesis
The following diagram synthesizes the core mechanisms and functional consequences of DNA methylation changes in cancer, illustrating how global hypomethylation and locus-specific hypermethylation collectively drive tumorigenesis.
Experimental Methodologies for Methylation Analysis
The validation of DNA methylation biomarkers relies on a diverse toolkit of laboratory techniques, each with specific strengths, resolutions, and applications. The choice of method depends on the experimental goal, required throughput, resolution, and the nature of the sample material (e.g., tissue, blood, urine) [20] [2].
Table 1: Comparison of Key DNA Methylation Detection Techniques
| Method Category | Specific Technique | Key Principle | Resolution | Throughput | Primary Application |
|---|---|---|---|---|---|
| High-Throughput Analysis | Whole-Genome Bisulfite Sequencing (WGBS) | Bisulfite conversion followed by whole-genome sequencing | Single-base | High | Discovery of novel methylation markers [20] [2] |
| Reduced Representation Bisulfite Sequencing (RRBS) | Bisulfite sequencing of CpG-rich regions selected by restriction enzyme digest | Single-base | Medium-High | Cost-effective methylation profiling [21] [2] | |
| Methylation Microarrays (e.g., EPIC) | Bisulfite-converted DNA hybridized to probe arrays | Single-CpG site | High | Large-scale epigenome-wide association studies (EWAS) [22] [23] | |
| Region-/Site-Specific Analysis | (Quantitative) Methylation-Specific PCR (qMSP) | PCR with primers specific for methylated vs. unmethylated sequences after bisulfite conversion | Locus-specific | Medium | Highly sensitive validation and clinical assays [18] [23] |
| Bisulfite Pyrosequencing | Bisulfite conversion followed by sequencing-by-synthesis | Single-base within a locus | Medium | Quantitative validation of CpG sites [18] [23] [2] | |
| Methylation-Sensitive High-Resolution Melting (MS-HRM) | Post-bisulfite PCR analysis based on DNA melting profile differences | Locus-specific | Medium | Screening and methylation level quantification [22] [23] | |
| Direct Methylation Analysis | Nanopore Sequencing | Direct detection of 5mC without bisulfite conversion as DNA passes through a protein nanopore | Single-base | High | Real-time analysis of long DNA fragments, avoids bisulfite bias [2] |
Advanced Workflow for Biomarker Validation in Liquid Biopsies
A significant challenge in clinical oncology is the non-invasive detection of cancer. Liquid biopsies, which analyze circulating tumor DNA (ctDNA) from blood plasma, present a promising solution but are complicated by the low abundance of ctDNA. The following workflow outlines a sophisticated approach for validating methylation biomarkers in such challenging samples, incorporating a novel classification algorithm to enhance detection sensitivity.
This workflow highlights the EpiClass algorithm, a method developed to improve biomarker performance in liquid biopsies. Unlike approaches that rely on the average methylation level across a locus, EpiClass analyzes the distribution of methylation densities on individual DNA molecules (epialleles). Cancer-derived ctDNA often contains molecules with high methylation density, whereas background methylation from normal cells tends to be more heterogeneous and lower. EpiClass identifies optimal thresholds in these distributions to classify samples with higher sensitivity and specificity, even when the tumor DNA is highly diluted [21].
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful development and validation of epigenetic biomarkers depend on a suite of specialized reagents and materials. The table below details key solutions used in the featured experiments and the broader field.
Table 2: Key Research Reagent Solutions for Epigenetic Biomarker Research
| Reagent / Material | Function / Description | Application Example |
|---|---|---|
| Bisulfite Conversion Kits (e.g., EZ DNA Methylation-Gold Kit) | Chemically converts unmethylated cytosines to uracils, while methylated cytosines remain unchanged. This is the foundational step for most methylation assays [22] [23]. | Essential for pre-processing DNA before qMSP, pyrosequencing, and sequencing-based methods [22]. |
| Methylation-Specific PCR (qMSP) Assays | Primer and probe sets designed to specifically amplify either the methylated or unmethylated version of a bisulfite-converted target sequence [23]. | Quantitative detection of hypermethylated biomarkers like MGMT or GSTP1 in clinical samples [18] [17]. |
| Control DNA (e.g., EpiTect Control DNA) | Pre-methylated and unmethylated DNA from human cell lines, used as standards for assay calibration and quality control [22]. | Included in MS-HRM and qMSP runs to create standard curves (e.g., 0%, 1%, 10%, 100% methylated) [22]. |
| Methylated DNA Immunoprecipitation (MeDIP) Kits | Uses an antibody against 5-methylcytosine to immunoprecipitate and enrich methylated DNA fragments from the genome [22]. | Enrichment for genome-wide methylation screening using microarrays or sequencing [22]. |
| Cell-free DNA (cfDNA) Extraction Kits | Specialized kits designed to isolate short-fragment, low-concentration cfDNA from blood plasma or other body fluids [21] [20]. | Preparation of template DNA for liquid biopsy-based methylation tests from patient plasma samples [21]. |
| Infinium Methylation BeadChips (e.g., EPIC array) | Microarray platforms that interrogate the methylation status of hundreds of thousands to over a million CpG sites across the genome [22] [23]. | Large-scale epigenome-wide association studies (EWAS) for biomarker discovery [22] [23]. |
Comparative Performance of Clinically Relevant Methylation Biomarkers
The ultimate test of an epigenetic biomarker is its performance in a clinical setting. The following table summarizes key validated biomarkers, their detection in various sample types, and their clinical utility for early detection and diagnosis.
Table 3: Performance and Application of DNA Methylation Biomarkers in Cancer
| Cancer Type | Key Methylation Biomarkers | Sample Type | Reported Performance | Clinical Utility |
|---|---|---|---|---|
| Colorectal Cancer (CRC) | SEPT9 [18] [2], SDC2 [20] | Blood (plasma), Stool [20] | Sensitivity: 71%, Specificity: 92% (for SEPT9 in a meta-analysis) [2] | Screening; blood-based SEPT9 test (Epi proColon) is FDA-approved [2]. |
| Glioblastoma | MGMT [18] | Tissue (FFPE) [18] | Predictive of response to temozolomide chemotherapy; combined with IDH1 status for prognosis [18]. | Predictive & Prognostic; standard of care testing [18]. |
| Lung Cancer | SHOX2, PTGER4 [20] [17] | Blood (plasma), Bronchoalveolar lavage fluid [20] | Able to discriminate between malignant and non-malignant lung disease in plasma [17]. | Diagnostic aid, particularly for indeterminate lung nodules [17]. |
| Prostate Cancer | GSTP1 [18] [23] | Tissue (FFPE), Urine [18] | Highly specific for prostate cancer detection in tissue [18]. | Diagnostic; helps distinguish cancer from benign prostate hyperplasia [18]. |
| Breast Cancer | Panel of 4 markers (e.g., TRDJ3, PLXNA4) [20] | Peripheral Blood Mononuclear Cells (PBMCs) [20] | Sensitivity: 93.2%, Specificity: 90.4% (for a 4-marker panel) [20]. | Early detection; demonstrates potential of blood-based immune cell methylation signatures [20]. |
| Ovarian Cancer | ZNF154 [21] | Blood (plasma) [21] | Sensitivity: 91.7%, Specificity: 100% (using EpiClass algorithm in a validation cohort) [21]. | Early detection; outperformed CA-125 in detecting etiologically diverse tumors [21]. |
The dual hallmarks of tumorigenesis—global hypomethylation and locus-specific hypermethylation—provide a rich source of biomarkers for cancer detection. The experimental data and methodologies compared in this guide demonstrate that the successful translation of these biomarkers, particularly for early detection, hinges on several factors: the choice of analytical method (with bisulfite-based techniques being the current standard), the biological sample (where liquid biopsies are gaining prominence), and the data analysis strategy (where algorithms like EpiClass show promise in enhancing signal detection in noisy samples) [21] [20] [2].
Future development will likely focus on multi-marker panels to improve sensitivity across heterogeneous cancer types and stages. Furthermore, the integration of methylation signatures with other molecular data (genetic, proteomic) using machine learning models presents a powerful path forward for developing the next generation of diagnostic tools [20] [17]. While challenges remain in standardizing assays and validating markers in large prospective screening populations, the existing body of work firmly establishes DNA methylation as a cornerstone of cancer biology with immense, and increasingly realized, clinical potential.
Epigenetic biomarkers, dynamic and reversible modifications that regulate gene expression without altering the DNA sequence itself, have emerged as powerful instruments in oncology [24]. Their ability to provide early indicators of malignant transformation, track disease progression, and predict therapeutic response positions them at the forefront of cancer precision medicine [25]. Unlike genetic mutations, epigenetic alterations are potentially reversible, offering unique therapeutic opportunities [24]. The analysis of these markers in liquid biopsies—through the detection of circulating tumor DNA (ctDNA) and other tumor-derived materials in blood or other biofluids—provides a minimally invasive window into the tumor's molecular landscape, enabling real-time monitoring and overcoming the limitations of traditional tissue biopsies [5] [25]. This guide provides a comparative evaluation of the three principal classes of epigenetic biomarkers—DNA methylation, histone modifications, and non-coding RNAs—focusing on their mechanisms, detection technologies, and validated clinical applications in cancer early detection.
DNA Methylation Biomarkers
DNA methylation, the covalent addition of a methyl group to the 5-carbon position of cytosine in CpG dinucleotides, is the most extensively characterized epigenetic mark in cancer [5] [25]. In cancer cells, typical patterns include global hypomethylation, which can lead to genomic instability, and promoter-specific hypermethylation of tumor suppressor genes, which silences their expression [5] [20]. These alterations often occur early in tumorigenesis and are highly stable, making them excellent biomarkers for early detection [5].
Key Methodologies and Workflows
A cornerstone technology for DNA methylation analysis is bisulfite sequencing. This method relies on the treatment of DNA with sodium bisulfite, which deaminates unmethylated cytosines to uracils, while methylated cytosines remain unchanged. Subsequent PCR amplification and sequencing allow for single-nucleotide resolution mapping of 5-methylcytosine (5mC) [24].
Figure 1: Bisulfite sequencing workflow for DNA methylation analysis.
The choice between untargeted and targeted approaches depends on the research goal. Whole-Genome Bisulfite Sequencing (WGBS) provides comprehensive, base-resolution methylome coverage but is resource-intensive and requires high sequencing depth [24]. Reduced Representation Bisulfite Sequencing (RRBS) offers a cost-effective alternative by using restriction enzymes to enrich for CpG-rich regions like promoters and CpG islands, making it suitable for large-cohort studies [24]. For clinical validation and diagnostic applications, targeted methods such as methylation-specific PCR (qMSP) and digital PCR (dPCR) are preferred due to their high sensitivity, specificity, and suitability for analyzing low-abundance ctDNA in liquid biopsies [5] [20].
Performance Data and Clinical Applications
DNA methylation biomarkers have been validated across numerous cancer types. The table below summarizes selected biomarkers and their performance in early cancer detection.
Table 1: DNA Methylation Biomarkers in Early Cancer Detection
| Cancer Type | Methylation Biomarkers | Sample Type | Detection Method | Performance Notes | References |
|---|---|---|---|---|---|
| Colorectal Cancer | SDC2, SEPT9 |
Plasma, Feces | Real-time PCR | SEPT9 test FDA-approved; high sensitivity and specificity for early-stage detection. |
[20] |
| Breast Cancer | Panel of 15 markers | ctDNA | WGBS, Targeted BS-seq | AUC of 0.971 in validation cohort. | [20] |
| Lung Cancer | SHOX2, RASSF1A |
Plasma, Bronchoalveolar Lavage | Methylight, NGS | Effective detection in liquid biopsies. | [20] |
| Bladder Cancer | CFTR, SALL3 |
Urine | Pyrosequencing | High sensitivity (87%) reported for urine-based mutation detection. | [5] [20] |
| Esophageal Cancer | Panel of 12 markers | Tissue | Microarray | AUC of 96.6% in TCGA data validation. | [20] |
Liquid biopsy source selection is critical for optimizing detection. While blood plasma is universally applicable, local biofluids can offer higher biomarker concentrations. For example, urine outperforms plasma for bladder cancer detection, and bile is superior for biliary tract cancers [5]. The inherent stability of DNA and the relative enrichment of methylated DNA fragments in cfDNA further enhance their utility in liquid biopsy settings [5].
Histone Modification Biomarkers
Histone modifications are post-translational alterations—including acetylation, methylation, phosphorylation, and ubiquitination—to histone proteins that regulate chromatin structure and gene accessibility [26] [27]. These modifications are established, interpreted, and removed by "writer," "reader," and "eraser" enzymes, respectively [27]. Aberrant histone modification patterns are a hallmark of cancer and can drive uncontrolled proliferation and therapy resistance [26].
Key Methodologies and Workflows
Chromatin Immunoprecipitation followed by sequencing (ChIP-seq) is a widely used method for mapping histone modifications genome-wide. It involves cross-linking proteins to DNA, immunoprecipitating the protein-DNA complexes with antibodies specific to a histone mark, and then sequencing the bound DNA fragments [24].
Mass spectrometry (MS)-based proteomics provides an unbiased, quantitative profile of histone post-translational modifications. This approach has been successfully applied to clinical FFPE and frozen tissues, revealing distinct epigenetic signatures associated with cancer subtypes and patient prognosis [26].
Figure 2: ChIP-seq workflow for histone modification profiling.
Performance Data and Clinical Applications
Histone modifications can serve as powerful diagnostic and prognostic biomarkers. A landmark multi-omics study of over 200 breast tumors identified a specific histone modification signature that distinguishes aggressive triple-negative breast cancers (TNBCs) from other subtypes [26]. This signature was characterized by an increase in H3K4 methylation (H3K4me1/me2) and a decrease in marks such as H3K27me3 and H4K20me3 [26]. Furthermore, high levels of H3K4me2 were mechanistically proven to sustain the expression of genes driving the TNBC phenotype, and inhibiting H3K4 methyltransferases reduced tumor growth in vivo, highlighting its potential as a therapeutic target [26].
Table 2: Experimentally Validated Histone Modification Associations in Cancer
| Histone Mark | Cancer Type | Experimental Method | Biological & Clinical Association | References |
|---|---|---|---|---|
| H3K4me2/me3 | Triple-Negative Breast Cancer (TNBC) | Mass Spectrometry, ChIP-seq, CRISPR-editing | Sustains expression of TNBC phenotype genes; associated with poor prognosis; inhibition reduces tumor growth. | [26] |
| H3K27me3 | Various Cancers | ChIP-seq, Immunohistochemistry | Polycomb-mediated gene silencing; target of EZH2 inhibitors. | [25] [27] |
| H4K16ac | Various Cancers | Mass Spectrometry | General hallmark of cancer; progressively decreases in breast cancer subtypes. | [26] |
| H4K20me3 | Various Cancers | Mass Spectrometry | Decreased in cancer; associated with genomic instability. | [26] |
The translation of histone modifications into clinical practice faces challenges, including tumor heterogeneity and the need for highly specific antibodies and complex data analysis [28]. However, their reversible nature makes them attractive therapeutic targets, with drugs like histone deacetylase (HDAC) inhibitors already in clinical use [27] [28].
Non-Coding RNA Biomarkers
Non-coding RNAs (ncRNAs) are functional RNA molecules that do not code for proteins. They are crucial regulators of gene expression at the epigenetic, transcriptional, and post-transcriptional levels [29] [30]. Key ncRNA classes include microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs), all of which are frequently dysregulated in cancer [31] [29].
Key Methodologies and Workflows
RNA sequencing (RNA-seq) is the primary discovery tool for profiling ncRNA expression. It allows for the simultaneous detection and quantification of all ncRNA classes without prior knowledge of sequences [24] [31]. For validation and clinical application, quantitative PCR (qPCR) is the gold standard due to its high sensitivity, specificity, and throughput [31]. Computational tools and machine learning are increasingly used to identify ncRNA signatures from high-throughput sequencing data [31].
Figure 3: Workflow for ncRNA biomarker discovery and validation.
Performance Data and Clinical Applications
ncRNAs are stable in biofluids and exhibit tissue- and cancer-specific expression patterns, making them excellent non-invasive biomarkers [31] [30]. Panels of ncRNAs often demonstrate high diagnostic accuracy.
Table 3: Validated Non-Coding RNA Biomarkers in Gastrointestinal and Breast Cancers
| ncRNA Class | Example Biomarkers | Cancer Type | Function & Clinical Utility | References |
|---|---|---|---|---|
| miRNA | miR-21, miR-92a |
Gastrointestinal, Breast | Oncogenic; promotes proliferation; diagnostic accuracy and poor prognosis. | [31] [30] |
| lncRNA | H19, MALAT1, HOTAIR |
Gastrointestinal, Breast, HNSCC | Regulates chromatin state, transcription; associated with metastasis and therapy resistance. | [31] [29] |
| circRNA | Various (e.g., circCCDC66) |
Various | Sponges miRNAs; regulates cytokine signaling and immune evasion in cancer. | [29] |
In gastrointestinal cancers, a panel including the lncRNAs H19, NEAT1, and MALAT1 and the miRNAs miR-21 and miR-92a has been consistently validated with excellent diagnostic accuracy and association with poor overall survival [31]. In breast cancer, ncRNA expression profiles differ significantly across molecular subtypes, offering potential for subtype classification and predicting response to therapy [30].
The Scientist's Toolkit: Essential Research Reagents and Solutions
The experimental protocols described rely on a suite of specialized reagents and tools. The following table details key solutions required for research in this field.
Table 4: Essential Research Reagent Solutions for Epigenetic Biomarker Studies
| Reagent / Solution | Primary Function | Key Considerations for Use |
|---|---|---|
| Sodium Bisulfite | Chemical conversion of unmethylated cytosine to uracil for DNA methylation analysis. | Optimized kits are essential to minimize DNA degradation and ensure complete conversion. |
| Methylation-Specific Antibodies | Immunoprecipitation of methylated DNA (MeDIP) or modified histones (ChIP). | Specificity and lot-to-lot consistency are critical for reproducibility in ChIP-seq and MeDIP-seq. |
| Histone Modification-Specific Antibodies | Detection and enrichment of specific histone PTMs (e.g., H3K4me3, H3K27ac) in ChIP assays. | Rigorous validation using known positive and negative controls is required for reliable results. |
| CRISPR/dCas9 Epigenetic Editors | Targeted alteration of epigenetic marks (e.g., dCas9-DNMT3A for methylation) for functional validation. | Used to establish causality between a specific epigenetic mark and gene expression or phenotype. |
| Cell-Free DNA Blood Collection Tubes | Stabilization of cfDNA in blood samples for liquid biopsy analysis. | Prevents genomic DNA contamination and degradation of cfDNA, which is critical for accurate quantification. |
| RNA Stabilization Reagents | Preservation of RNA integrity in liquid biopsies (e.g., plasma, urine) and tissues. | Prevents degradation of labile ncRNA molecules by RNases, ensuring accurate expression profiling. |
The three classes of epigenetic biomarkers offer complementary strengths. DNA methylation is the most technologically mature for clinical translation, with several FDA-approved or designated tests (e.g., Epi proColon, Shield) for cancer detection in liquid biopsies [5] [20]. Its stability and early emergence in tumorigenesis are key advantages. Histone modifications provide deep functional insights into the chromatin state of tumors and are promising therapeutic targets, though their clinical implementation is more complex due to technical challenges [26] [28]. Non-coding RNAs offer high sensitivity for detecting specific cancer types and subtypes from biofluids and are valuable for prognosis, but their regulatory networks are complex and require sophisticated computational analysis [31] [29] [30].
The future of epigenetic biomarkers lies in multi-omics integration. Combining data from DNA methylation, histone modifications, ncRNA profiling, and genetic alterations using artificial intelligence and machine learning will enable the identification of robust, multi-modal biomarker signatures [24] [27]. This integrated approach, particularly when applied to liquid biopsies, holds the greatest potential for achieving the ultimate goal of precision oncology: early, accurate, and dynamic detection of cancer to guide personalized therapeutic interventions.
Epigenetic marks, particularly DNA methylation and 5-hydroxymethylcytosine (5hmC), have emerged as powerful biomarkers in clinical cancer research. Their unique biochemical properties and stability in various sample types provide significant technical advantages for early detection, monitoring, and precision oncology. This guide objectively compares the performance of these epigenetic marks against traditional biomarkers and details the experimental methodologies harnessing their potential for clinical application.
Technical Advantages of Epigenetic Marks
Epigenetic modifications offer distinct stability and detectability profiles that make them superior to genetic alterations for many clinical applications.
Table 1: Comparative Analysis of Biomarker Stability and Detectability in Clinical Samples
| Biomarker Type | Stability in Clinical Samples | Primary Detection Methods | Key Technical Advantages | Limitations |
|---|---|---|---|---|
| DNA Methylation (5mC) | High stability in FFPE tissues, plasma, and cfDNA; withstands bisulfite conversion [32] [33] [34] | Bisulfite sequencing (RRBS, WGBS), MSP, pyrosequencing, microarrays [32] [35] | Cost-effective amplification; high sensitivity/specificity in FDA-approved tests; tissue- and cancer-type specific patterns [32] [35] | Bisulfite conversion can degrade DNA; requires specific adjustment for cell-type heterogeneity in EWAS [32] |
| 5-Hydroxymethylcytosine (5hmC) | Stable epigenomic mark; patterns established early in tumorigenesis and persist through progression [36] | 5hmC-enriched sequencing, hMeDIP-Seq [37] [36] | Associated with active gene regulation; enables high-accuracy tissue of origin prediction (85.2%) [36] | Requires specialized enrichment protocols; less established in clinical workflows [36] |
| Histone Modifications | Moderate; requires specific preservation for ChIP assays [37] | ChIP-Sequencing, ChIP-String [37] | Defines functional chromatin states; reveals combinatorial patterns [37] | Technically challenging for low-input samples; not yet feasible for liquid biopsy [37] |
| Genetic Mutations | Stable in ctDNA but often at very low frequency in early stages [35] [34] | Targeted NGS, ddPCR [35] [34] | Straightforward interpretation; well-established in clinical pipelines [35] | Can lack sensitivity for early-stage cancer detection due to low variant allele frequency [35] |
Experimental Protocols for Epigenetic Analysis
Robust and sensitive methodologies are critical for leveraging epigenetic marks in clinical samples. The following workflows are foundational to the field.
Cell-Free DNA Methylation Analysis for Early Cancer Detection
This protocol is designed for genome-scale methylation analysis of low-input cfDNA from blood plasma, enabling early cancer detection and tissue-of-origin identification [33].
Workflow Overview:
Detailed Steps:
- Sample Collection & Processing: Collect whole blood (2×10 mL) in cell-free DNA BCT Streck tubes. Maintain at 15–25°C and process within 72 hours. Centrifuge at 1,600 × g for 10 minutes, transfer plasma, and perform a second centrifugation at 16,000 × g for 10 minutes. Aliquot and store plasma at -80°C [36].
- cfDNA Isolation: Extract cfDNA from plasma, normalizing to a low input of 5-10 ng for library construction [33].
- Library Preparation & Bisulfite Conversion: Use cell-free Reduced Representation Bisulfite Sequencing (cfRRBS). This method is optimized for minimal input and generates an average of three million high-quality CpGs per sample. Treat DNA with sodium bisulfite, converting unmethylated cytosines to uracils while methylated cytosines remain unchanged [32] [33].
- Sequencing & Data Analysis: Perform high-throughput sequencing (e.g., Illumina platforms). Align sequences to a reference genome (e.g., GRCh38) using tools like BWA-MEM2. Analyze data through a bioinformatics pipeline for differential methylation and deep-learning-powered tissue deconvolution models to correlate findings with clinical data [33] [36].
Targeted Methylation Sequencing for Multi-Cancer Early Detection
This approach uses custom probe panels to enrich for specific cancer-related methylation regions, optimizing for high sensitivity and specificity in detecting multiple cancer types from a single blood sample [35] [38].
Workflow Overview:
Detailed Steps:
- Probe Design & Panel Construction: Synthesize a custom panel of capture probes targeting >100,000 distinct regions encompassing over a million methylation sites. This panel is designed to differentiate cancer-specific methylation patterns [38].
- Pre-Capture Bisulfite Conversion: Isolate cfDNA and treat with sodium bisulfite. This "pre-capture" method is preferred for low-abundance cfDNA as subsequent PCR amplification increases library complexity before hybridization, reducing input requirements [38].
- Target Enrichment & Sequencing: Hybridize the bisulfite-converted and amplified library with the custom probe panel. Wash off non-specifically bound fragments and sequence the captured targets on a high-throughput platform [38].
- Bioinformatic Analysis & Machine Learning: Use machine learning (ML) algorithms, such as convolutional neural networks (CNNs) or gradient boosting machines (GBMs), to analyze the sequenced methylation patterns. These models are trained to classify cancer status and predict the tissue of origin (TOO) with high accuracy [35].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of epigenetic clinical tests relies on a suite of specialized reagents and tools.
Table 2: Key Research Reagent Solutions for Epigenetic Analysis
| Reagent/Tool | Function | Application Example |
|---|---|---|
| Sodium Bisulfite | Chemically converts unmethylated cytosine to uracil, allowing for methylation status determination via sequencing or PCR [32] [34] | Foundational step in MSP, bisulfite pyrosequencing, RRBS, and WGBS [32] |
| Twist Targeted Methylation Panel | Large pool of biotinylated oligonucleotide probes designed to capture and enrich specific methylation regions of interest from a sequencing library [38] | Used in MCED tests (e.g., GRAIL's Galleri) to enrich for 100,000+ regions from plasma cfDNA [35] [38] |
| Anti-5hmC Antibody | Specifically binds to 5-hydroxymethylcytosine for immunoprecipitation-based (hMeDIP) enrichment of 5hmC-modified DNA fragments [37] [36] | Enabling 5hmC profiling in tumor tissues and cfDNA; used to identify stable cancer-specific 5hmC signatures [36] |
| DNA Methyltransferases (DNMTs) / HDAC Inhibitors | Small molecule inhibitors (e.g., DNMT inhibitors Azacitidine) that reverse aberrant epigenetic marks, used as epidrugs [34] [39] | Therapeutic application; also used in vitro to test functional role of observed epigenetic changes [37] |
| Illumina Infinium MethylationEPIC BeadChip | Microarray-based technology for profiling methylation status at >850,000 CpG sites across the genome [40] | Used in large-scale epigenome-wide association studies (EWAS) for biomarker discovery [32] [40] |
The intrinsic stability of epigenetic marks in diverse clinical samples, coupled with advanced detection methodologies, positions them as indispensable tools for modern cancer research and diagnostic development. DNA methylation and 5hmC offer a powerful combination for sensitive early detection and accurate tissue-of-origin localization, directly addressing the challenges of cancer heterogeneity and low analyte abundance. As the field progresses, the integration of these epigenetic biomarkers with machine learning and multi-omics approaches will continue to refine their clinical utility, paving the way for more effective, personalized cancer management strategies.
Advanced Methodologies for Epigenetic Biomarker Analysis and Application
DNA methylation is a fundamental epigenetic mechanism involving the addition of a methyl group to the 5-carbon position of cytosine, primarily at cytosine-phosphate-guanine (CpG) dinucleotides, forming 5-methylcytosine (5mC) [41] [20]. This modification regulates gene expression without altering the underlying DNA sequence and plays pivotal roles in genomic imprinting, X-chromosome inactivation, and cellular differentiation [41] [5]. In cancer, aberrant DNA methylation patterns emerge early in tumorigenesis and remain stable throughout tumor evolution, making them ideal biomarkers for early detection [20] [5]. These alterations typically manifest as genome-wide hypomethylation accompanied by hypermethylation of specific CpG-rich gene promoters, particularly those of tumor suppressor genes [5].
The transition from microarray-based technologies to next-generation sequencing (NGS) platforms has revolutionized DNA methylation profiling, providing unprecedented resolution and coverage for biomarker discovery [41] [42]. While microarrays offer a cost-effective solution for profiling predefined CpG sites, NGS methods enable comprehensive mapping of methylation patterns across the entire genome, including previously unexplored regions [41] [43]. This comparison guide objectively examines the performance characteristics, experimental requirements, and applications of current DNA methylation profiling technologies within the context of validating epigenetic biomarkers for early cancer detection.
Technology Landscape: A Comparative Analysis of Profiling Methods
Microarray-Based Approaches
Principle: DNA methylation arrays integrate bisulfite conversion with hybridization to oligonucleotide probes fixed on a chip, allowing detection at specific CpG sites [44] [45]. The Illumina Infinium MethylationEPIC BeadChip represents the current state-of-the-art, with the EPICv2 version covering over 935,000 CpG sites [44].
Performance Characteristics: EPIC arrays demonstrate high reproducibility between technical replicates and strong concordance with whole-genome bisulfite sequencing (WGBS) data [44]. However, they are limited to predefined CpG sites and favor CpG-rich regions like islands and promoters, potentially missing biologically significant methylation events in other genomic contexts [45].
Next-Generation Sequencing Approaches
Bisulfite Sequencing Methods: Whole-genome bisulfite sequencing (WGBS) represents the gold standard for base-resolution methylation profiling, providing comprehensive coverage of nearly every CpG site [43] [45]. Reduced representation bisulfite sequencing (RRBS) offers a more targeted approach, using restriction enzymes to focus on CpG-rich regions at a lower cost [45]. However, bisulfite treatment causes substantial DNA degradation and introduces sequencing biases due to reduced sequence complexity [43] [45].
Enzymatic Conversion Methods: Enzymatic methyl-sequencing (EM-seq) utilizes enzymatic conversion rather than harsh chemical treatment, better preserving DNA integrity while maintaining base resolution [43] [45]. Studies show EM-seq has high concordance with WGBS while causing less DNA damage, making it particularly suitable for low-input samples and formalin-fixed paraffin-embedded (FFPE) tissues [43].
Third-Generation Sequencing: Long-read technologies from Oxford Nanopore Technologies (ONT) and PacBio enable direct detection of DNA methylation on native DNA without conversion [43] [45]. These platforms excel at resolving methylation patterns in repetitive regions and enable phasing of methylation haplotypes, but traditionally require more DNA input and have higher error rates than short-read sequencing [45].
Affinity Enrichment Methods: Techniques like methylated DNA immunoprecipitation sequencing (MeDIP-seq) use antibodies or methyl-binding proteins to enrich methylated DNA fragments before sequencing [41] [45]. While cost-effective for genome-wide methylation trends, they provide lower resolution and are biased toward highly methylated regions [41] [45].
Table 1: Comparative Performance of DNA Methylation Profiling Technologies
| Technology | Resolution | CpGs Covered | DNA Input | Cost | Best For |
|---|---|---|---|---|---|
| EPIC Array | Single CpG | ~935,000 sites | Moderate | $ | Large cohort studies [44] [45] |
| WGBS | Single-base | >28 million CpGs | High | $$$$ | Comprehensive methylome [41] [43] |
| RRBS | Single-base | ~2 million CpGs | Low | $$ | CpG island-focused studies [45] |
| EM-seq | Single-base | Comparable to WGBS | Low | $$$ | Low-input/degraded samples [43] [45] |
| ONT | Single-base | Genome-wide | High | $$$ | Repetitive regions, haplotype phasing [43] [45] |
| MeDIP-seq | ~150 bp | ~23 million CpGs | Moderate | $ | Genome-wide methylation trends [41] [45] |
Table 2: Technical Comparison Across Profiling Platforms
| Parameter | EPIC Array | WGBS | EM-seq | ONT |
|---|---|---|---|---|
| DNA Degradation | Minimal | Substantial | Minimal | None |
| Base Resolution | Yes | Yes | Yes | Yes |
| Throughput | High | Medium | Medium | Medium |
| FFPE Compatibility | Good | Limited | Good | Limited |
| 5hmC Discrimination | No | No | Yes | Yes |
| Multiplexing Capacity | High | Medium | Medium | Low |
Analytical Performance in Cancer Research Context
Recent comparative studies evaluating DNA methylation detection approaches across human genome samples derived from tissue, cell lines, and whole blood provide critical performance data for technology selection [43]. EM-seq showed the highest concordance with WGBS, indicating strong reliability due to their similar sequencing chemistry [43]. While each method identified unique CpG sites, emphasizing their complementary nature, ONT sequencing captured certain loci uniquely and enabled methylation detection in challenging genomic regions that are difficult to assess with short-read technologies [43].
For cancer biomarker discovery, methylation arrays have demonstrated particular utility in developing classification models. A 2024 study comparing machine learning models for central nervous system tumor classification found that models trained on EPIC array data achieved accuracies above 95% in classifying tumor types, with neural network models maintaining performance until tumor purity fell below 50% [46]. This robustness to variable tumor purity is particularly valuable for clinical applications where sample quality may be compromised.
Experimental Protocols for Biomarker Validation
Discovery Phase Workflow
The initial discovery phase typically employs genome-wide approaches to identify differentially methylated regions (DMRs) associated with cancer states. A typical workflow involves:
Sample Preparation: Extract high-quality DNA from tumor tissues, blood, or other liquid biopsy sources. The recommended input for WGBS is 100ng-1μg, while EM-seq can work with lower inputs (10-100ng) [43] [45].
Library Preparation: For bisulfite-based methods, fragment DNA followed by bisulfite conversion using kits such as EZ DNA Methylation Kit (Zymo Research). For enzymatic methods, use EM-seq kits that employ TET2 and APOBEC enzymes for gentler conversion [43] [45].
Sequencing: Sequence on appropriate platforms - Illumina short-read sequencers for WGBS/RRBS/EM-seq, or Nanopore/PacBio instruments for long-read approaches. Recommended coverage is 20-30x for WGBS [45].
Bioinformatic Analysis: Process data using specialized tools - BISMARK [46] or BSMAP [47] for alignment, and tools like DMRcate for identifying differentially methylated regions [44].
Validation of Methylation Biomarkers
Following discovery, potential biomarkers require rigorous validation using targeted methods:
Targeted Bisulfite Sequencing (Target-BS): This approach enables high-precision validation of specific gene regions' DNA methylation status through ultra-high depth sequencing (several hundred to thousands of times coverage) [47]. Specific gene regions of less than 300 base pairs are selected, and primers specific for bisulfite-treated DNA are designed for amplification [47].
Methylation-Specific PCR Methods: Quantitative methylation-specific PCR (qMSP) and digital PCR (dPCR) offer highly sensitive, locus-specific analysis suitable for clinical validation [5]. These methods are particularly useful for liquid biopsy applications where target abundance is low [20] [5].
Functional Validation: For established biomarkers, functional validation through CRISPR-Cas9 targeted editing experiments can demonstrate causality. The CRISPR-dCas9 system can introduce or remove methylation modifications at specific DNA sequences by fusing dCas9 with methyltransferases (e.g., DNMT3A) or demethylases (e.g., TET1) [47]. Subsequent assessment of gene expression changes via RT-qPCR and Western blotting confirms the functional impact of methylation changes [47].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents for DNA Methylation Studies
| Reagent/Solution | Function | Application Examples |
|---|---|---|
| Sodium Bisulfite | Converts unmethylated cytosine to uracil | WGBS, RRBS, Targeted BS [47] [45] |
| EM-seq Kit | Enzymatic conversion of unmethylated cytosines | Gentle conversion preserving DNA integrity [43] [45] |
| EPIC BeadChip Array | Genome-wide methylation profiling at predefined sites | Large cohort studies, clinical classification [44] [46] |
| 5mC Antibodies | Immunoprecipitation of methylated DNA | MeDIP-seq, immunofluorescence [41] [47] |
| DNA Methyltransferase Inhibitors | Global methylation interference | Functional studies (e.g., 5-azacytidine) [47] |
| CRISPR-dCas9 Methylation Editors | Targeted methylation/demethylation | Functional validation of specific loci [47] |
The evolving landscape of DNA methylation profiling technologies offers researchers multiple pathways for cancer biomarker discovery and validation. Microarrays provide cost-effective solutions for large-scale screening studies, while NGS methods deliver comprehensive methylome mapping at base resolution. The emergence of enzymatic conversion methods and long-read sequencing addresses limitations of traditional bisulfite-based approaches, particularly for challenging sample types.
For research focused on validating epigenetic biomarkers for early cancer detection, a strategic approach combining discovery and validation technologies shows greatest promise. Genome-wide discovery using EPIC arrays or WGBS/EM-seq followed by targeted validation with highly sensitive methods like Target-BS or dPCR creates a robust framework for biomarker development. As the field advances, integration of machine learning approaches for analyzing methylation data will further enhance classification accuracy and clinical utility, ultimately improving early cancer detection capabilities.
Liquid biopsy represents a transformative, minimally invasive approach in oncology that enables the detection and analysis of tumor-derived material in body fluids [48] [49]. Unlike traditional tissue biopsies, which provide a limited snapshot of a single tumor region, liquid biopsies capture the entire tumor burden and reflect the molecular heterogeneity of cancer [5]. The concept is grounded in the knowledge that blood and other bodily secretions contain tumor cells, nucleic acids, cellular components, and metabolites [48]. Among the various analytes, circulating tumor DNA (ctDNA)—small fragments of DNA released by tumor cells into the bloodstream—has demonstrated particular clinical promise due to advancements in DNA analysis technologies [48] [49].
ctDNA carries tumor-specific characteristics, such as somatic mutations, methylation changes, and fragmentation patterns, which distinguish it from normal cell-free DNA (cfDNA) that originates from the physiological apoptosis of healthy cells [48] [49]. The half-life of ctDNA is short, estimated between 16 minutes and several hours, allowing it to provide a real-time snapshot of tumor burden and enabling dynamic monitoring of disease progression and treatment response [50] [49]. The analysis of ctDNA and its features has created new avenues for cancer diagnosis, early detection, prognosis prediction, and monitoring of treatment response across a wide spectrum of malignancies [48] [51] [49].
Analytical Methodologies for ctDNA Analysis
The detection of ctDNA requires highly sensitive techniques due to its low abundance in circulation, especially in early-stage cancers or low-shedding tumors [48] [49]. The analytical methods can be broadly categorized into those targeting genomic alterations and those exploiting epigenetic or fragmentomic features.
Mutation-Based Detection Methods
Polymerase chain reaction (PCR)-based methods, including digital droplet PCR (ddPCR) and BEAMing (beads, emulsion, amplification, magnetics), are targeted approaches ideal for detecting single or a few well-characterized mutations with high sensitivity and rapid turnaround times [48] [49]. They are particularly useful for monitoring known driver mutations in specific cancers, such as BRAF in melanoma, KRAS in lung and colorectal cancer, and ESR1 in breast cancer [48] [49].
Next-generation sequencing (NGS) methodologies enable a broader profiling of genomic alterations and include whole-exome sequencing (WES), whole-genome sequencing (WGS), and targeted approaches such as CAPP-Seq and TEC-Seq [48] [49]. These methods facilitate comprehensive assessment of numerous patient-specific genomic changes, providing a more detailed understanding of the disease, particularly in heterogeneous cancers with high genomic instability [49]. To overcome errors introduced during sequencing, methods incorporating unique molecular identifiers (UMIs) have been developed, such as Duplex Sequencing and the more recent CODEC method, which achieves 1000-fold higher accuracy than conventional NGS [49].
Epigenetic and Fragmentomic Approaches
Epigenetic modifications, particularly DNA methylation, have emerged as highly promising biomarkers for liquid biopsy [5]. DNA methylation involves the addition of a methyl group to cytosine bases at CpG dinucleotides and plays a crucial role in gene regulation [5]. In cancer, DNA methylation patterns are frequently altered, with tumors typically displaying both genome-wide hypomethylation and site-specific hypermethylation of CpG-rich gene promoters [5]. These alterations often occur early in tumorigenesis and remain stable throughout tumor evolution, making them ideal biomarkers [5].
Fragmentomics is another emerging field that analyzes the fragmentation patterns of cfDNA, including fragment sizes, end motifs, and nucleosome positioning [48] [52]. Cancer patients exhibit more diverse fragmentation patterns compared to healthy individuals, which can be leveraged to distinguish cancer-derived cfDNA [48]. The DELFI method, for example, uses a machine learning model incorporating genome-wide fragmentation profiles to detect cancer with high sensitivity [48].
Table 1: Comparison of Major ctDNA Analysis Technologies
| Method Category | Specific Technologies | Key Features | Best Applications | Limitations |
|---|---|---|---|---|
| PCR-Based | ddPCR, BEAMing | High sensitivity for known mutations, rapid turnaround, quantitative | Monitoring known mutations (e.g., EGFR, KRAS), tumor-informed MRD | Limited to a small number of predefined mutations |
| Next-Generation Sequencing | WES, WGS, CAPP-Seq, TEC-Seq | Broad genomic coverage, discovery of novel alterations, tumor-uninformed approaches possible | Comprehensive genomic profiling, identifying resistance mutations | Higher cost, longer turnaround, potential for sequencing artifacts |
| Methylation Analysis | Bisulfite sequencing (WGBS, RRBS), Microarrays, EM-seq | Stable, early cancer markers, tissue-of-origin identification | Early cancer detection, multi-cancer screening | Bisulfite conversion degrades DNA; requires sensitive detection |
| Fragmentomics | DELFI, NF profiling, end motif analysis | Does not require genetic alterations, provides insight into gene regulation | Early detection, differentiating cancer from benign conditions | Novel field, requires advanced bioinformatics |
Experimental Protocols for Key Applications
Protocol for Methylation-Based Detection in Breast Cancer
A 2025 study detailed a protocol for discovering and validating cfDNA methylation markers for breast cancer diagnosis and prognosis [53]. The workflow is summarized in the diagram below:
Sample Collection and Processing: The study utilized plasma samples from 201 breast cancer patients, 83 healthy donors, and 71 individuals with benign tumors [53]. Cell-free DNA was extracted from plasma following standard protocols, with quality control measures to ensure DNA integrity [53].
Marker Discovery and Assay Development: BC-specific methylation markers were identified using large-scale methylation datasets (850K and 450K arrays) [53]. The researchers identified 21 BC-specific methylated CpG sites that distinguished breast cancer from tumor-adjacent tissues with high diagnostic accuracy [53]. Multiplex digital droplet PCR (mddPCR) assays were developed to detect methylation at eight key markers in the cfDNA [53].
Validation and Functional Analysis: The diagnostic performance was evaluated using logistic regression models, achieving an area under the curve (AUC) of 0.856 for distinguishing BC from healthy controls and 0.742 for differentiating BC from benign tumors [53]. Notably, combining these methylation markers with mammography and ultrasound improved diagnostic performance (AUC=0.898) [53]. A prognostic model based on six methylation sites was associated with poor overall survival (HR=2.826) [53]. Functional validation through in vitro experiments demonstrated that FAM126A overexpression regulates malignant phenotypes in BC cells [53].
Protocol for Multi-Feature Analysis in Pancreatic Cancer
A 2025 multi-center study developed integrated models for early detection and prognosis of pancreatic cancer using multiple cfDNA features [52]. The experimental workflow is illustrated below:
Cohort Design and Sample Preparation: The study enrolled 975 individuals across multiple centers, divided into Training (n=432), Testing (n=267), and two External Validation cohorts (n=129 and n=139) [52]. The cohorts included patients with pancreatic cancer, pancreatic benign tumors, chronic pancreatitis, and healthy controls [52]. Plasma cfDNA was extracted and subjected to low-pass whole-genome sequencing [52].
Multi-Feature Analysis: Four types of cfDNA features were analyzed: fragmentation patterns, end motifs, nucleosome footprint (NF), and copy number alterations (CNA) [52]. Pancreatic cancer patients showed significantly shorter cfDNA fragments (median 175 bp) compared to non-cancer groups (median 182-186 bp) [52]. KEGG pathway analysis of NF data revealed enrichment in cancer-related pathways including hedgehog, VEGF, MAPK, and Wnt signaling [52].
Model Development and Validation: The least absolute shrinkage and selection operator (LASSO) was used to select predictive features [52]. A weighted diagnostic model (PCM score) and a prognostic evaluation model (PCP score) were developed [52]. The combined PCM model demonstrated superior performance across all cohorts, with AUCs of 0.979 in the Testing cohort and 0.992 and 0.986 in the External Validation cohorts [52]. For early-stage (I/II) disease, the model achieved an AUC of 0.994 compared to healthy controls [52].
Performance Comparison of Liquid Biopsy Approaches
The quantitative performance of various liquid biopsy approaches across different cancer types is summarized in the table below.
Table 2: Performance Metrics of Liquid Biopsy Approaches Across Cancer Types
| Cancer Type | Technology/Assay | Biomarker Type | Clinical Application | Performance Metrics | Study (Year) |
|---|---|---|---|---|---|
| Breast Cancer | Multiplex ddPCR | DNA Methylation (8 markers) | Diagnosis vs Healthy | AUC: 0.856 | [53] (2025) |
| Breast Cancer | Multiplex ddPCR | DNA Methylation (8 markers) | Diagnosis vs Benign | AUC: 0.742 | [53] (2025) |
| Breast Cancer | Methylation ddPCR + Imaging | Combined | Diagnosis vs Benign | AUC: 0.898 | [53] (2025) |
| Pancreatic Cancer | PCM Score (Combined) | Multi-feature | Early Detection | AUC: 0.979-0.992 | [52] (2025) |
| Pancreatic Cancer | PCM Score (Combined) | Multi-feature | Resectable (Stage I/II) Detection | AUC: 0.994 | [52] (2025) |
| Pancreatic Cancer | PCM Score (Combined) | Multi-feature vs PBT | Differentiation from Benign | AUC: 0.886 | [52] (2025) |
| Esophageal Cancer | Various (Meta-analysis) | ctDNA mutation | Prognosis (Post-neoadjuvant) | HR for PFS: 3.97 | [50] (2025) |
| Esophageal Cancer | Various (Meta-analysis) | ctDNA mutation | Prognosis (During follow-up) | HR for PFS: 5.42 | [50] (2025) |
| Multiple Cancers | DELFI | Fragmentomics | Early Detection | Sensitivity: 91% | [48] |
Clinical Utility in Different Disease Settings
Early Detection and Diagnosis: Multicancer early detection tests using blood-based methylation ctDNA assays continue to be of great interest, though a key limitation remains the limited sensitivity for detecting early-stage cancers due to very low ctDNA levels [54]. However, combining liquid biopsy markers with conventional imaging significantly improves diagnostic performance, as demonstrated in breast cancer where methylation markers combined with mammography and ultrasound achieved an AUC of 0.898 for differentiating malignant from benign tumors [53].
Minimal Residual Disease (MRD) and Prognosis: Detection of ctDNA after curative-intent therapy, termed molecular residual disease (MRD), is strongly associated with high risk of clinical relapse [54]. In esophageal cancer, a 2025 meta-analysis of 22 studies found that ctDNA detection at all time points was associated with poorer progression-free survival (PFS) and overall survival (OS), with the prognostic value increasing from baseline (PFS HR=1.64) to after neoadjuvant therapy (PFS HR=3.97) and during follow-up (PFS HR=5.42) [50]. ctDNA testing predicted clinical recurrence an average of 4.53 months earlier than conventional radiological imaging [50].
Treatment Monitoring in Advanced Disease: The SERENA-6 clinical trial, presented at ASCO 2025, demonstrated that switching therapies based on ctDNA findings has clinical utility in advanced breast cancer [54]. Patients with HR-positive/HER2-negative breast cancer who switched to camizestrant upon detection of ESR1 mutations in ctDNA without radiological progression showed improved progression-free survival and quality of life compared to those continuing aromatase inhibitors [54]. This represents the first registrational study demonstrating that switching therapies upon ctDNA findings has clinical utility [54].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Liquid Biopsy Research
| Category | Specific Reagents/Solutions | Function/Application | Examples/Notes |
|---|---|---|---|
| Sample Collection & Storage | Cell-free DNA BCT tubes | Stabilize nucleated blood cells and preserve cfDNA profile | Prevents genomic DNA contamination from white blood cell lysis [5] |
| Plasma preparation tubes | Enable plasma separation and storage | Critical for pre-analytical phase [5] | |
| DNA Extraction | cfDNA extraction kits | Isolation of high-quality cfDNA from plasma | Magnetic bead-based systems often preferred for low-concentration samples [53] [52] |
| Bisulfite Conversion | Bisulfite conversion kits | Chemical conversion of unmethylated cytosines to uracils | Key step for methylation analysis; newer kits minimize DNA degradation [5] |
| Library Preparation | Methylation-specific library prep kits | Preparation of sequencing libraries from bisulfite-converted DNA | Compatible with Illumina, Thermo Fisher platforms [53] |
| Unique Molecular Identifiers (UMIs) | Molecular barcodes for error correction and quantification | Essential for distinguishing true mutations from sequencing artifacts [49] | |
| Target Enrichment | Targeted methylation panels | Capture of cancer-specific methylated regions | Custom or commercial panels (e.g., for breast cancer) [53] |
| PCR Amplification | Methylation-specific PCR assays | Amplification of specific methylated regions | ddPCR provides absolute quantification for low-abundance targets [53] |
| Sequencing | Whole-genome bisulfite sequencing | Comprehensive methylation profiling | Covers ~90% of CpGs but requires high DNA input [5] |
| Enzymatic methyl-sequencing | Bisulfite-free methylation profiling | Better preserves DNA integrity [5] | |
| Bioinformatics | Methylation analysis pipelines | Processing and interpretation of methylation data | Tools for differential methylation analysis and visualization [53] [52] |
Current Challenges and Future Directions
Despite the promising advances in liquid biopsy technologies, several challenges remain for their widespread clinical implementation. There is still a lack of standardization in liquid biopsy sample collection and analysis, with unclear clinical and laboratory guidelines for optimal time points for sampling [48] [53]. The low abundance of ctDNA in early-stage disease and the potential confounding signals from patient comorbidities, particularly chronic inflammatory diseases, present additional hurdles [48].
The DYNAMIC-III clinical trial in stage III colon cancer raised important questions about the readiness of ctDNA to guide treatment decisions in early-stage disease [54]. While ctDNA detection was prognostic, treatment escalation strategies for ctDNA-positive patients did not improve recurrence-free survival, suggesting that current treatment modalities rather than the assay technology might be the limiting factor [54].
Future directions for the field include the development of more sensitive detection methods, standardization of pre-analytical and analytical processes, and the conduct of large-scale prospective clinical trials to validate clinical utility [5] [49]. Integration of artificial intelligence with multi-omics approaches holds particular promise for enhancing the diagnostic precision of liquid biopsy [55]. Emerging technologies such as chromatin accessibility analysis and advanced cfDNA fragmentation profiling may further refine diagnostic accuracy and therapeutic monitoring [55].
As the field progresses, the successful translation of ctDNA biomarkers into clinical practice will depend on collaborative efforts between researchers, clinicians, diagnostic companies, and regulatory bodies to establish robust validation frameworks and demonstrate tangible benefits for patient outcomes across the cancer care continuum.
Artificial Intelligence and Machine Learning in Methylation Pattern Recognition
The application of artificial intelligence (AI) and machine learning (ML) to DNA methylation analysis represents a transformative advancement in cancer diagnostics. DNA methylation, a stable epigenetic modification that regulates gene expression without altering the DNA sequence, provides an abundant source of biological information for distinguishing normal tissues from malignancies [20] [5]. The inherent stability of DNA methylation patterns, which often emerge early in tumorigenesis and remain consistent throughout tumor evolution, makes them ideal biomarkers for early cancer detection and classification [5]. Machine learning algorithms excel at deciphering the complex, high-dimensional patterns within methylation data, enabling researchers to develop sophisticated diagnostic and prognostic models with remarkable accuracy [56]. This integration of computational power with epigenetic science is particularly crucial in oncology, where precise early detection significantly impacts patient survival outcomes.
The validation of epigenetic biomarkers for cancer early detection research requires robust analytical frameworks that can handle the vast datasets generated by modern methylation profiling technologies. AI and ML approaches have demonstrated exceptional capabilities in this domain, from identifying subtle methylation signatures in liquid biopsies to classifying intricate brain tumor subtypes with precision surpassing traditional histopathological methods [57] [58]. As these computational methods continue to evolve, they are paving the way for the development of non-invasive diagnostic tests that can detect cancers at their most treatable stages, ultimately transforming the landscape of cancer screening and personalized medicine.
Performance Comparison of ML Approaches in Methylation Analysis
Quantitative Performance Metrics Across Model Architectures
Multiple studies have systematically compared the performance of various machine learning models applied to DNA methylation data for cancer classification. These evaluations consistently demonstrate that different algorithmic approaches offer distinct advantages in accuracy, robustness, and computational efficiency. The selection of an appropriate model depends on specific research objectives, dataset characteristics, and clinical requirements.
Table 1: Performance Comparison of ML Models for CNS Tumor Classification Based on Methylation Profiles
| Model Architecture | Classification Accuracy | F1-Score | Precision | Recall | Robustness to Low Tumor Purity |
|---|---|---|---|---|---|
| Neural Network (NNmod) | 99% | 0.99 | 98% | 98% | Maintains performance down to 50% tumor purity |
| Random Forest (RFmod) | 98% | 0.97 | 96% | 97% | Moderate performance degradation with decreasing purity |
| k-Nearest Neighbors (kNNmod) | 95% | 0.88 | 90% | 86% | Significant performance reduction with decreasing purity |
A comprehensive study comparing three machine learning models for central nervous system (CNS) tumor classification revealed that a neural network approach (NNmod) achieved superior performance across all metrics, with 99% accuracy for both class and family prediction [57]. The random forest model (RFmod) also demonstrated strong performance with 98% accuracy, while the k-nearest neighbors model (kNNmod) showed somewhat lower but still respectable performance at 95% accuracy [57]. Notably, the neural network model exhibited the greatest robustness to reduced tumor purity, maintaining high performance until tumor purity fell below 50%, a critical advantage for clinical applications where samples often contain mixed cell populations [57].
Specialized Applications and Model Performance
Beyond general classification tasks, ML models have been optimized for specific methylation analysis applications, including liquid biopsy detection and rare cancer subtype identification. The performance requirements for these specialized applications often differ from general tumor classification, emphasizing sensitivity for early detection or precise localization for tissue-of-origin determination.
Table 2: Performance of Integrated ML Models in Liquid Biopsy Applications
| Test Name | Cancer Type | Sensitivity | Specificity | Key Features | ML Approach |
|---|---|---|---|---|---|
| GutSeer | Gastrointestinal (multi-cancer) | 82.8% (all stages); 81.5% (early-stage) | 95.8% | Combines methylation + fragmentomics | Targeted bisulfite sequencing with integrated ML |
| Heidelberg Brain Tumor Classifier | CNS tumors | High accuracy across 100+ subtypes | High specificity | Explains genomic regions of various sizes | Random Forest with explainable AI (XAI) |
| epiCervix | Cervical cancer | 89.9% (invasive); 51-52% (CIN2+) | 94-98% | Haplotype-based methylation scoring | Next-generation sequencing with pattern recognition |
The GutSeer assay, designed for multi-gastrointestinal cancer detection, exemplifies the power of integrating multiple data modalities within an ML framework. By combining DNA methylation with fragmentomics features through targeted bisulfite sequencing, this approach achieved 82.8% sensitivity and 95.8% specificity in validation cohorts, demonstrating particularly strong performance for early-stage cancers (81.5% sensitivity) [59]. Similarly, in cervical cancer detection, a haplotype-based methylation profiling approach utilizing next-generation sequencing data achieved 89.9% sensitivity for invasive cancer at 94-98% specificity, significantly outperforming traditional median methylation scoring methods (78.0% sensitivity) [60].
Experimental Protocols and Methodological Frameworks
DNA Methylation Profiling Technologies and Workflows
The successful application of ML to methylation pattern recognition depends heavily on the quality and characteristics of the underlying data, which varies significantly across profiling technologies. Understanding these methodological differences is essential for interpreting model performance and selecting appropriate analytical approaches.
Figure 1: Experimental Workflow for ML-Based Methylation Analysis
The experimental workflow for ML-based methylation analysis begins with sample collection, which can include tissue biopsies, blood (for liquid biopsy), urine, or other bodily fluids [20] [5]. Following DNA extraction, the most critical step is bisulfite conversion, which treats DNA to convert unmethylated cytosines to uracils while leaving methylated cytosines unchanged, enabling subsequent discrimination of methylation status [20] [56]. For microarray-based approaches, such as the Illumina Infinium MethylationEPIC array, the converted DNA is hybridized to probes targeting specific CpG sites across the genome [61] [62]. For sequencing-based methods like whole-genome bisulfite sequencing (WGBS) or reduced representation bisulfite sequencing (RRBS), the converted DNA undergoes library preparation and high-throughput sequencing [20] [56]. Emerging technologies also include enzymatic methylation sequencing (EM-seq) and long-read sequencing platforms from Oxford Nanopore and PacBio, which enable methylation profiling without harsh bisulfite conversion, thereby better preserving DNA integrity [5] [56].
Machine Learning Model Development and Training Protocols
The development of ML models for methylation analysis follows rigorous computational protocols to ensure robust performance and generalizability. The process typically begins with data preprocessing and normalization to address technical variations and batch effects, which are particularly challenging in methylation data from different platforms or processing batches [56] [61]. For array-based data, this includes background correction, dye bias adjustment, and probe-type normalization, while sequencing-based data requires alignment to reference genomes, methylation calling, and coverage normalization [61] [62].
Feature selection represents a critical step in model development, as methylation datasets typically contain hundreds of thousands of CpG sites, but only a subset provides biologically relevant information for specific classification tasks. The Heidelberg brain tumor classifier, for instance, employed a random forest algorithm to identify the most informative 10,000 probes from an initial set of 428,799 probes for final model training [58]. Similarly, the GutSeer assay for gastrointestinal cancers utilized genome-wide methylome profiling to identify 1,656 markers specific to five major GI cancers before developing a targeted sequencing panel [59].
Model training strategies must account for class imbalances common in cancer datasets, often employing techniques such as stratified sampling, synthetic minority over-sampling, or customized loss functions [57]. Validation represents the final critical phase, requiring independent cohorts to assess real-world performance. The GUIDE study, for example, employed a rigorous three-phase approach with separate training, validation, and independent test cohorts totaling 3,318 participants to validate the GutSeer assay [59].
Explainable AI in Methylation-Based Cancer Diagnostics
As ML models become more complex, understanding their decision-making processes has emerged as a crucial requirement for clinical adoption. Explainable AI (XAI) approaches are being developed to interpret black-box models and identify the specific methylation patterns driving classifications, thereby building trust in automated diagnostics and generating biological insights.
Figure 2: Explainable AI Framework for Methylation Classification
Research on the Heidelberg brain tumor classifier has revealed that ML models utilize distinct genomic regions to distinguish between tumor types. For IDH-mutant gliomas, probes within CpG islands were predominantly used (52.0% of average probe usage), reflecting the CpG island methylator phenotype (CIMP) characteristic of these tumors [58]. In contrast, classification of pituitary adenomas (PITAD) and lipomatous neoplasms (LIPN) relied more heavily on probes in shelf and open sea regions (78.6% and 57.7%, respectively) [58]. This differential utilization of genomic regions according to functional annotation provides biological plausibility to model decisions and reveals insights into tumor biology.
The XAI framework also demonstrated that a relatively small subset of probes contributes the majority of classification power, with the top 10,000 probes (2.3% of all probes) accounting for 61.2% of total usage across all class combinations [58]. This genomic redundancy, where many genes can distinguish individual tumor classes, explains the robustness of the classifier and reveals potential targets for therapeutic investigation. Importantly, probe usage values showed high concordance with feature importance values calculated using the established SHAP (SHapley Additive exPlanations) approach, validating the robustness of the interpretation method [58].
Research Reagent Solutions and Essential Materials
The successful implementation of ML-driven methylation analysis requires specific laboratory reagents and computational resources. The selection of appropriate tools directly impacts data quality, analytical performance, and ultimately, the clinical utility of the resulting models.
Table 3: Essential Research Reagents and Computational Tools for Methylation Analysis
| Category | Specific Product/Tool | Application and Function | Considerations |
|---|---|---|---|
| Methylation Profiling Platforms | Illumina Infinium MethylationEPIC v2.0 Array | Genome-wide methylation profiling at ~935,000 CpG sites | Covers enhancers, open chromatin; GRCh38 annotation [61] |
| Targeted Bisulfite Sequencing Panels | Focused analysis of cancer-specific markers | Cost-effective for clinical applications; enables fragmentomics [59] | |
| Sample Processing Reagents | Streck cfDNA BCT Tubes | Blood collection for cell-free DNA stabilization | Preserves ctDNA integrity; reduces background [59] |
| Zymo EZ-96 DNA Methylation MagPrep Kit | Bisulfite conversion of DNA | High conversion efficiency; suitable for automation [60] | |
| QIAamp Circulating Nucleic Acid Kit | Cell-free DNA extraction from plasma | Optimized for low-concentration samples [59] | |
| Computational Tools | Bismark | Alignment and methylation calling from bisulfite sequencing | Handles various sequencing designs; accurate methylation extraction [60] [59] |
| SeSAMe | Preprocessing and analysis of methylation array data | Addresses array-specific artifacts; improves reproducibility [61] | |
| ML Frameworks | Random Forest | Classification based on methylation profiles | Interpretable; robust to noise; feature importance metrics [57] [58] |
| Neural Networks | Complex pattern recognition in methylation data | High accuracy; robust to low tumor purity [57] |
The selection between microarray and sequencing-based approaches represents a fundamental decision in methylation study design. Microarrays like the Illumina Infinium MethylationEPIC v2.0 offer a cost-effective solution for profiling large sample cohorts, with coverage focused on functionally relevant genomic regions [61]. However, sequencing-based approaches provide greater flexibility in genomic coverage, single-molecule resolution, and the ability to integrate multiple data types, such as fragmentomics in liquid biopsy applications [60] [59]. Recent advancements in targeted sequencing panels, such as the 1,656-marker panel used in the GutSeer assay, balance comprehensive coverage with practical efficiency and cost considerations for clinical implementation [59].
For liquid biopsy applications, specialized collection tubes and extraction kits are essential to maintain the integrity of circulating tumor DNA, which typically represents a small fraction of total cell-free DNA, particularly in early-stage cancers [5] [59]. The computational workflow requires specialized tools for processing bisulfite-converted sequencing data, with Bismark representing the widely adopted standard for alignment and methylation calling [60] [59]. For array-based data, packages like SeSAMe implement optimized preprocessing pipelines to address technical artifacts and ensure reproducible results [61].
The integration of artificial intelligence and machine learning with DNA methylation analysis has fundamentally advanced cancer diagnostics, enabling precise tumor classification, early detection through liquid biopsies, and biologically insightful explanations of model decisions. As detailed in this comparison, neural network architectures generally achieve superior accuracy and robustness to low tumor purity compared to traditional random forest approaches, though both demonstrate strong performance in methylation-based classification tasks [57]. The emerging paradigm of explainable AI provides critical insights into the biological mechanisms underlying model decisions, building essential trust for clinical adoption and revealing novel tumor biology [58].
Future advancements in this field will likely focus on several key areas: enhanced multi-modal integration combining methylation with fragmentomics, genetic alterations, and clinical data; development of more efficient targeted panels optimized for specific clinical applications; and continued refinement of explainable AI frameworks to illuminate the black box of complex models. As methylation-based ML tools continue to evolve and validate in prospective clinical trials, they hold immense promise for transforming cancer detection, monitoring, and ultimately, patient outcomes through earlier intervention and personalized treatment strategies.
The validation of epigenetic biomarkers, particularly DNA methylation patterns, represents a paradigm shift in multi-cancer early detection (MCED). Unlike genetic mutations, epigenetic modifications offer the advantage of tissue-specific patterns that can simultaneously detect cancer presence and predict its tissue of origin (TOO), also known as cancer signal origin (CSO). The integration of multiple biomarker classes—including DNA methylation, protein biomarkers, and fragmentomic patterns—has emerged as a powerful approach to enhance the sensitivity and specificity of MCED tests. This guide provides a comprehensive comparison of current MCED technologies, their performance characteristics, and the experimental protocols validating their clinical utility for researchers and drug development professionals focused on epigenetic biomarker validation.
MCED Technology Platforms: Comparative Performance Analysis
Performance Metrics Across Leading MCED Platforms
Table 1: Comparative Performance of Major MCED Tests
| Test Name | Company/Developer | Primary Biomarker Class | Sensitivity (All Cancers) | Specificity | TOO/CSO Prediction Accuracy | Detectable Cancer Types |
|---|---|---|---|---|---|---|
| Galleri | GRAIL, Inc. | Targeted DNA Methylation | 40.4% (Episode Sensitivity) [63] | 99.6% [63] | 92% [63] | >50 types [63] |
| OncoSeek | SeekIn | Protein Tumor Markers + AI | 58.4% [64] | 92.0% [64] | 70.6% (Overall Accuracy) [64] | 14 common types [64] |
| CancerSEEK | Exact Sciences | Protein Markers + DNA Mutations | 62% [65] | >99% [65] | Not Specified | 8 types [65] |
| Shield | Guardant Health | Genomic Mutations + Methylation + Fragmentomics | 83% (CRC only) [65] | Not Specified | Not Specified | Colorectal Cancer [65] |
| DELFI | Delfi Diagnostics | cfDNA Fragmentation Patterns | 73% [65] | 98% [65] | Not Specified | 7 types [65] |
| PanSeer | Singlera Genomics | DNA Methylation | 87.6% [65] | 96.1% [65] | Not Specified | 5 types [65] |
Cancer-Type Specific Detection Performance
Table 2: OncoSeek Test Sensitivity by Cancer Type (n=15,122 Participants)
| Cancer Type | Sensitivity | Cancer Type | Sensitivity |
|---|---|---|---|
| Bile Duct | 83.3% [64] | Lung | 66.1% [64] |
| Gallbladder | 81.8% [64] | Liver | 65.9% [64] |
| Endometrium | 80.0% [64] | Head and Neck | 59.1% [64] |
| Pancreas | 79.1% [64] | Stomach | 57.9% [64] |
| Cervix | 75.0% [64] | Colorectum | 51.8% [64] |
| Ovary | 74.5% [64] | Breast | 38.9% [64] |
Recent large-scale validation studies demonstrate the evolving landscape of MCED technologies. The OncoSeek test, which integrates seven protein tumor markers with artificial intelligence, achieved an area under the curve (AUC) of 0.829 across 15,122 participants from seven centers in three countries [64]. The Galleri test, which utilizes targeted methylation sequencing of cell-free DNA, demonstrated in the PATHFINDER 2 study (n=23,161) a cancer signal detection rate of 0.93% with a positive predictive value (PPV) of 61.6% when used in a screening population [63]. Notably, the test showed 73.7% episode sensitivity for the 12 cancers responsible for two-thirds of cancer deaths in the U.S. [63].
Analytical Methodologies: Experimental Protocols and Workflows
DNA Methylation Analysis Workflow
Figure 1: DNA Methylation Analysis Workflow for MCED Tests. This diagram illustrates the standardized protocol for processing samples and analyzing DNA methylation patterns in MCED testing, from sample collection through bioinformatic analysis.
Multi-Biomarker Integration Strategy
Figure 2: Multi-Biomarker Class Integration in MCED. This schematic illustrates how different biomarker classes are combined using machine learning algorithms to generate comprehensive cancer detection outputs.
Detailed Experimental Protocols
Targeted Methylation Sequencing (Galleri Protocol)
The Galleri test employs a targeted methylation sequencing approach that involves several critical steps. Cell-free DNA is extracted from plasma samples (recommended volume: 2×10 mL whole blood) collected in EDTA or citrate tubes [66]. Following extraction, bisulfite conversion is performed where unmethylated cytosine residues are converted to uracil while methylated cytosine residues remain unchanged [66]. Library preparation utilizes targeted amplification of approximately 100,000 informative methylation regions, followed by next-generation sequencing. Bioinformatic analysis employs machine learning algorithms trained on methylation patterns from known cancer and non-cancer samples to detect cancer signals and predict tissue of origin [67]. Validation studies demonstrate this method can detect over 50 cancer types with a specificity of 99.6% and CSO prediction accuracy of 92% [63].
Protein Biomarker Quantification (OncoSeek Protocol)
The OncoSeek methodology utilizes a multi-analyte protein biomarker approach. Seven selected protein tumor markers (PTMs) are quantified from blood samples using immunoassay platforms such as Roche Cobas e411/e601 or Bio-Rad Bio-Plex 200 [64]. The test incorporates individual clinical data (e.g., age, gender) with protein biomarker concentrations into an AI-based risk assessment model that calculates the probability of cancer. Validation studies across multiple centers demonstrated consistent performance with Pearson correlation coefficients of 0.99-1.00 between different laboratories and platforms [64]. This approach achieved 58.4% sensitivity at 92.0% specificity across 14 cancer types, with particularly high sensitivity for pancreatic (79.1%), ovarian (74.5%), and lung (66.1%) cancers [64].
Multi-Modal Integration (CancerSEEK/Shield Protocol)
The Shield test (Guardant Health) exemplifies integrated multi-analyte approach, combining genomic mutations, methylation patterns, and DNA fragmentation profiles for enhanced sensitivity [65]. Similarly, CancerSEEK simultaneously analyzes eight cancer-associated proteins and 16 cancer gene mutations, with the combination increasing test sensitivity from 43% to 69% compared to either biomarker class alone [65]. This integrated methodology requires sophisticated computational frameworks to weight and combine signals from different biomarker classes, optimizing sensitivity while maintaining high specificity.
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents for MCED Development
| Reagent/Material | Function | Technical Specifications | Example Applications |
|---|---|---|---|
| Cell-free DNA Blood Collection Tubes | Sample preservation | EDTA or citrate anticoagulant; prevents cfDNA degradation | Plasma separation for methylation analysis [66] |
| Bisulfite Conversion Kit | DNA modification | Converts unmethylated C to U; preserves methylated C | Pre-treatment for methylation-specific PCR or sequencing [66] |
| Methylation-Specific PCR Primers | Target amplification | Designed for converted DNA; targets CpG-rich regions | Amplification of cancer-specific methylation markers [66] |
| Targeted Methylation Panels | Library preparation | Captures 100,000+ informative CpG sites | Galleri test target enrichment [67] |
| Immunoassay Reagents | Protein quantification | Antibody-based detection of protein biomarkers | OncoSeek protein tumor marker panel [64] |
| Next-Generation Sequencing Kits | DNA sequencing | High-throughput sequencing of converted DNA | Methylation pattern analysis [66] |
| Bioinformatics Pipelines | Data analysis | Machine learning algorithms for pattern recognition | Cancer signal detection and TOO prediction [67] |
Validation Frameworks and Clinical Translation
Analytical Validation Standards
Robust validation of MCED tests requires rigorous assessment across multiple parameters. Sensitivity must be evaluated across cancer types and stages, with particular attention to early-stage (I/II) detection rates. The PATHFINDER 2 study reported that 53.5% of Galleri-detected cancers were stage I or II [63]. Specificity must be established in large cohorts without cancer, with leading tests achieving 92-99.6% specificity [64] [63]. Reproducibility across laboratories and platforms is essential, as demonstrated by OncoSeek showing Pearson correlation coefficients of 0.99-1.00 between different testing sites [64].
Clinical Validation Study Designs
Several validation study architectures have emerged for MCED evaluation. Case-control studies provide initial performance data but may overestimate real-world performance. Prospective blinded studies, like the OncoSeek evaluation in symptomatic patients (73.1% sensitivity, 90.6% specificity), better reflect clinical utility [64]. Large-scale interventional trials, such as PATHFINDER 2 (n=35,878), provide the highest level of evidence by evaluating MCED tests in actual screening populations with outcome follow-up [63]. Real-world evidence studies, including analysis of over 100,000 Galleri tests, complement clinical trials by providing performance data in diverse clinical practice settings [67].
The integration of multiple biomarker classes represents the most promising path forward for MCED development. Epigenetic biomarkers, particularly DNA methylation patterns, provide the foundation for cancer signal detection and tissue of origin prediction, while protein biomarkers and genomic alterations offer complementary information that enhances overall test performance. As validation studies increasingly move from retrospective case-control designs to large-scale prospective trials and real-world implementation, the analytical and clinical frameworks for evaluating these complex tests continue to mature. The ongoing challenge for researchers and drug development professionals lies in optimizing multi-modal biomarker integration while ensuring accessibility, affordability, and equitable implementation across diverse healthcare systems and populations.
The landscape of cancer detection is undergoing a transformative shift with the emergence of non-invasive biospecimen sources that offer viable alternatives to traditional tissue biopsies. Saliva, urine, and stool have gained significant attention as valuable sources of biomarkers that can be obtained through minimally invasive collection methods. These biospecimens contain a rich repertoire of molecular information, including epigenetic markers, transcriptomic signatures, and metabolic profiles that reflect underlying pathological states [68] [69]. The growing interest in these biospecimens is driven by their potential to revolutionize early cancer detection, enable population-level screening, and facilitate continuous monitoring of disease progression and treatment response.
Epigenetic biomarkers, particularly DNA methylation patterns, have emerged as promising targets for cancer detection in non-invasive biospecimens due to their stability, frequency in cancer development, and detectability even in precancerous lesions [70] [32]. The validation of epigenetic biomarkers from these novel biospecimen sources represents a critical frontier in cancer research, offering the potential for developing highly sensitive and specific diagnostic tests that can be implemented at scale. This comparison guide examines the current state of research, performance characteristics, and methodological considerations for utilizing saliva, urine, and stool in cancer detection, with particular emphasis on their application in epigenetic biomarker discovery and validation.
Comparative Analysis of Biospecimen Performance
The utility of saliva, urine, and stool varies significantly across cancer types, with each biospecimen offering distinct advantages and limitations based on the biological proximity to the cancer origin and the molecular markers they contain. The table below summarizes the key performance metrics of these biospecimens for detecting various cancers.
Table 1: Performance Comparison of Non-Invasive Biospecimens in Cancer Detection
| Cancer Type | Biospecimen | Key Biomarkers | Sensitivity (%) | Specificity (%) | AUC | References |
|---|---|---|---|---|---|---|
| Colorectal Cancer | Stool | DNA methylation (NDRG4, BMP3); Transcriptomics | 98.0 (NDRG4/BMP3) | 90.0 (NDRG4/BMP3) | 0.86 (Transcriptomics) | [69] [71] |
| Stool | FIT | ~75.0 | - | - | [71] | |
| Stool | mt-sDNA | 94.0 | - | - | [71] | |
| Prostate Cancer | Urine | TTC3, H4C5, EPCAM | 91.0 | 84.0 | 0.92 | [72] |
| Bladder Cancer | Urine | SEPT9 | 78.2 | 93.3 | - | [69] |
| Urine | SOX1, TJP2, MYOD, HOXA9 | 100.0 | 100.0 | - | [69] | |
| Breast Cancer | Saliva | Sialic Acid | 80.0 | 93.0 | - | [73] |
| Oral Cancer | Saliva | Sialic Acid | - | - | - | [73] |
| Renal Cancer (ccRCC) | Urine | VOCs | 86.0 | 92.0 | 0.94 | [74] |
Table 2: Analytical Comparison of Biospecimen Sources
| Characteristic | Saliva | Urine | Stool |
|---|---|---|---|
| Collection Ease | High (non-invasive, can be self-collected) | High (non-invasive, can be self-collected) | Moderate (requires specific collection kit) |
| Sample Stability | Moderate (rapid protein degradation) | High (stable metabolites and DNA) | Variable (requires preservatives) |
| Biomarker Types | Proteins, DNA, RNA, miRNAs, metabolites | Cell-free DNA, RNA, proteins, metabolites | Cell-free DNA, RNA, human cells, hemoglobin, microbiome |
| Primary Cancers Detected | Oral, breast, pancreatic, lung | Prostate, bladder, renal, kidney | Colorectal, gastric |
| Epigenetic Biomarker Examples | DNA methylation patterns | DNA methylation (SEPT9, GDF15/TMEFF2/VIM) | DNA methylation (SEPT9, VIM, NDRG4/BMP3) |
| Key Challenges | Rapid biomarker degradation, variable composition | Biomarker concentration variability | High bacterial content, complex sample processing |
Stool-Based Detection Methodologies
Epigenetic Biomarkers in Stool
Stool-based testing has emerged as a particularly valuable approach for detecting gastrointestinal cancers, with colorectal cancer (CRC) screening representing the most advanced application. The fecal immunochemical test (FIT), which detects hemoglobin, has been widely adopted but suffers from limited sensitivity and specificity, particularly for early-stage disease [75] [71]. Epigenetic biomarkers in stool, especially DNA methylation patterns, have shown superior performance characteristics. Promising methylation biomarkers for CRC include SEPT9 (78.2% sensitivity, 93.3% specificity), and the combination of NDRG4 and BMP3 (98% sensitivity, 90% specificity) [69]. These biomarkers can be detected in cell-free DNA or DNA from shed cells in stool samples, providing a molecular signature of malignant transformation.
The commercial landscape for stool-based epigenetic tests is evolving, with several options now available. ColoSure evaluates VIM (vimentin) methylation but carries a risk of false negative results [70]. Multitarget stool DNA (mt-sDNA) tests that combine epigenetic markers with other molecular alterations have demonstrated enhanced sensitivity (94%) compared to FIT alone (≈75%) [71]. These tests leverage the fact that tumors and precancerous lesions continuously shed cells and DNA into the intestinal lumen, allowing for the detection of cancer-specific epigenetic alterations without the need for invasive procedures.
Transcriptomic Analysis of Stool Samples
Beyond epigenetic markers, transcriptomic analysis of shed intestinal cells in stool represents a cutting-edge approach for CRC detection and characterization. A novel methodology combining microbial ribosomal RNA (rRNA) depletion with unique molecular identifier (UMI)-based RNA sequencing has enabled deep profiling of human mRNA from stool samples [71]. This technique addresses the primary challenge of stool transcriptomics—the high dominance of bacterial RNA—by using DNA probes targeting microbial rRNA sequences followed by RNase H treatment to selectively degrade bacterial rRNA, enriching human mRNA for sequencing.
The workflow for stool transcriptomic analysis involves: (1) home-based self-collection of stool samples preserved in RNAlater; (2) total RNA extraction; (3) microbial rRNA depletion; (4) poly(A)-capture and UMI-based RNA sequencing; and (5) bioinformatic analysis to quantify gene expression [71]. This approach has demonstrated remarkable accuracy in distinguishing CRC from control samples (AUC = 0.86), with gene expression patterns in stool strongly correlating with matched tumor tissue signatures (r = 0.29, p < 5e−112) [71]. Notably, stool transcriptomes revert to control-like patterns after tumor resection, providing evidence that the signal originates from the tumor and has potential for monitoring treatment response.
Table 3: Key Research Reagents for Stool-Based Analyses
| Reagent/Kit | Function | Application Examples |
|---|---|---|
| RNAlater | RNA stabilizer for sample preservation | Stabilizes RNA in stool samples during home collection and transport [71] |
| Microbial rRNA Depletion Probes | DNA probes targeting bacterial rRNA sequences | Enriches human mRNA by removing abundant bacterial RNA [71] |
| RNase H | Enzyme that degrades RNA in RNA-DNA hybrids | Selective degradation of bacterial rRNA after probe hybridization [71] |
| Poly(A) Capture Beads | Isolate polyadenylated eukaryotic mRNA | Further enrichment of human transcripts after rRNA depletion [71] |
| UMI (Unique Molecular Identifier) Reagents | Barcodes for individual mRNA molecules | Enables accurate quantification and reduces sequencing artifacts [71] |
Diagram 1: Stool transcriptomics workflow for colorectal cancer detection
Urine-Based Detection Methodologies
Epigenetic Biomarkers in Urine
Urine has emerged as a particularly promising biospecimen for detecting urological cancers, with prostate cancer representing a key application area. Traditional prostate cancer screening relies on prostate-specific antigen (PSA) testing, but its limited specificity often leads to unnecessary biopsies [72]. Recent research has identified novel epigenetic biomarkers in urine that offer improved performance. A panel comprising TTC3 (tetratricopeptide repeat domain 3), H4C5 (H4 clustered histone 5), and EPCAM (epithelial cell adhesion molecule) has demonstrated exceptional accuracy in detecting prostate cancer (91% sensitivity, 84% specificity, AUC 0.92) [72]. This three-biomarker panel maintains diagnostic accuracy even in PSA-negative prostate cancer cases (85.7% in validation study) and effectively distinguishes prostate cancer from benign conditions like prostatitis and benign prostatic hyperplasia (AUC 0.89) [72].
For bladder cancer detection, urine-based epigenetic biomarkers have also shown considerable promise. The SEPT9 biomarker demonstrates 78.2% sensitivity and 93.3% specificity, while a multi-gene panel (SOX1, TJP2, MYOD, HOXA91, and HOXA92) has achieved perfect accuracy (100% sensitivity and specificity) in some studies [69]. Another promising panel for bladder cancer detection combines GDF15, TMEFF2, and VIM (92.5% sensitivity, 95.0% specificity) [69]. The commercial Bladder EpiCheck test, which uses an unspecified epigenetic panel, reports 73.1% sensitivity and 87.4% specificity [69]. These biomarkers can be detected in urine samples using techniques like quantitative methylation-specific PCR (qMSP) or bisulfite sequencing after extracting DNA from prostate cells shed in urine.
Metabolomic Approaches in Urine Analysis
Beyond epigenetic markers, urine metabolomics offers a complementary approach for cancer detection, particularly for renal cell carcinoma. A recent study identified 24 volatile organic compounds (VOCs) in urine that can distinguish clear cell renal cell carcinoma (ccRCC) from healthy controls with 86% sensitivity and 92% specificity (AUC 0.94) [74]. The analytical methodology for this approach utilizes stir-bar sorptive extraction coupled with thermal desorption gas chromatography/mass spectrometry (SBSE-TD-GC/MS), which efficiently captures and analyzes the VOC profile from urine samples [74].
The experimental protocol for urine-based metabolomic analysis includes: (1) collection of urine samples from ccRCC patients and healthy controls; (2) VOC extraction using stir-bar sorptive extraction; (3) thermal desorption of captured compounds; (4) separation and identification using GC/MS; (5) statistical analysis to identify discriminant VOC patterns; and (6) validation in independent cohorts [74]. This approach demonstrates the potential of urine as a source of metabolic biomarkers that reflect the underlying biochemical alterations associated with cancer progression.
Diagram 2: Urine analysis pathways for cancer detection
Saliva-Based Detection Methodologies
Biomarker Candidates in Saliva
Saliva contains a diverse array of biomolecules, including proteins, DNA, RNA, microRNAs, and metabolites, that can serve as biomarkers for both oral and systemic cancers [68]. Salivary sialic acid (SA) has emerged as a particularly promising biomarker for oral and breast cancers. Studies have demonstrated significantly elevated salivary SA levels in breast cancer patients (mean 14.9-18.5 mg/dL) compared to healthy individuals (mean 3.5-6.7 mg/dL), with one study reporting 80% sensitivity and 93% specificity for breast cancer detection [73]. For oral cancer, salivary SA levels show a dose-response relationship with disease progression, with mean levels increasing from 40.3 mg/dL in healthy controls to 57.5 mg/dL in precancerous lesions and 80.4 mg/dL in established oral cancer [73].
The collection of saliva offers numerous advantages for cancer screening, including non-invasiveness, ease of collection (can be self-administered), low cost, and minimal requirement for specialized equipment or personnel [68]. However, challenges remain in standardizing collection protocols and ensuring biomarker stability, as salivary proteins appear to degrade more quickly than serum proteins [68]. Proper preservation methods are crucial for maintaining sample integrity until analysis.
Advanced Detection Technologies for Salivary Biomarkers
Innovative detection technologies are being developed to enable point-of-care testing for salivary biomarkers. Portable Raman spectrometers show particular promise for sialic acid analysis, potentially enabling home-based cancer detection [73]. Surface-Enhanced Raman Scattering (SERS) offers a label-free, highly sensitive approach to sialic acid detection that provides a molecular fingerprint of the sample [73]. This technique relies on the inelastic scattering of photons and can be implemented in portable devices suitable for decentralized testing.
Biosensors represent another technological approach for salivary biomarker detection. These typically incorporate specific receptors or antibodies for target molecules and can be enhanced by nanomaterials like multiwalled carbon nanotubes or ferrocene to improve sensitivity [73]. Recent advances include the development of wearable sensors for sialic acid and miniaturized electrochemical sensors, though these technologies have been rarely employed in real samples of actual cancer patients [73]. The integration of these advanced detection platforms with salivary biomarkers holds significant potential for developing accessible, point-of-care cancer screening tools.
Table 4: Research Reagents for Saliva-Based Cancer Detection
| Reagent/Technology | Function | Application Examples |
|---|---|---|
| Saliva Collection Devices | Standardized saliva collection | Enables consistent sample collection for biomarker analysis |
| Raman Spectroscopy/SERS | Label-free molecular detection | Quantification of sialic acid levels in saliva [73] |
| Salivary Biosensors | Target molecule detection with receptors/antibodies | Sialic acid detection using carbon nanotubes/ferrocene [73] |
| Protein Stabilizers | Prevent degradation of salivary proteins | Maintains biomarker integrity during storage and transport [68] |
| High-Performance Liquid Chromatography | Separation and quantification of biomarkers | Traditional method for sialic acid quantification [73] |
Emerging Technologies and Innovative Approaches
PCR-Free Epigenetic Detection Methods
Conventional detection of epigenetic biomarkers typically relies on PCR-based methods following bisulfite conversion, but emerging technologies are exploring PCR-free approaches that could revolutionize point-of-care testing. An innovative organic biosensor based on Field-Effect Transistor (FET) technology has been developed for direct detection of DNA methylation biomarkers without PCR amplification [70]. This approach utilizes an Organic Charge-Modulated Field-Effect Transistor (OCMFET) structure that transduces the intrinsic negative charge of target DNA molecules captured by DNA probes anchored on the sensing surface.
The detection strategy for this PCR-free epigenetic biosensor involves converting epigenetic information (methylation patterns) into genetic information by exploiting the selective digestion of non-methylated regions. Specifically, the process includes: (1) DNA extraction from stool samples; (2) treatment with methylation-sensitive restriction enzymes that cleave unmethylated target sequences; (3) application of digested DNA to the OCMFET biosensor; (4) hybridization of intact (methylated) targets with specific probes on the sensing area; and (5) electronic detection of charge changes resulting from DNA hybridization [70]. This approach has successfully discriminated between methylated and unmethylated samples for colorectal cancer biomarkers SEPT9 and GRIA4, demonstrating concordance with standard MethyLight assays [70].
Integration with Wastewater-Based Epidemiology
An intriguing future direction for non-invasive cancer detection involves the application of wastewater-based epidemiology (WBE) to monitor population-level cancer incidence through epigenetic biomarkers [69]. This approach leverages the fact that epigenetic biomarkers associated with cancer are excreted in urine and feces and can be detected in wastewater systems. The SEPT9 biomarker and binary combinations like GDF15/TMEFF2/VIM, NDRG4/BMP3, and TWIST1/NID2 have been proposed as potential targets for future monitoring of multiple cancers from individual- to population-level scales using WBE [69].
This population-level approach could complement individual screening efforts by providing data on cancer incidence trends across different geographic regions and demographic groups. However, significant technical and ethical considerations must be addressed, including the sensitivity of detection methods for diluted biomarkers in complex wastewater matrices and the privacy implications of population-level cancer monitoring.
The validation of epigenetic biomarkers in non-invasive biospecimens represents a paradigm shift in cancer detection, offering the potential for widespread screening, early diagnosis, and improved patient outcomes. Saliva, urine, and stool each offer unique advantages and applications, with performance characteristics that continue to improve with advancing technologies. The integration of multiple biomarker types—epigenetic, transcriptomic, and metabolomic—within these biospecimens provides a comprehensive molecular portrait that may further enhance detection accuracy.
Future research directions should focus on standardizing collection and analysis protocols, validating biomarkers in diverse populations, and developing cost-effective point-of-care devices that can democratize cancer screening. The emergence of innovative detection technologies, such as PCR-free biosensors and portable spectroscopic devices, promises to make cancer screening more accessible and convenient. As these non-invasive approaches continue to mature, they have the potential to transform cancer detection from clinic-centered procedures to decentralized, population-wide screening programs that significantly reduce the global burden of cancer.
Epigenetic modifications represent a crucial layer of molecular regulation that can provide profound insights into cancer development and progression. Unlike genetic mutations, epigenetic alterations are reversible modifications that regulate gene expression without changing the underlying DNA sequence, making them promising targets for both biomarker development and therapeutic intervention [76]. In the context of cancer detection, DNA methylation has emerged as one of the most stable and clinically actionable epigenetic marks, with aberrant methylation patterns occurring early in carcinogenesis across virtually all cancer types [20]. These patterns can be detected in various sample types, including tumor tissue, blood, urine, and other bodily fluids, providing opportunities for minimally invasive cancer screening and monitoring.
The emergence of systems-epigenomics represents a paradigm shift in biomarker discovery, moving from reductionist approaches that focus on individual epigenetic marks toward network-based analyses that capture the complex regulatory relationships underlying cancer biology [77]. This approach recognizes that cancer is driven not by isolated molecular events but by dysregulated networks of interacting components, including genes, proteins, and epigenetic regulators. By integrating multi-omics data through advanced computational methods, systems-epigenomics aims to identify robust biomarker signatures with enhanced specificity for early cancer detection, ultimately addressing critical challenges such as tumor heterogeneity and the low abundance of tumor-derived signals in liquid biopsies [78] [79].
Comparative Analysis of Epigenomic Technologies
The analytical performance of epigenomic biomarker detection depends critically on the technological platform employed. Different methods offer distinct trade-offs in terms of resolution, throughput, sensitivity, and clinical applicability. Understanding these technical characteristics is essential for selecting appropriate platforms for biomarker development and validation.
Table 1: Performance Comparison of Major DNA Methylation Analysis Technologies
| Technology | Resolution | Sensitivity | DNA Input | Multiplexing Capacity | Clinical Applicability |
|---|---|---|---|---|---|
| Amplicon Bisulfite Sequencing | Single-base | High (≤1%) | Low (10-50 ng) | Moderate (10-100 targets) | High |
| Bisulfite Pyrosequencing | Single-base | High (≤5%) | Low (10-50 ng) | Low (single targets) | High |
| Methylation-Specific PCR | Regional | Moderate (1-5%) | Very Low (1-10 ng) | Low to moderate | High |
| Infinium MethylationEPIC | Single CpG (850,000 sites) | Moderate (1-5%) | Moderate (250-500 ng) | High (genome-wide) | Moderate |
| Whole-Genome Bisulfite Sequencing | Single-base (genome-wide) | High (≤1%) | High (50-100 ng) | Very high | Low (research) |
| Enrichment-Based Sequencing | Single-base (targeted) | High (≤1%) | Low (10-50 ng) | High (100-10,000 targets) | Moderate |
Data synthesized from community-wide benchmarking studies and technology reviews [20] [80].
Sensitivity and input requirements are particularly critical parameters for early cancer detection applications, where the abundance of tumor-derived DNA in circulation is often extremely low, especially in early-stage disease [78]. Liquid biopsy approaches for DNA methylation analysis must overcome the challenge that circulating tumor DNA (ctDNA) can represent less than 0.1% of total cell-free DNA in early-stage cancers, necessitating highly sensitive detection methods [79] [20]. Among profiling technologies, bisulfite sequencing-based methods generally provide the best combination of sensitivity and quantitative accuracy, with amplicon bisulfite sequencing and bisulfite pyrosequencing demonstrating particularly strong all-around performance in comparative assessments [80].
Table 2: Clinical Validity of Selected DNA Methylation Biomarkers for Early Cancer Detection
| Cancer Type | Methylation Biomarker | Sample Type | Sensitivity | Specificity | AUC |
|---|---|---|---|---|---|
| Colorectal Cancer | SDC2, SEPT9 | Plasma, Feces | 86.4-90% | 90.7-97% | 0.90-0.97 |
| Breast Cancer | TRDJ, PLXNA4, KLRD1, KLRK1 | PBMCs, Plasma | 93.2% | 90.4% | 0.971 |
| Lung Cancer | SHOX2, RASSF1A | Plasma, Bronchoalveolar Lavage | 74-89% | 88-96% | 0.85-0.92 |
| Liver Cancer | SEPT9, BMPR1A | Plasma | 82-91% | 87-94% | 0.89-0.93 |
| Esophageal Cancer | OTOP2, KCNA3 | Tissue, Plasma | 84-90% | 89-95% | 0.966 |
Data compiled from clinical validation studies of methylation biomarkers [20].
The clinical validity of DNA methylation biomarkers has been demonstrated across multiple cancer types, with many markers showing superior sensitivity and specificity compared to traditional protein biomarkers like CEA and CA19-9 [20]. For example, a prospective cohort study (ColonSecure) evaluating DNA methylation levels in circulating free DNA demonstrated 86.4% sensitivity and 90.7% specificity for detecting colorectal cancer, outperforming conventional serum markers [20]. Similarly, in breast cancer, a panel of four methylation biomarkers detected in peripheral blood mononuclear cells achieved 93.2% sensitivity and 90.4% specificity, substantially higher than mammography for certain populations [20].
Experimental Protocols for Epigenomic Biomarker Discovery
Sample Processing and DNA Extraction
Robust sample processing is fundamental to reliable epigenomic biomarker analysis. For liquid biopsy applications, blood samples should be collected in EDTA or specialized cell-free DNA tubes, with plasma separation preferably within 2-4 hours of collection to prevent leukocytic DNA contamination [76]. DNA extraction from plasma can be performed using commercial cell-free DNA kits, with typical yields of 3-15 ng/mL of plasma. For formalin-fixed paraffin-embedded (FFPE) tissues, specialized extraction protocols are required to address nucleic acid fragmentation and cross-linking. Magnetic bead-based extraction methods have demonstrated superior performance for FFPE samples, with optimized protocols enabling library construction from as little as 100 ng of total nucleic acids [76]. DNA quality and quantity should be assessed using fluorometric methods, with bisulfite conversion efficiency verified through control reactions.
Bisulfite Conversion Methods
Bisulfite conversion remains the gold standard for DNA methylation analysis, converting unmethylated cytosines to uracils while leaving methylated cytosines unchanged. The bisulfite conversion protocol typically involves denaturing DNA in alkaline conditions, followed by incubation with sodium bisulfite (3-5 hours at 64°C), desalting, and desulfonation in alkaline conditions [80]. Commercial bisulfite conversion kits have substantially improved reproducibility and DNA recovery, with conversion efficiencies typically >99% required for reliable quantification. For genome-wide analyses, the Infinium MethylationEPIC BeadChip platform provides coverage of approximately 850,000 CpG sites, with protocols following manufacturer specifications for amplification, hybridization, and scanning [80].
Targeted Methylation Analysis
For validation of candidate biomarkers, targeted approaches offer superior sensitivity and cost-effectiveness. Amplicon bisulfite sequencing involves PCR amplification of bisulfite-converted DNA using primers designed to avoid CpG sites, followed by next-generation sequencing (150-250x recommended coverage) [80]. Bisulfite pyrosequencing utilizes sequencing-by-synthesis to quantitatively determine methylation levels at individual CpG sites, with typical protocols involving PCR amplification followed by pyrosequencing on dedicated instrumentation [80]. For both methods, careful assay design is essential to account for bisulfite-induced sequence complexity, and inclusion of methylation standards (0%, 25%, 50%, 75%, 100% methylated) enables quantitative calibration.
Data Processing and Quality Control
Raw sequencing data requires specialized processing pipelines to account for bisulfite conversion. For bisulfite sequencing data, alignment tools such as Bismark or BS-Seeker2 map reads to reference genomes while accounting for C-to-T conversion. Methylation calls are typically extracted using a binomial statistical model, with filtering based on coverage depth (typically ≥10x) and base quality scores. For Infinium array data, preprocessing includes background correction, normalization, and probe-type correction using packages such as minfi or SeSAMe [81]. Quality control metrics should include bisulfite conversion efficiency, detection P-values, sample clustering, and sex chromosome concordance.
Network-Based Approaches for Enhanced Specificity
The integration of epigenomic data within network biology frameworks represents a powerful strategy to enhance the specificity of cancer biomarkers. Rather than considering individual methylation marks in isolation, network-based approaches analyze patterns of co-regulation and functional relationships to identify robust signatures that more accurately reflect the underlying biology of cancer [77].
Figure 1: Network-Based Biomarker Discovery Workflow
Network-based biomarker discovery typically begins with the construction of molecular interaction networks that integrate multiple data types, including DNA methylation, chromatin accessibility, histone modifications, and gene expression data [77]. Graph neural networks (GNNs) and related machine learning approaches can then analyze these networks to identify dysregulated modules and subnetworks that distinguish cancer states with higher specificity than individual markers [77]. For example, a network-based analysis of ovarian cancer cell lines successfully reduced approximately 65,000 gene features to a discriminative subset of 83 transcripts that robustly stratified molecular subtypes, revealing distinct biological programs including TP53-mutated serous-like and PI3K/AKT-activated clear cell-like subgroups [77].
The application of artificial intelligence methods further enhances network-based biomarker discovery by identifying hidden patterns in complex datasets that might escape conventional statistical approaches. AI-powered tools can integrate multi-omics data with clinical variables to generate predictive models that not only detect cancer but also provide information about tumor subtype, potential therapeutic vulnerabilities, and prognosis [79] [77]. For instance, explainable AI approaches have been used to predict prostate cancer progression in patients on active surveillance by integrating radiomic features from serial MRI scans with clinical variables like PSA density, achieving AUC values up to 0.917 [77].
The Scientist's Toolkit: Essential Research Reagents and Technologies
Successful implementation of systems-epigenomics approaches requires careful selection of reagents, technologies, and computational resources. The following toolkit summarizes essential components for network-based epigenomic biomarker discovery.
Table 3: Essential Research Reagents and Technologies for Systems-Epigenomics
| Category | Specific Products/Platforms | Key Applications | Performance Considerations |
|---|---|---|---|
| Bisulfite Conversion Kits | EZ DNA Methylation kits, Epitect Bisulfite kits | DNA methylation analysis | Conversion efficiency >99%, DNA recovery >80% |
| Methylation Arrays | Infinium MethylationEPIC, Illumina iScan | Genome-wide methylation profiling | 850,000 CpG sites, 3-5 μg DNA input |
| Targeted Enrichment | Agilent SureSelect, Illumina TruSeq, Twist Bioscience | Custom methylation panels | >10,000x enrichment, input ~50-100 ng |
| Bisulfite Sequencing | Illumina NovaSeq, PacBio Sequel, Oxford Nanopore | Single-base resolution methylation | Coverage >30x, PCR duplication control |
| Single-Cell Platforms | 10x Genomics Single Cell Multiome, Parse Biosciences | Cellular heterogeneity | Cell throughput >10,000, multi-modal capture |
| Computational Tools | Bismark, BS-Seeker, minfi, SeSAMe, MethylKit | Data processing and analysis | Support for spike-in controls, batch correction |
| Network Analysis | Cytoscape, Gephi, DeepGraph, STELLAR | Network visualization and analysis | Integration with pathway databases |
The selection of appropriate technologies should be guided by specific research questions and sample characteristics. For biomarker discovery phases, genome-wide approaches like the Infinium MethylationEPIC array or whole-genome bisulfite sequencing provide comprehensive coverage, though at higher cost and computational requirements [81] [80]. For clinical validation, targeted methods such as amplicon bisulfite sequencing or bisulfite pyrosequencing offer the sensitivity, reproducibility, and cost-effectiveness needed for large-scale studies [80]. Emerging technologies including single-cell epigenomics and long-read sequencing are resolving previously intractable challenges such as cellular heterogeneity and haplotype-specific methylation, further expanding the toolkit for precision cancer detection [82].
Systems-epigenomics represents a transformative approach to cancer biomarker discovery that leverages network biology and artificial intelligence to enhance the specificity and clinical utility of epigenetic biomarkers. By moving beyond single-marker analyses to consider coordinated patterns of epigenetic regulation, this paradigm addresses fundamental challenges in early cancer detection, including tumor heterogeneity, tissue-of-origin determination, and discrimination of indolent from aggressive malignancies. The integration of multi-omics data within network frameworks enables the identification of robust signatures that more accurately reflect the complex biology of cancer development and progression [77].
Future developments in this field will likely focus on several key areas. Multi-cancer early detection tests that analyze methylation patterns in circulating DNA are already showing promise in clinical trials, with tests like Galleri demonstrating the ability to detect over 50 cancer types from a single blood sample [79]. The incorporation of longitudinal sampling and treatment response monitoring will expand the clinical utility of epigenomic biomarkers beyond initial detection to encompass personalized surveillance and therapy selection [78] [79]. Additionally, the growing emphasis on accessibility and implementation in diverse healthcare settings will drive the development of simplified assay formats and point-of-care testing platforms that can democratize access to precision cancer detection [78]. As these technologies mature and validation studies demonstrate their clinical utility, systems-epigenomics approaches are poised to fundamentally transform cancer screening and early detection, ultimately reducing cancer mortality through earlier intervention and more personalized management strategies.
Overcoming Technical and Biological Challenges in Epigenetic Biomarker Development
Cell-type heterogeneity presents a significant challenge in the analysis of complex tissues, particularly in oncology research. Cellular deconvolution is a computational strategy that addresses this by inferring the relative proportions and, in some cases, the gene expression profiles of distinct cell types from bulk RNA-sequencing (RNA-seq) data [83]. This approach is especially valuable in the context of cancer research, where the tumor microenvironment consists of diverse cell populations—including malignant, immune, and stromal cells—that interact dynamically to influence disease progression and treatment response [84]. The ability to dissect this cellular complexity from bulk transcriptomic data enables researchers to extract meaningful biological signals that would otherwise be obscured in bulk analyses.
The importance of deconvolution has grown with the recognition that epigenetic biomarkers, such as DNA methylation patterns, are often cell-type-specific [18] [85] [17]. For early cancer detection, where liquid biopsies contain scarce amounts of circulating tumor DNA (ctDNA), understanding the cellular origin of these epigenetic signals is paramount [85] [17]. Deconvolution algorithms provide the analytical framework necessary to interpret these complex biomarker patterns within heterogeneous clinical samples, thereby enhancing the sensitivity and specificity of cancer diagnostics [85].
Performance Benchmarking of Deconvolution Algorithms
Key Performance Metrics
Evaluating deconvolution methods requires specialized metrics that quantify how well estimated cell proportions match ground truth measurements. The most commonly used metrics in benchmarking studies include:
- Root Mean Square Error (RMSE): Measures the average magnitude of estimation errors, with lower values indicating better performance [86] [87].
- Pearson's Correlation Coefficient (r): Quantifies the linear relationship between estimated and true proportions, with values closer to 1.0 representing stronger agreement [84] [87].
- Mean Absolute Deviation (MAD): Represents the average absolute difference between predicted and actual values [87].
- Spearman's Correlation: Assesses monotonic relationships (not necessarily linear) between estimates and ground truth [86].
These metrics are typically calculated for each cell type individually to identify algorithm strengths and weaknesses across different cellular populations.
Comparative Performance Across Multiple Studies
Recent large-scale benchmarking efforts have evaluated numerous deconvolution algorithms across various tissue types and experimental conditions. The table below synthesizes performance findings from multiple independent studies:
Table 1: Performance Comparison of Deconvolution Algorithms Across Benchmarking Studies
| Algorithm | Study Reference | Performance Summary | Best Performing Cell Types | Notable Limitations |
|---|---|---|---|---|
| Bisque | Genome Biology (2025) [83] | Most accurate for snRNA-seq reference data | Broad cell types in brain tissue | - |
| hspe (dtangle) | Genome Biology (2025) [83]; Sci. Adv. (2024) [86] | Among most accurate for proportion estimation; Best for cell proportions in ROSMAP data | Major cell populations | Performance decreases for rare cell types (<5% abundance) |
| bMIND | Science Advances (2024) [86] | Best for estimating sample-wise cell-type gene expressions | Multiple brain cell types | Requires appropriate reference data |
| MuSiC | Science Advances (2024) [86] | Lower performance despite scRNA-seq design | - | Underperforms in real bulk tissue data |
| CIBERSORTx | Nature Comm. (2024) [84] | Good performance for coarse-grained populations | Immune cell types in tumor microenvironment | Lower accuracy for fine-grained subpopulations |
| DWLS | Genome Biology (2025) [83] | Moderate performance | - | - |
| BayesPrism | Genome Biology (2025) [83] | Moderate performance | - | - |
These comparative analyses reveal that algorithm performance varies significantly depending on the tissue context, cell type abundance, and resolution required. Methods like Bisque and hspe/dtangle consistently demonstrate strong performance for estimating broad cell type proportions, while bMIND excels at reconstructing cell-type-specific gene expression patterns [83] [86]. The DREAM Challenge evaluation further highlighted that while most methods perform well for coarse-grained cell types, fine-grained subpopulations (particularly CD4+ T cell functional states) remain challenging across all algorithms [84].
Experimental Protocols for Method Validation
Orthogonal Validation Using Multi-Assay Datasets
Rigorous validation of deconvolution algorithms requires comparison against orthogonal measurements of cell type proportions. The following workflow illustrates a comprehensive validation approach using matched multi-modal data:
Diagram 1: Multi-Assay Validation Workflow. This experimental design uses orthogonal RNAScope/IF measurements from matched tissue sections as ground truth for validating deconvolution algorithms [83].
The protocol involves several critical steps:
Tissue Processing: Adjacent sections are taken from the same tissue block (e.g., human dorsolateral prefrontal cortex) to ensure cellular composition remains comparable across assays [83].
Multi-Modal Data Generation:
- Bulk RNA-seq: Performed using different RNA extraction protocols (total, nuclear, cytoplasmic) and library preparation methods (polyA+, RiboZeroGold) to assess protocol effects [83].
- Reference snRNA-seq: Generated from the same tissue blocks to capture cell-type-specific expression profiles [83] [86].
- Orthogonal Validation Data: RNAScope/IF (RNA in situ hybridization combined with immunofluorescence) provides direct measurement of cell type proportions through molecular labeling of specific cell markers [83].
Algorithm Application & Validation: Deconvolution methods estimate cell proportions from bulk RNA-seq data using snRNA-seq as reference, with results compared against RNAScope/IF measurements using statistical metrics like RMSE and correlation coefficients [83] [86].
This multi-assay approach provides a "silver standard" for validation, overcoming limitations of pseudobulk simulations that may not fully capture the technical and biological complexities of real bulk tissue data [83] [86].
In Vitro Admixture Experiments for Controlled Validation
For tumor microenvironment applications, controlled in vitro admixture experiments provide an alternative validation strategy:
Cell Purification: Immune cells are isolated from healthy donors, while stromal, endothelial, and cancer cells are obtained from cell lines [84].
Controlled Mixing: Cells are combined in predefined proportions representative of solid tumors, with variations across different cancer types (e.g., breast vs. colon cancer) and biological distributions [84].
RNA Extraction and Sequencing: RNA is extracted from the admixtures and subjected to bulk RNA-seq [84].
Performance Assessment: Deconvolution predictions are compared against the known mixing proportions to calculate accuracy metrics [84].
This approach provides exact ground truth but may not fully replicate the biological complexity of actual tumor samples, where cell-type-specific gene expression patterns may differ from purified cells [84].
Research Reagent Solutions for Deconvolution Studies
Successful implementation of deconvolution algorithms requires appropriate research reagents and computational resources. The following table outlines essential materials and their functions:
Table 2: Essential Research Reagents and Computational Tools for Deconvolution Studies
| Category | Specific Tool/Reagent | Function/Application | Considerations |
|---|---|---|---|
| Reference Data | snRNA-seq from matched tissue [83] | Gold-standard reference for deconvolution | Requires fresh frozen tissue; computationally intensive |
| Purified cell type expression profiles [84] | In vitro validation of algorithm performance | May not capture in vivo gene expression states | |
| Validation Technologies | RNAScope/IF [83] | Orthogonal measurement of cell type proportions | Requires tissue sections; expertise in imaging |
| IHC/Immunofluorescence [86] | Protein-level validation of major cell types | Limited multiplexing capability | |
| Bulk RNA-seq Protocols | PolyA+ enrichment [83] | mRNA profiling with higher exonic mapping rate | May miss non-polyadenylated transcripts |
| RiboZeroGold rRNA depletion [83] | Total RNA profiling with higher intronic mapping | Captures more diverse gene biotypes | |
| Computational Tools | DeconvoBuddies R/Bioconductor package [83] | Implements Mean Ratio marker selection and provides datasets | Requires R programming knowledge |
| Marker gene sets (Mean Ratio method) [83] | Identifies cell-type-specific genes with minimal off-target expression | Performance varies by tissue type |
Applications in Epigenetic Biomarker Validation for Cancer Detection
Deconvolution algorithms play a crucial role in validating and interpreting epigenetic biomarkers for early cancer detection. The following applications are particularly relevant:
Cell-Type-Specific Methylation Signatures
DNA methylation patterns are highly cell-type-specific, complicating the interpretation of bulk tissue or liquid biopsy measurements [18] [17]. Deconvolution addresses this challenge by:
- Identifying Cellular Origins: Linking aberrant methylation patterns to specific cell populations within heterogeneous samples [85] [17].
- Improving Sensitivity: Enabling detection of rare cell populations (e.g., circulating tumor cells) by accounting for background signals from major cell types [85].
- Enabling Tissue-of-Origin Determination: Methylation profiles deconvoluted from liquid biopsies can hint at the anatomical origin of tumors, which is crucial for early detection strategies [85].
Biomarker Discovery in Complex Tissues
In solid tumors, deconvolution facilitates the discovery of cell-type-specific epigenetic alterations:
- Differentiating Driver from Passenger Events: By associating methylation changes with specific cell types, researchers can prioritize events likely to have functional consequences [18] [17].
- Resolving Tumor Microenvironment Complexity: Algorithms can dissect the methylation contributions of malignant, immune, and stromal compartments, revealing clinically relevant subgroups [84].
- Longitudinal Monitoring: Deconvolution of serial liquid biopsies enables tracking of cellular composition shifts during treatment, providing insights into therapy resistance mechanisms [85].
The integration of deconvolution methodologies with epigenetic biomarker development represents a powerful approach for advancing cancer diagnostics and personalized medicine.
Deconvolution algorithms have emerged as essential tools for addressing cell-type heterogeneity in biomedical research, particularly in the context of validating epigenetic biomarkers for early cancer detection. Performance benchmarking studies consistently identify Bisque, hspe (dtangle), and bMIND as top-performing methods for estimating cell proportions and cell-type-specific gene expressions across various biological contexts [83] [86]. The selection of an appropriate algorithm, however, depends on specific research requirements, including tissue type, available reference data, and the required cellular resolution.
Robust validation using orthogonal approaches—such as multi-assay datasets with RNAScope/IF measurements or controlled in vitro admixtures—provides critical assessment of algorithm performance under conditions that approximate real-world applications [83] [84]. As epigenetic biomarkers continue to gain prominence in liquid biopsy development for early cancer detection [85] [17], deconvolution methods will play an increasingly important role in ensuring the accurate interpretation of these complex molecular signals within heterogeneous clinical samples.
The reliability of epigenetic biomarkers in cancer early detection research is fundamentally dependent on sample quality. Pre-analytical variables—including sample type selection, collection methods, and DNA extraction efficiency—directly impact the integrity and analytical performance of molecular biomarkers. This guide provides a comparative analysis of extraction methods and sample handling protocols to optimize the pre-analytical phase for epigenetic biomarker validation in cancer research.
Sample Type Considerations for Epigenetic Analysis
The choice of biological sample matrix introduces specific methodological considerations for downstream epigenetic analysis. Blood derivatives (plasma and serum) and saliva each present distinct advantages and limitations for DNA methylation studies.
Table 1: Comparison of Biological Matrices for DNA Methylation Analysis
| Sample Type | Key Characteristics | Advantages | Limitations | Primary Applications |
|---|---|---|---|---|
| Plasma | Liquid fraction of blood with anticoagulant; contains circulating cell-free DNA (cfDNA) | Preferred for metabolomics; suitable for cfDNA analysis [88] | Requires centrifugation; potential anticoagulant interference | Liquid biopsy, cancer detection, non-invasive prenatal testing |
| Serum | Liquid fraction after blood clotting; contains cfDNA | Clotting process may concentrate certain analytes | Clotting process removes platelets and clotting factors; potentially higher variability [88] | Biomarker discovery, retrospective studies |
| Saliva | Mixed fluid containing epithelial and immune cells; ~65% immune cells, ~35% epithelial cells [89] | Non-invasive collection; high participant compliance; good DNA yield [90] [91] | Bacterial DNA contamination; variable cell composition [90] | Pediatric studies, longitudinal monitoring, psychological stress research |
| Dried Blood Spots (DBS) | Capillary blood dried on filter paper | Minimal invasiveness; cost-effective storage and transport [92] | Limited sample volume; potential analytical variation [92] | Neonatal screening, population studies, resource-limited settings |
The selection between plasma and serum requires careful consideration. One study comparing five extraction methods for metabolomics found plasma to be the most suitable matrix when combined with methanol-based extraction methods [88]. For DNA methylation analysis, studies have demonstrated moderate cross-tissue correlation between blood and saliva for second- and third-generation methylation profile scores (MPSs) after correcting for cell composition, with PCGrimAge showing the highest intraclass correlation coefficient (ICC = 0.76) [89].
Comparative Analysis of DNA Extraction Methods
Blood-Derived DNA Extraction
Multiple methods exist for DNA extraction from blood and its derivatives, each with distinct performance characteristics.
Table 2: Comparison of DNA Extraction Methods from Blood and Saliva
| Extraction Method | Principle | Average Yield | Purity (A260/A280) | Time Requirement | Cost Considerations |
|---|---|---|---|---|---|
| Solvent Precipitation (Methanol) | Protein precipitation using organic solvents | High (metabolite coverage) [88] | Outstanding accuracy [88] | Moderate | Low cost |
| Column-Based Kits (QIAamp, Roche High Pure) | Silica-membrane binding | Variable; Roche showed higher DNA concentrations than other column methods [92] | Good purity with contaminants removed | 1.5-2 hours for 10 samples [92] | Higher cost per sample |
| Chelex-100 Boiling Method | Ion-exchange resin, heat-induced cell lysis | Significantly higher ACTB DNA concentrations vs. other methods [92] | Lower purity (no purification steps) [92] | Rapid (<1 hour) | Cost-effective |
| Solid-Phase Extraction (SPE) | Selective binding with phospholipid removal | Reduced overall metabolite coverage [88] | Increased repeatability, reduced matrix effects [88] | Time-consuming | Moderate to high |
Method Performance in Specialized Applications
For dried blood spots (DBS), a back-to-back comparison of five extraction methods identified the Chelex-100 resin method as superior, yielding significantly higher ACTB DNA concentrations (p < 0.0001) compared to column-based methods [92]. Optimization experiments further demonstrated that reducing elution volumes from 150 μL to 50 μL significantly increased DNA concentration without requiring additional starting material [92].
In plant DNA extraction (with relevance to difficult biological samples), a comparison of three methods found that a modified Mericon extraction method provided the highest DNA yields with better quality, affordable cost, and less time compared to CTAB-based methods and the DNeasy Qiagen Plant Mini Kit [93].
Pre-Analytical Variables Impacting Sample Quality
Pre-analytical factors significantly influence DNA integrity and analytical outcomes, particularly for cell-free DNA (cfDNA) analysis.
Critical Pre-Analytical Factors
Sample Collection: The choice of blood collection tubes (EDTA tubes vs. specialized cell-free DNA collection tubes) affects cfDNA stability [94]. For saliva, collection methods (stimulated vs. unstimulated) impact sample composition and downstream analysis [91].
Processing Time and Temperature: Extended processing time and inappropriate storage temperatures accelerate miRNA and cfDNA degradation [94] [95]. Studies demonstrate time- and temperature-dependent degradation profiles for miRNAs in blood samples [95].
Biological and Physiological Variables: Demographic factors (age, gender), lifestyle (diet, exercise), psychophysical state (obesity, stress), and physiological processes (pregnancy, menstruation) influence cfDNA characteristics [94]. For instance, cfDNA levels are significantly higher in elderly individuals (over 60 years) compared to younger people [94].
Impact of Pre-Analytical Variables on cfDNA Analysis
Cell-free DNA analysis is particularly vulnerable to pre-analytical variability. The journey from sample collection to cfDNA analysis involves multiple steps—preparation, collection, transportation, temporary storage, processing, extraction, quality control, and long-term storage—each introducing potential variables that affect analytical results [94]. The concentration and fragment size distribution of cfDNA can be altered by delays in processing, improper storage conditions, or choice of extraction method, potentially compromising downstream applications such as cancer detection or non-invasive prenatal testing [94].
Experimental Protocols for Method Validation
Protocol 1: Chelex-100 DNA Extraction from Dried Blood Spots
This optimized protocol is particularly advantageous for research in low-resource settings and large populations [92]:
- Sample Preparation: Punch one 6 mm DBS disk into a 1.5-2.0 mL microcentrifuge tube.
- Soaking Step: Incubate the DBS punch overnight at 4°C in 1 mL of Tween20 solution (0.5% Tween20 in PBS).
- Washing: Remove Tween20 solution and add 1 mL of PBS. Incubate for 30 minutes at 4°C.
- DNA Extraction: Remove PBS and add 50 μL of pre-heated 5% (m/v) Chelex-100 solution (56°C).
- Heat Incubation: Incubate at 95°C for 15 minutes, with brief pulse-vortexing every 5 minutes.
- Clarification: Centrifuge for 3 minutes at 11,000 rcf to pellet Chelex beads and residual paper.
- Recovery: Transfer supernatant to a new tube using a pipette.
- Final Clarification: Repeat centrifugation and transfer supernatant for precision.
Validation: Quantify DNA yield using spectrophotometry (DeNovix DS-11) and qPCR amplification of housekeeping genes (e.g., ACTB). Assess suitability for downstream applications such as T-cell receptor excision circle (TREC) quantification for severe combined immunodeficiency (SCID) screening [92].
Protocol 2: Solvent Precipitation for Plasma Metabolomics
This protocol demonstrates high metabolite coverage and outstanding accuracy for LC-MS analysis [88]:
- Sample Preparation: Aliquot 100 μL of plasma into a microcentrifuge tube.
- Protein Precipitation: Add 300 μL of cold methanol (or methanol:acetonitrile 1:1 v/v) to the plasma sample.
- Vortexing and Incubation: Vortex vigorously for 60 seconds and incubate at -20°C for 60 minutes.
- Precipitation: Centrifuge at 14,000 × g for 15 minutes at 4°C to pellet precipitated proteins.
- Recovery: Transfer supernatant to a new tube.
- Concentration: Evaporate solvent under nitrogen stream or vacuum centrifugation.
- Reconstitution: Reconstitute dried extract in initial mobile phase compatible with LC-MS analysis.
Quality Control: Spike samples with isotope-labelled internal standards to monitor extraction efficiency, matrix effects, and analytical performance [88].
Visualization of Optimal Workflows
Research Reagent Solutions for Sample Processing
Table 3: Essential Research Reagents for Sample Processing and DNA Extraction
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Blood Collection Tubes | EDTA tubes, specialized cfDNA collection tubes | Sample preservation and stabilization | Choice affects cfDNA stability; specialized tubes enable room temperature storage [94] |
| Saliva Collection Kits | DNA Genotek, Oragene DNA Collection Kit | Nucleic acid stabilization in saliva | Enable room temperature storage and transport; maintain DNA integrity [91] |
| Protein Precipitation Reagents | Methanol, methanol:acetonitrile (1:1 v/v) | Protein removal for metabolomics and proteomics | Methanol-based methods show broad specificity and outstanding accuracy [88] |
| Ion-Exchange Resins | Chelex-100 resin | DNA purification via chelation of metal ions | Cost-effective; suitable for high-throughput DBS processing [92] |
| Silica-Membrane Kits | QIAamp DNA Mini Kit, Roche High Pure Kit | Selective DNA binding and purification | Provide standardized protocols; relatively pure DNA extracts [92] |
| Lysis Buffers | CTAB buffer, ATL buffer (Qiagen) | Cell membrane disruption and DNA release | CTAB effective for difficult samples (e.g., plants, cereals) [93] |
| Enzymatic Reagents | Proteinase K, RNase A | Protein and RNA degradation | Essential for removing contaminants from DNA extracts [92] [93] |
| Quality Control Assays | ACTB qPCR, miRNA panels | Assessment of DNA/RNA quality and quantity | Identify hemolysis, platelet contamination, and degradation [92] [95] |
Optimal sample quality in epigenetic biomarker research requires meticulous attention to pre-analytical variables. Method selection should be guided by specific research objectives, sample availability, and downstream applications. Solvent precipitation methods offer broad metabolite coverage for plasma metabolomics, while Chelex-100 extraction provides a cost-effective, efficient approach for DNA isolation from dried blood spots. Saliva represents a viable alternative to blood for DNA methylation studies, particularly in pediatric populations or when decentralized collection is necessary, though careful attention to cell composition correction is essential. Standardized protocols and comprehensive quality control measures throughout the pre-analytical phase are fundamental for generating reliable, reproducible data in cancer early detection research.
Formalin-Fixed Paraffin-Embedded (FFPE) samples represent an invaluable resource for cancer research, with an estimated 400 million to over one billion specimens archived worldwide in hospital biobanks [96]. These archives, often accompanied by detailed clinical records and long-term outcome data, provide an unparalleled opportunity for large-scale retrospective studies in cancer epigenetics, particularly for validating biomarkers for early detection [96] [18]. However, the very preservation process that enables this extensive archiving also introduces significant challenges for molecular analysis, especially for DNA-based assays.
The fixation and embedding process triggers chemical modifications that fragment DNA and create protein cross-links, ultimately compromising nucleic acid integrity [97] [96]. For the validation of epigenetic biomarkers in early cancer detection—a field where DNA methylation patterns and other epigenetic marks have shown exceptional promise [18] [98]—understanding and mitigating these quality issues becomes paramount. This guide objectively compares the performance of FFPE-derived DNA against alternative sample types and provides researchers with evidence-based strategies for maximizing experimental success in epigenetic biomarker validation.
DNA Quality Comparison: FFPE Versus Alternative Preservation Methods
Quantitative Assessment of DNA Yield and Integrity
The integrity of DNA extracted from FFPE tissues is fundamentally compromised compared to cryopreserved alternatives. A recent pan-cancer comparison of matched samples demonstrated that cryopreserved tissues yielded a 4.2-fold increase in DNA per milligram of tissue compared to FFPE samples (p-value < 0.001) [99]. More critically, DNA quality assessments revealed a 223% increase in DNA quality number and a 9-fold increase in DNA fragments >40,000 bp from cryopreserved tissues (p-value < 0.0001) [99], highlighting the profound impact of preservation method on nucleic acid integrity.
Table 1: DNA Quantity and Quality Metrics Across Preservation Methods
| Metric | FFPE Samples | Cryopreserved/Frozen Samples | Statistical Significance |
|---|---|---|---|
| DNA yield per mg tissue | Significantly lower | 4.2-fold higher | p < 0.001 [99] |
| DNA purity (A260/280) | Variable; often compromised | Generally optimal | Not quantified |
| High molecular weight DNA (>40,000 bp) | Minimal fragments | 9-fold more abundant | p < 0.0001 [99] |
| DNA Quality Number (DQN) | Significantly lower | 223% higher | p < 0.0001 [99] |
| Degree of fragmentation | High | Low | Qualitative [97] [96] |
| Downstream compatibility | Limited for long-read technologies | Suitable for all sequencing platforms | Qualitative [99] |
The timing of analysis further compounds these quality issues in FFPE samples. A systematic evaluation of lung adenocarcinoma FFPE samples stored for varying durations revealed that aging significantly contributes to DNA fragmentation, with notable increases observed between 0.5 vs. 3 years (p=0.02 for silica-membrane extraction; p=0.03 for total-tissue DNA collection) and between 9 vs. 12 years (p<0.01 and p=0.03, respectively) [97]. Interestingly, this same study found that aging had no significant effect on absolute DNA yield or DNA purity, suggesting that quantification metrics alone are insufficient indicators of FFPE sample quality [97].
Technical Performance in Epigenetic Analyses
For DNA methylation analysis specifically, which serves as a cornerstone for epigenetic cancer biomarkers [18] [98], FFPE samples demonstrate particular limitations. A comparative study of cardiac tissue from nine individuals found that while frozen and FFPE tissues produced reproducible DNA methylation results, the methylation levels in FFPE samples were significantly overestimated compared to fresh and frozen tissues at 21.4% of examined CpG sites, while 5.7% were underestimated [100].
The Infinium MethylationEPIC array analysis revealed that a substantially higher percentage of CpG probes were filtered out during quality control for FFPE samples (18.4%) compared to fresh (13.6%) or frozen (13.2%) tissues (p < 0.05) [100], indicating more frequent analytical failure. Principal component analysis clearly separated FFPE from fresh and frozen samples [100], highlighting the systematic bias introduced by FFPE processing.
Table 2: DNA Methylation Analysis Performance Across Sample Types
| Performance Metric | Fresh Tissue | Frozen Tissue | FFPE Tissue |
|---|---|---|---|
| Reproducibility (median r² of duplicates) | 0.993 | 0.994 | 0.992 [100] |
| Correlation with fresh tissue (median r²) | 1.000 | 0.995 | 0.978 [100] |
| CpG probes removed during QC (%) | 13.6% | 13.2% | 18.4% [100] |
| CpG sites with overestimated β-values | Reference | Comparable to fresh | 21.4% [100] |
| CpG sites with underestimated β-values | Reference | Comparable to fresh | 5.7% [100] |
| Compatibility with methylation arrays | Optimal | Optimal | Good with increased data loss [100] |
Despite these limitations, DNA from FFPE tissues remains analytically valuable when appropriate quality control measures are implemented. Several studies have successfully identified and validated epigenetic biomarkers in cancer research using FFPE-derived DNA [18] [98]. For instance, one study identified and validated 15 differentially methylated regions (DMRs) in lung adenocarcinoma using FFPE samples, with specific hypermethylation patterns in genes including OSR1, SIM1, and HOXB3/HOXB4 demonstrating high potential as cancer biomarkers [98].
Experimental Protocols for Quality Assessment and Analysis
DNA Extraction Method Comparison
The choice of DNA extraction method significantly impacts the quantity and quality of DNA obtained from FFPE samples. Two primary approaches show distinct performance characteristics:
Silica-Binding DNA Collection Method (QIAamp DNA FFPE Tissue Kit): This approach yields less fragmented DNA but with lower overall yield. It includes a crosslink removal step involving incubation at 95°C for 10 minutes and purification through silica membrane washing [97].
Total Tissue DNA Collection Method (WaxFree DNA Extraction Kit): This method provides significantly higher DNA yield (p<0.01) but includes more contaminants and yields more fragmented DNA compared to the silica-binding method (p<0.01) [97]. It features a longer crosslink removal step (incubation at 90°C for 60 minutes) and employs a resin-enzyme mix for PCR inhibitor removal [97].
The selection between these methods depends on the downstream application: silica-binding methods are preferable for PCR-based assays requiring higher purity, while total tissue collection may be更适合 for applications where yield is the primary concern.
DNA Quantification and Quality Control Workflow
Robust quality assessment is essential before employing FFPE-derived DNA in epigenetic analyses. A recommended workflow includes:
DNA Quantification: Perform using multiple methods including UV spectrophotometry (for concentration and A260/280 purity ratio), fluorescent dye-based methods (e.g., PicoGreen for double-stranded DNA quantification), and quantitative PCR (qPCR) [97].
DNA Integrity Assessment:
- qPCR-based Methods: Employ kits such as the Quantifiler Trio DNA Quantification Kit (degradation index) and Infinium HD FFPE QC kit (ΔCt value) [100]. FFPE tissue typically shows statistically significant higher degradation indices (mean = 2.51) compared to fresh (mean = 0.97) and frozen tissues (mean = 0.84) [100].
- Fragment Analysis: Use fragment analyzers (e.g., Agilent Fragment Analyzer System or Femto Pulse System) to determine the distribution of DNA fragment sizes [99].
Quality Scoring System: Implement a Q-score based on qPCR product size ratios (e.g., Q129/Q41 and Q305/Q41), where lower DNA integrity produces lower Q-scores [97].
DNA Methylation Analysis Techniques for FFPE-Derived DNA
Several methylation analysis methods have been successfully applied to FFPE-derived DNA:
Methylation-Sensitive High Resolution Melting (MS-HRM): Used to validate differentially methylated regions in lung adenocarcinoma samples, enabling detection of methylation changes in candidate biomarkers such as OSR1, SIM1, and HOXB3/HOXB4 [98].
Infinium MethylationEPIC Array: Requires high-quality DNA after bisulfite conversion; studies show increased data loss with FFPE samples but generally reproducible results when quality thresholds are met [100].
Methylation-Specific Multiplex Ligation-Dependent Probe Amplification (MS-MLPA): Employed for clinical evaluation of specific gene methylation events, such as MLH1 promoter hypermethylation in colorectal cancer [18].
Pyrosequencing: Provides quantitative methylation data for specific genomic regions; used for MGMT promoter methylation assessment in glioblastoma [18].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents for FFPE DNA Analysis in Epigenetic Studies
| Product Category | Specific Examples | Primary Function | Considerations for FFPE Samples |
|---|---|---|---|
| DNA Extraction Kits | QIAamp DNA FFPE Tissue Kit (Qiagen) | Silica-membrane based DNA purification | Optimized for FFPE cross-link reversal; yields less fragmented DNA [97] |
| DNA Extraction Kits | WaxFree DNA Extraction Kit (Trimgen) | Total tissue DNA collection with inhibitor removal | Higher DNA yield but more fragmentation; includes resin-enzyme purification [97] |
| DNA Quantification | Quantifiler Trio DNA Quantification Kit (Thermo Fisher) | qPCR-based DNA quantification and degradation assessment | Provides degradation index; higher values indicate poorer quality [100] |
| DNA Quantification | Infinium HD FFPE QC Kit (Illumina) | Quality assessment for methylation arrays | ΔCt values >2 indicate poor quality [100] |
| DNA Quantification | Qubit dsDNA HS Assay Kit (Thermo Fisher) | Fluorometric DNA quantification | Selective for double-stranded DNA; more accurate than UV for fragmented DNA [97] |
| Methylation Analysis | Infinium MethylationEPIC Kit (Illumina) | Genome-wide methylation profiling | Increased probe failure with FFPE DNA; requires quality screening [100] |
| Methylation Analysis | MS-HRM reagents | Targeted methylation analysis | Compatible with fragmented DNA; suitable for biomarker validation [98] |
| Methylation Analysis | MS-MLPA Kits (MRC-Holland) | Multiplex methylation assessment | Used for clinical marker evaluation (e.g., MLH1, MGMT) [18] |
| Bisulfite Conversion | EZ DNA Methylation Kit (Zymo Research) | DNA bisulfite treatment for methylation analysis | Compatible with fragmented DNA from FFPE sources [14] |
FFPE samples present both opportunities and challenges for epigenetic biomarker discovery and validation. While they provide unparalleled access to extensive archival collections with clinical annotations, their compromised DNA quality requires careful methodological considerations.
For researchers designing studies involving FFPE specimens for epigenetic cancer biomarker research, the following evidence-based recommendations are proposed:
Implement Rigorous Quality Control: Utilize multiple DNA quality assessment methods (spectrophotometry, fluorometry, qPCR, and fragment analysis) to establish fitness-for-purpose for intended epigenetic analyses [97] [100] [99].
Select Appropriate Extraction Methods: Choose silica-membrane methods when DNA integrity is prioritized over yield, particularly for longer amplicon applications [97].
Account for Storage Duration: Consider sample age as a significant factor in experimental design, as fragmentation increases substantially with storage time [97].
Validate Findings with Complementary Methods: Confirm epigenetic biomarkers identified in FFPE samples using multiple analytical approaches to control for potential artifacts [18] [98].
Consider Prospective Collection: When possible, supplement retrospective FFPE studies with prospectively collected frozen specimens to control for preservation-related artifacts [96] [99].
As epigenetic biomarkers continue to show promise for early cancer detection [18] [98] [11], the strategic utilization of FFPE archives will remain crucial for validating these markers across large populations with extensive clinical follow-up. By understanding and addressing the inherent limitations of these valuable samples, researchers can more effectively leverage them to advance cancer diagnostics and personalized medicine.
The pursuit of early cancer detection through biomarkers represents a paradigm shift in oncology. However, a significant challenge complicating this endeavor is the inherent biological noise originating from non-malignant processes, primarily aging and inflammation. These processes induce molecular changes that can masquerade as cancer signals, leading to compromised diagnostic specificity and false positives [101] [102]. The scientific community is now focused on deciphering this complex molecular interplay to isolate cancer-specific signatures. This guide provides a comparative analysis of biomarker performance, detailing the experimental methodologies that underpin advances in distinguishing true cancer signals from age-related and inflammatory backgrounds, with a specific focus on validating epigenetic biomarkers for early detection research.
The Shared Biology of Cancer, Aging, and Inflammation
Cancer and aging are interconnected biological processes driven by overlapping hallmarks, including genomic instability, epigenetic alterations, and chronic inflammation [102]. Aging is characterized by a functional decline in tissues and a gradual accumulation of molecular damage, while cancer represents a dysregulated, proliferative state. Despite their different outcomes, they share common mechanistic pathways.
Genomic and Epigenetic Instability: Both aging and cancer are fueled by the accumulation of DNA damage. In aging, this leads to cellular senescence and functional decline, whereas in cancer, it provides the genetic diversity for tumor evolution [102]. A key epigenetic mechanism is DNA methylation. Aging and cancer are both associated with global hypomethylation, which can lead to genomic instability and oncogene activation, and site-specific hypermethylation, which can silence tumor suppressor genes like p16 and VHL [35]. This convergence on epigenetic regulation makes certain methylation marks ambiguous without careful contextualization.
Chronic Inflammation: Elevated levels of inflammatory markers, such as C-reactive protein (CRP), interleukins, and TNF-α, are hallmarks of both the aging process (a condition known as "inflammaging") and the tumor microenvironment [101]. This chronic inflammatory state can promote cellular proliferation and survival, fueling tumorigenesis and creating a background signal that can obscure cancer-specific biomarkers.
The following diagram illustrates the convergent and divergent pathways of these shared biological processes.
Comparative Analysis of Biomarker Performance
Researchers have employed diverse biomarker classes to achieve cancer-specific detection. The table below summarizes the specificity challenges and validation status of key biomarker types in the context of aging and inflammation.
Table 1: Specificity Challenges of Cancer Biomarker Classes
| Biomarker Class | Specificity Challenge | Strategies to Enhance Specificity | Clinical Translation Example |
|---|---|---|---|
| Single Protein Biomarkers (e.g., PSA, CA-125) | Low specificity; levels influenced by benign conditions (prostatitis, endometriosis) and age [79]. | Use in combination with other markers (multi-analyte panels); adjust age-specific reference ranges [79]. | FDA-approved but leading to overdiagnosis and unnecessary procedures [79]. |
| Epigenetic Clocks (e.g., HorvathAge, PhenoAge) | Strongly correlated with chronological age; acceleration is a general marker of aging and mortality risk, not specific to cancer [8] [103]. | Develop cancer-specific epigenetic clocks; use as a risk stratification layer rather than a direct diagnostic tool [8]. | PhenoAge acceleration associated with increased risk of lung and colorectal cancer in UK Biobank [103]. |
DNA Methylation Panels (e.g., SEPT9, SHOX2) |
Locus-specific hyper/hypomethylation can occur in pre-malignant conditions and non-cancerous age-related tissues [35]. | Focus on multi-locus methylation signatures; combine methylation with mutational data [79] [35]. | FDA-approved SEPT9 methylated DNA test for colorectal cancer screening [35]. |
| Circulating Tumor DNA (ctDNA) Methylation | Fragmentation and low concentration in early-stage disease; methylation patterns must be distinguished from age-related methylation drift [78] [35]. | Use targeted methylation sequencing and ML to identify cancer-specific pan-cancer signatures [35]. | GRAIL's Galleri test (targeted methylation sequencing of ctDNA) [35]. |
Experimental Protocols for Biomarker Validation
Validating the specificity of a candidate biomarker requires a rigorous, multi-stage experimental workflow. The following section details key protocols for controlling age and inflammatory confounders.
Study Design and Cohort Selection
A foundational step is the assembly of a well-characterized cohort that allows for the dissociation of cancer signals from confounders.
- Primary Protocol: Prospective cohort studies with nested case-control designs.
- Key Methodology:
- Participant Recruitment: Recruit individuals from broad age ranges (e.g., 40-75) with no history of cancer at baseline. Participants should undergo standardized blood collection (e.g., using cell-stabilizing tubes) to ensure sample integrity for ctDNA and methylation analysis [104].
- Data Collection: Systematically collect sociodemographic, lifestyle, and health information. Critical covariates include age, sex, body mass index (BMI), smoking status, and comorbidities such as diabetes, cardiovascular disease, and chronic inflammatory conditions (e.g., rheumatoid arthritis) [104] [103]. These factors are essential for statistical adjustment.
- Follow-up and Case Ascertainment: Follow participants over time (e.g., 10+ years). Incident cancer cases are identified via linkage to national cancer registries (e.g., ICD-10 codes). For each case, one or more controls are selected matched on age, sex, and date of biospecimen collection [103].
Laboratory Analysis and Multi-Omics Profiling
The analytical phase focuses on generating high-quality, quantitative data from biospecimens.
- Primary Protocol: DNA methylation profiling from plasma (liquid biopsy) and tissue.
- Key Methodology:
- Plasma Separation: Process blood samples within a strict time window (e.g., 2-4 hours of draw) using standardized centrifugation protocols to isolate platelet-poor plasma, which is critical for the reproducibility of cell-free DNA (cfDNA) measurements [104].
- cfDNA Extraction and Bisulfite Conversion: Extract cfDNA from plasma using commercial kits. Treat DNA with sodium bisulfite, which converts unmethylated cytosines to uracils while leaving methylated cytosines unchanged. This allows for the subsequent quantification of methylation status at single-base resolution [35].
- Methylation Profiling:
- Genome-Wide Discovery: Use array-based technologies (Illumina Infinium MethylationEPIC BeadChip) or whole-genome bisulfite sequencing (WGBS) on a discovery cohort to identify differentially methylated regions (DMRs) between cancer cases and controls [35] [8].
- Targeted Validation: Develop targeted assays (e.g., bisulfite sequencing panels, PCR-based assays) for the most promising DMRs and validate them in a larger, independent cohort [35].
Data Analysis and Machine Learning Modeling
The final stage involves computational models to integrate complex data and build predictive algorithms.
- Primary Protocol: Supervised machine learning for classification and feature importance analysis.
- Key Methodology:
- Feature Engineering: Input features include methylation beta-values from hundreds to thousands of CpG sites, chronological age, and levels of inflammatory markers (e.g., CRP). Age acceleration residuals can be calculated by regressing epigenetic age on chronological age [8] [103].
- Model Training and Validation: Use multiple algorithms (e.g., XGBoost, Random Forest, Logistic Regression) on the training set (typically 80% of data). Perform 5-fold cross-validation to tune hyperparameters and prevent overfitting. Evaluate the final model on the held-out test set (20% of data) [8].
- Model Interpretation: Apply SHapley Additive exPlanations (SHAP) values to quantify the contribution of each feature (e.g., a specific CpG site, inflammatory marker) to the model's prediction. This helps identify which features are driving the cancer classification versus those linked to background aging or inflammation [8].
The following diagram maps this multi-stage experimental workflow.
The Scientist's Toolkit: Essential Research Reagent Solutions
The experimental protocols described rely on a suite of specialized reagents and platforms. The table below catalogs key solutions for research in this field.
Table 2: Essential Research Reagents and Platforms
| Research Solution | Function | Example Use-Case |
|---|---|---|
| Cell-Free DNA Blood Collection Tubes (e.g., Streck cfDNA BCT, PAXgene Blood cpb DNA Tube) | Stabilize nucleated blood cells to prevent genomic DNA contamination and preserve cfDNA profile post-phlebotomy. | Ensures pre-analytical sample integrity for reproducible ctDNA quantification in multi-center cohort studies [104]. |
| Illumina Infinium MethylationEPIC BeadChip | Genome-wide methylation array profiling covering > 850,000 CpG sites, including enhancer regions. | Discovery-phase identification of differentially methylated regions (DMRs) associated with cancer in large biobanks [35] [8]. |
| Bisulfite Conversion Kits | Chemical treatment of DNA to differentiate methylated and unmethylated cytosines for downstream analysis. | Prepares genomic DNA (from tissue) or cfDNA (from plasma) for targeted bisulfite sequencing or PCR assays [35]. |
| Targeted Methylation Sequencing Panels (e.g., GRAIL's targeted panel) | Multiplexed PCR or hybrid capture-based sequencing for deep, cost-effective profiling of pre-defined CpG sites. | Validation and clinical application of a pan-cancer methylation signature in liquid biopsies [35]. |
| Ultra-Sensitive Immunoassays (e.g., Simoa, ELISA) | Quantify low-abundance protein biomarkers in serum/plasma (e.g., CRP, GDF-15, cytokines). | Measuring inflammatory and senescence-associated proteins as confounding variables or complementary biomarkers [101] [104]. |
Distinguishing cancer-specific biomarker signals from the background noise of aging and inflammation is a central challenge in modern oncology research. The path forward lies not in seeking a single perfect biomarker, but in the sophisticated integration of multi-omics data—particularly DNA methylation—using machine learning models trained on large, meticulously characterized cohorts. By adhering to rigorous experimental protocols that explicitly account for age and inflammatory confounders, and by leveraging the powerful tools now available, researchers can enhance biomarker specificity. This progress is critical for developing reliable early detection tests that minimize false positives and pave the way for a new era of precision cancer prevention.
The successful validation of epigenetic biomarkers for early cancer detection represents a paradigm shift in oncology, yet significant hurdles related to analytical sensitivity persist. This review systematically examines the fundamental technological and biological barriers limiting detection sensitivity in early-stage malignancies. We synthesize current experimental data on circulating tumor DNA (ctDNA) abundance, DNA methylation biomarkers, and microRNA profiling across cancer types, with particular focus on the performance characteristics of emerging detection platforms. The integration of artificial intelligence with multi-omics approaches demonstrates promising pathways to overcome these limitations, though standardization and validation challenges remain. By objectively comparing the sensitivity metrics of current technologies and detailing experimental methodologies, this analysis provides researchers and drug development professionals with a framework for advancing more robust epigenetic biomarker validation strategies.
The clinical validation of epigenetic biomarkers for early cancer detection hinges on overcoming critical sensitivity limitations inherent in analyzing minimal tumor-derived material. Early-stage tumors shed remarkably small amounts of biomarker material into circulation, creating a profound signal-to-noise challenge against abundant background molecules from healthy cells [79] [78]. This "needle in a haystack" problem is compounded by biological factors including tumor size, vascularity, and location, as well as technological constraints of current detection platforms [5]. The convergence of these barriers often results in false negatives, particularly for stage I cancers where timely intervention could dramatically improve outcomes.
Epigenetic biomarkers—especially DNA methylation patterns and microRNAs—offer distinct advantages for early detection due to their stability, cancer-specific patterning, and early emergence in tumorigenesis [35] [105]. However, realizing their clinical potential requires confronting the sensitivity limitations that currently restrict reliable detection. This review systematically compares the performance of current technologies, details experimental protocols for sensitivity optimization, and identifies promising pathways toward overcoming these barriers through integrated technological and biological approaches.
Biological Barriers to Detection Sensitivity
Limited Circulating Tumor DNA Abundance in Early-Stage Cancers
The fundamental biological barrier in early cancer detection is the extremely low concentration of tumor-derived material in circulation, particularly ctDNA. In early-stage disease, ctDNA often constitutes less than 0.1% of total cell-free DNA, creating an analytical challenge against a background of predominantly non-tumor derived DNA [78] [5]. This low abundance directly impacts the limit of detection for all downstream technologies, regardless of their intrinsic sensitivity.
Table 1: Biological Barriers to Detection Sensitivity in Early-Stage Cancers
| Biological Factor | Impact on Sensitivity | Representative Data | Clinical Consequences |
|---|---|---|---|
| Low ctDNA fraction | <0.1% of total cfDNA in stage I tumors [5] | Early-stage lung cancer: median ctDNA fraction 0.1% vs. 5.6% in metastatic disease [79] | High false-negative rates for early detection |
| Tumor location effects | CNS tumors shed minimal ctDNA into blood [5] | Bile outperforms plasma for cholangiocarcinoma detection [5] | Variable performance across cancer types |
| Fragment length & integrity | ctDNA more fragmented than non-malignant cfDNA [78] | Median ctDNA length ~165bp vs. ~185bp for non-malignant cfDNA [5] | Recovery biases in extraction and amplification |
| Molecular heterogeneity | Methylation patterns vary within and between tumors [106] | Only 20-30% of differentially methylated regions consistent across breast cancer subtypes [106] | Requires multi-marker panels for comprehensive detection |
The biological challenges extend beyond mere abundance. The rapid clearance of ctDNA from circulation, with half-lives estimated between minutes to a few hours, creates a narrow temporal window for detection [5]. Additionally, the fragmentation patterns of ctDNA differ from non-malignant cell-free DNA, potentially introducing biases during extraction and amplification steps [78]. Tumor location further influences detectability, with central nervous system tumors and those confined to epithelial layers shedding minimal material into blood compared to more vascularized malignancies [5].
Tissue-Specific and Subtype-Dependent Biomarker Expression
The biological heterogeneity of cancer manifests in distinct epigenetic profiles across tissue types and molecular subtypes, creating additional barriers to pan-cancer detection approaches. DNA methylation patterns demonstrate considerable variation between cancer types, with certain malignancies exhibiting more pronounced epigenetic alterations than others [106]. For instance, triple-negative breast cancers show distinct hypermethylation profiles compared to hormone receptor-positive subtypes, potentially influencing detection sensitivity across the disease spectrum [105] [106].
This heterogeneity extends to microRNA biomarkers, where expression patterns vary significantly across cancer types and risk categories. In prostate cancer, miR-199a-5p demonstrates consistent overexpression across all Gleason risk categories, while miR-24-3p appears exclusively overexpressed in high-risk disease [107]. Such subtype-dependent variation complicates the development of universal detection panels and necessitates cancer-specific sensitivity thresholds.
Technological Limitations and Platform Performance
Sensitivity Constraints of Current Detection Technologies
The technological landscape for epigenetic biomarker detection encompasses diverse platforms with varying sensitivity profiles, each with distinct advantages and limitations for early cancer detection. PCR-based methods, including droplet digital PCR (ddPCR), offer high sensitivity for targeted applications but limited multiplexing capability. In contrast, next-generation sequencing (NGS) approaches enable comprehensive genome-wide profiling but often with reduced sensitivity for low-frequency variants unless deep sequencing is employed [105].
Table 2: Performance Comparison of DNA Methylation Detection Technologies
| Technology | Detection Sensitivity | Optimal Input DNA | Multiplexing Capacity | Cost & Throughput | Best Applications |
|---|---|---|---|---|---|
| Whole-Genome Bisulfite Sequencing (WGBS) | ~99% sensitivity at ≥30x coverage [105] | ≥100 ng [105] | Genome-wide | High cost, high throughput [105] | Comprehensive methylation profiling |
| Reduced Representation Bisulfite Sequencing (RRBS) | Moderate (covers ~10% of CpGs) [105] | ≥30 ng [105] | Epigenome-wide (CpG-rich regions) | Moderate cost & throughput [105] | Large-scale, cost-effective methylation analysis |
| Targeted Methylation Sequencing | Moderate (selected cancer-specific regions) [105] | ≥100 ng [105] | Targeted CpG sites (custom panels) | Variable cost ($$-$$$), moderate throughput [105] | Liquid biopsy, cancer biomarker panels |
| Enzymatic Methylation Sequencing (EM-seq) | ~99% sensitivity at ≥30x coverage [105] | ≥10 ng [105] | Whole genome (adaptable for targeted) | High cost, high throughput [105] | Bisulfite-free analysis (preserves DNA integrity) |
| Methylated DNA Immunoprecipitation Sequencing (MeDIP-seq) | Moderate (bias toward lower CpG density) [105] | ≥50 ng [105] | Epigenome-wide (low CpG density regions) | Moderate cost & throughput [105] | Analyzing methylation across large genomic regions |
| Pyrosequencing | Low (detects ≥5% methylation) [105] | ≥20 ng [105] | Targeted CpG regions | Low cost, low throughput [105] | Clinical assays, biomarker validation |
Bisulfite conversion-based methods remain widely used but introduce significant DNA degradation, losing up to 90% of input DNA during the conversion process [105]. This substantial loss exacerbates sensitivity challenges when analyzing the limited ctDNA available from early-stage tumors. Emerging bisulfite-free technologies like enzymatic methylation sequencing (EM-seq) and Tet-assisted pyridine borane sequencing (TAPS) demonstrate improved DNA preservation, thereby enhancing recovery of scarce tumor-derived molecules [105].
Methodological Workflows and Their Impact on Sensitivity
The complete experimental workflow—from sample collection to data analysis—profoundly influences ultimate detection sensitivity. Pre-analytical factors including blood collection tubes, processing timelines, extraction methods, and storage conditions can significantly impact ctDNA recovery and integrity [78] [5]. For instance, delays in plasma separation (>6 hours) can increase background wild-type DNA from leukocyte lysis, effectively diluting the already scarce tumor-derived DNA [5].
The analytical phase introduces additional sensitivity constraints through platform-specific limitations. During library preparation, PCR amplification biases can distort the original representation of methylated and unmethylated molecules [105]. Sequencing depth directly impacts sensitivity, with 30x coverage often considered minimum for reliable methylation calling, though early-stage detection may require significantly deeper sequencing (>100x) to identify rare tumor-derived fragments [105]. Bioinformatics pipelines for bisulfite-converted data face alignment challenges due to reduced sequence complexity, potentially introducing mapping errors that further compromise sensitivity [35].
Experimental Protocols for Sensitivity Optimization
High-Sensitivity Methylation Analysis Workflow
Advanced experimental protocols have been developed specifically to address sensitivity limitations in early cancer detection. The following workflow outlines a high-sensitivity approach for methylation-based detection of early-stage tumors:
Sample Collection and Processing: Collect blood using cell-stabilizing tubes (e.g., Streck, PAXgene) to prevent leukocyte lysis and background DNA release. Process within 6 hours with double centrifugation (3,000×g for 20min, then 15,000×g for 10min at 10°C) to obtain platelet-poor plasma [107]. Extract cfDNA using silica-membrane columns or magnetic beads optimized for short fragment recovery, with elution in low-EDTA TE buffer to prevent inhibition of downstream enzymatic steps.
Bisulfite-Free Conversion: Utilize enzymatic conversion (EM-seq) instead of traditional bisulfite treatment to preserve DNA integrity. Protocol: Fragment DNA to 200bp via sonration, then treat with EM-seq enzyme mix (TET2 and T4-BGT) for 3 hours at 37°C, followed by cleanup with solid-phase reversible immobilization (SPRI) beads [105]. This approach maintains >85% of input DNA compared to <10% recovery with bisulfite conversion.
Library Preparation and Target Enrichment: Employ unique molecular identifiers (UMIs) during adapter ligation to correct for PCR duplicates and sequencing errors. Use hybrid capture-based enrichment with biotinylated RNA baits targeting 5,000-10,000 differentially methylated regions pan-cancer. Hybridize at 65°C for 16 hours with rotation, followed by streptavidin bead capture and wash under stringent conditions [105].
Sequencing and Analysis: Sequence on Illumina platforms with minimum 100x coverage. Process data through a specialized bioinformatics pipeline: (1) UMI-aware alignment to bisulfite-converted reference genome; (2) methylation calling with beta-binomial modeling to account for amplification biases; (3) machine learning classification using random forest or convolutional neural networks trained on cancer-specific methylation signatures [35] [105].
Multi-Aanalyte Integration for Enhanced Sensitivity
Given the limitations of single-analyte approaches, integrated multi-analyte protocols significantly enhance detection sensitivity for early-stage cancers:
Parallel DNA Methylation and miRNA Profiling: Process split plasma samples for simultaneous DNA and RNA analyses. For miRNA: extract using miRNeasy Serum/Plasma Advanced Kit, reverse transcribe with miRCURY LNA RT Kit, and profile using pre-designed panels (e.g., 46-cancer miRNA panel) with spike-in controls for normalization [107]. For DNA methylation: process as above. Integrate results through machine learning models that weight contributions from both analyte types, significantly improving sensitivity over either method alone [107].
Multi-Modal Assay Integration: Combine epigenetic markers with protein biomarkers and fragmentomic patterns. Measure cancer-associated proteins (e.g., CA-19-9, CEA) via multiplex immunoassay on the same plasma sample. Analyze fragment length distribution of cfDNA through microfluidic electrophoresis. Integrate all three data types (epigenetic, proteomic, fragmentomic) using regularized regression models that adjust for clinical covariates, achieving superior sensitivity for stage I cancers compared to single-platform approaches [79] [78].
Emerging Solutions and Future Directions
Artificial Intelligence and Machine Learning Approaches
Artificial intelligence is revolutionizing sensitivity in early cancer detection by identifying subtle patterns across complex datasets that evade conventional analytical methods. Machine learning algorithms, particularly deep learning networks, can integrate multi-omics data to enhance detection of minimal tumor signals [35]. For DNA methylation analysis, convolutional neural networks (CNNs) demonstrate exceptional capability in recognizing cancer-specific methylation patterns from noisy background signals, achieving up to 10-fold improvement in detecting low-abundance ctDNA compared to traditional statistical thresholds [35].
The application of AI extends to tumor origin determination, a critical challenge in multi-cancer early detection tests. Gradient boosting machines (GBMs) trained on methylation patterns from over 50 cancer types can accurately predict tissue of origin even at low variant allele frequencies (<0.1%), enabling appropriate diagnostic follow-up for positive screens [35]. Furthermore, AI-powered approaches can deconvolute the cellular composition of cfDNA, distinguishing tumor-derived fragments from those released due to benign conditions including inflammation, age-related clonal hematopoiesis, and other non-malignant sources that contribute to false positives [35] [8].
Integrated Multi-Omics and Technological Innovations
The convergence of multiple technological innovations presents promising pathways to overcome current sensitivity limitations:
Table 3: Emerging Solutions for Sensitivity Enhancement
| Solution Approach | Technology Platform | Sensitivity Improvement | Current Limitations |
|---|---|---|---|
| Bisulfite-free sequencing | EM-seq, TAPS, SMRT-seq | 5-10x via reduced DNA degradation [105] | Higher cost, limited clinical validation |
| Multi-omics integration | Methylation + miRNA + proteins | 2-3x over single-analyte [78] [107] | Computational complexity, standardization |
| Third-generation sequencing | Nanopore, Single-Molecule Real-Time | Enables long-read methylation haplotyping [105] | Higher error rates, cost barriers |
| Machine learning enhancement | CNN, GBM, Random Forest | 3-10x for low VAF detection [35] | "Black box" interpretation, training data requirements |
| Local vs. systemic sources | Urine, saliva, bile, CSF | 5-20x for applicable cancers [5] | Limited to specific cancer types |
Liquid Biopsy Source Optimization: Moving beyond blood-based detection, local liquid biopsy sources offer dramatically improved sensitivity for applicable cancers. For urological malignancies, urine testing demonstrates 5-20x higher sensitivity than plasma-based approaches due to direct contact with tumors [5]. Similarly, bile outperforms plasma for cholangiocarcinoma, cerebrospinal fluid for central nervous system tumors, and saliva for head and neck cancers [5]. This paradigm of source selection based on tumor location represents a fundamental shift in approach to sensitivity optimization.
Third-Generation Sequencing and Epigenetic Mapping: Long-read sequencing technologies from Oxford Nanopore and Pacific Biosciences enable comprehensive methylation haplotyping across individual DNA molecules, preserving phasing information lost in short-read approaches [105]. This capability allows detection of cancer-specific epigenetic patterns on single DNA molecules, significantly enhancing signal-to-noise discrimination. When combined with molecular barcoding strategies that reduce PCR duplicates and sequencing errors, these platforms demonstrate potential for single-molecule methylation analysis at extremely low input levels [105].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Essential Research Reagents and Platforms for Epigenetic Biomarker Validation
| Reagent/Platform | Function | Key Considerations | Representative Products |
|---|---|---|---|
| Cell-stabilizing blood collection tubes | Preserve blood cell integrity during transport | Critical for preventing background DNA release | Streck Cell-Free DNA BCT, PAXgene Blood ccfDNA tubes |
| cfDNA extraction kits | Isolation of high-quality circulating DNA | Optimized for short fragment recovery | QIAamp Circulating Nucleic Acid Kit, miRNeasy Serum/Plasma Advanced Kit |
| Bisulfite conversion reagents | DNA modification for methylation analysis | High conversion efficiency, minimal DNA degradation | EZ DNA Methylation kits, EM-seq kits |
| Target enrichment systems | Selection of cancer-relevant genomic regions | Hybrid capture vs. amplicon-based approaches | Illumina TruSight Oncology, IDT xGen Pan-Cancer Panel |
| Methylation arrays | Genome-wide methylation profiling | Fixed content but cost-effective for large studies | Illumina Infinium MethylationEPIC v2.0 (930,000 CpGs) |
| UMI adapters | Unique molecular identifiers | Essential for distinguishing PCR duplicates from true molecules | Integrated DNA Technologies, Twist Bioscience |
| Methylation-sensitive digital PCR | Absolute quantification of methylation | High sensitivity for validation studies | Bio-Rad ddPCR methylation assays, Qiagen digital PCR |
| Bioinformatics pipelines | Methylation data analysis | Bisulfite alignment, quality control, visualization | Bismark, MethylKit, SeSAMe, NanoMethPhase |
The successful validation of epigenetic biomarkers for early cancer detection remains contingent on overcoming persistent sensitivity limitations rooted in both biological constraints and technological boundaries. The extremely low abundance of tumor-derived material in early-stage disease creates a fundamental detection challenge that current technologies struggle to overcome with sufficient reliability for population screening. However, emerging solutions—including bisulfite-free sequencing, multi-analyte integration, artificial intelligence, and optimized liquid biopsy sources—demonstrate promising pathways toward the required sensitivity thresholds.
Future progress will depend on standardized experimental protocols that minimize pre-analytical variability, validated multi-omics integration frameworks, and transparent AI algorithms that maintain clinical interpretability. The research community must prioritize methodological rigor and independent validation across diverse populations to ensure that sensitivity claims translate to real-world clinical impact. As these technological and analytical advances mature, the vision of detecting cancers at their earliest, most treatable stages through epigenetic biomarkers moves progressively closer to clinical realization.
The successful translation of epigenetic biomarkers from research discoveries into clinically viable assays for early cancer detection hinges on overcoming significant challenges in standardization and reproducibility. In biomedical research, a lack of reproducibility has had tangible consequences, including the halt of cancer clinical trials when key molecular signatures used for decision-making could not be independently validated [108]. The fundamental requirements for robust clinical assays include both analytical validation (accuracy, precision, sensitivity, specificity) and clinical validation (ability to predict clinical outcomes) [109]. For epigenetic biomarkers in particular, which include DNA methylation patterns, histone modifications, and non-coding RNAs, the path to clinical implementation requires rigorous standardization across multiple domains to ensure results are comparable within and between laboratories [18] [23].
Epigenetic Biomarkers: Promise and Challenges in Cancer Detection
DNA Methylation Biomarkers in Oncology
DNA methylation represents one of the most studied and robust epigenetic marks in cancer diagnostics [23]. Aberrant DNA methylation patterns are early events in carcinogenesis and include both global hypomethylation (leading to oncogene activation and genomic instability) and localized hypermethylation at specific CpG islands (leading to silencing of tumor suppressor genes) [17] [2]. The stability of DNA methylation patterns and their detectability in various bodily fluids makes them particularly attractive for clinical assay development [17].
Several DNA methylation biomarkers have already transitioned to clinical use. The SEPT9 blood test for colorectal cancer screening and MGMT promoter methylation testing for predicting response to temozolomide in glioblastoma represent pioneering examples of clinically implemented epigenetic biomarkers [18] [2]. The plasma-based SEPT9 methylation assay demonstrates a pooled sensitivity of 0.71 and specificity of 0.92 for colorectal cancer detection, though its ability to identify precancerous lesions remains limited [2]. MGMT promoter methylation testing has become a standard component in the diagnostic workup for glioblastoma patients, with approximately 40% of gliomas exhibiting this epigenetic alteration [18].
Analytical Challenges in Epigenetic Biomarker Implementation
Despite the promising potential of epigenetic biomarkers, several analytical challenges impede their widespread clinical adoption:
- Reproducibility issues: Biomarker assays that yield different results across settings or experiments lead to inconsistent findings, undermining clinical utility [109]
- Standardization gaps: Lack of standardized protocols for measuring and reporting biomarkers complicates comparison across studies [109]
- Sample limitations: Liquid biopsies contain minimal circulating tumor DNA, especially in early-stage disease, requiring highly sensitive detection methods [85]
- Technical variability: Differences in sample preparation, reagent batches, instrumentation, and data analysis introduce variability [108] [110]
Comparative Analysis of Epigenetic Detection Platforms
Analytical Performance of Methylation Detection Techniques
Table 1: Comparison of DNA Methylation Detection Methodologies
| Method Category | Specific Techniques | Resolution | Throughput | Key Applications | Limitations |
|---|---|---|---|---|---|
| High-Throughput | WGBS, RRBS, Methylation arrays (450K, 850K) | Single-base to genome-wide | High | Discovery, biomarker identification | Higher cost, computational complexity |
| Region-Specific | (q)MSP, Bisulfite pyrosequencing, MS-HRM | Single CpG to gene-specific | Medium to high | Clinical validation, diagnostic assays | Limited scope, primer design challenges |
| Direct Methylation | Nanopore sequencing, SMRT sequencing | Single-molecule | Medium | Long-read analysis, modification detection | Emerging technology, standardization ongoing |
| Bisulfite-Based | EPIC array, Targeted bisulfite sequencing | Single-base to targeted regions | Medium to high | EWAS, validation studies | DNA degradation, conversion biases |
Clinical Performance of Validated Methylation Biomarkers
Table 2: Clinically Implemented or Advanced DNA Methylation Biomarkers in Oncology
| Biomarker | Cancer Type | Sample Type | Clinical Utility | Performance Metrics | Regulatory Status |
|---|---|---|---|---|---|
| SEPT9 | Colorectal | Blood | Screening, early detection | Sensitivity: 0.71, Specificity: 0.92 [2] | FDA-approved |
| MGMT | Glioblastoma | FFPE tissue | Predictive (response to temozolomide) | Present in ~40% of gliomas [18] | Clinical guidelines |
| GSTP1 | Prostate | Tissue | Diagnostic | - | Clinical use |
| SHOX2/PTGER4 | Lung | Blood, plasma | Diagnostic, discrimination of malignant vs. non-malignant | - | Advanced development |
| Multi-target stool DNA | Colorectal | Stool | Screening | - | FDA-approved (Cologuard) |
Experimental Protocols for Epigenetic Analysis
Integrated Genetic-Epigenetic Analysis from Liquid Biopsies
Background: Liquid biopsies represent a minimally invasive approach for cancer detection and monitoring, but especially in early-stage disease, circulating tumor DNA (ctDNA) levels are very low [85]. Traditional approaches require splitting samples for separate genetic and epigenetic analyses, reducing the already limited material available for each assay [85].
Protocol: The Avida Duo target enrichment system (Agilent) enables simultaneous genetic and methylation analysis from the same DNA sample without PCR amplification that typically erases methylation markers [85].
Workflow:
- Sample Collection: Blood draw (typically 5-10 mL) collected in cell-stabilizing tubes
- Plasma Separation: Centrifugation at 1600× g for 10 minutes at room temperature
- cfDNA Extraction: Isolation using magnetic bead-based methods (e.g., Qiagen Circulating Nucleic Acid Kit)
- Library Preparation: Create pre-capture library without PCR amplification using the Avida Duo system
- Target Enrichment: Hybridization-based capture of targeted genomic regions
- Sequencing: Next-generation sequencing on platforms such as Illumina NovaSeq or NextSeq
- Data Analysis: Simultaneous assessment of genetic variants and methylation patterns
Key Advantages: This integrated approach effectively doubles the available material for analysis by eliminating the need for sample splitting, thereby increasing assay sensitivity [85]. The method also avoids bisulfite conversion, which can create bias in target enrichment efficiency and fragment integrity [85].
Integrated Workflow for Genetic and Epigenetic Analysis from Liquid Biopsies
Quality Control and Standardization in Flow Cytometry
Background: Flow cytometry represents another key technology in clinical cancer diagnostics, particularly for hematological malignancies, but suffers from significant interlaboratory variability [110].
Standardization Protocol:
- Sample Preparation: Implement standardized anticoagulant use, processing time (within 24-48 hours), and temperature control
- Instrument Calibration: Daily calibration using standardized fluorescent beads across all instruments in multicenter studies
- Antibody Panel Standardization: Use of pre-formatted, lyophilized antibody cocktails to minimize reagent variability
- Data Acquisition: Standardized instrument settings across platforms, including photomultiplier tube voltages and compensation matrices
- Automated Analysis: Implementation of machine learning approaches for automated gating to reduce subjective manual assessment
Validation Metrics: Successful standardization efforts, such as those for CD4+ T cell enumeration in HIV/AIDS, have achieved interlaboratory coefficients of variation of less than 10% [110]. International consortia including the EuroFlow consortium and Human Immunophenotyping Consortium (HIPC) have developed standardized panels and data analysis tools for specific applications including multiple myeloma and B-cell leukemia detection [110].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Epigenetic Biomarker Development
| Reagent/Material | Function | Examples/Specifications |
|---|---|---|
| Bisulfite Conversion Kits | Chemical conversion of unmethylated cytosines to uracils | EZ DNA Methylation kits (Zymo Research), MethylEdge Bisulfite Conversion System (Promega) |
| Methylation-Specific PCR Reagents | Amplification and detection of methylation patterns | MSP primers, qMSP probes, optimized buffer systems |
| Target Enrichment Systems | Capture of targeted genomic regions for sequencing | Avida Duo system (Agilent), hybridization capture probes |
| cfDNA Extraction Kits | Isolation of cell-free DNA from plasma/serum | Qiagen Circulating Nucleic Acid Kit, MagMAX Cell-Free DNA Isolation Kit |
| DNA Methylation Standards | Controls for assay validation and quantification | Fully methylated/unmethylated DNA controls, synthetic spike-in controls |
| Methylation Arrays | Genome-wide methylation profiling | Illumina EPIC array, Infinium Methylation arrays |
| Next-Generation Sequencing Kits | Library preparation and sequencing | Illumina DNA Prep kits, Swift Biosciences Accel-NGS Methyl-Seq DNA Library Kit |
The establishment of robust clinical assays for epigenetic biomarkers in early cancer detection requires a multifaceted approach addressing pre-analytical, analytical, and post-analytical variables. Key considerations for advancing the field include:
- Adoption of standardized protocols for sample processing, data generation, and analysis across laboratories
- Implementation of reference materials and controls to enable interlaboratory comparability
- Development of integrated analysis platforms that maximize information yield from limited samples
- Rigorous validation through prospective studies following established frameworks for biomarker qualification [23]
International consortia and collaborative efforts play a crucial role in developing the standardized reagents, protocols, and analysis tools needed to advance epigenetic biomarkers from research discoveries to clinically impactful assays that can improve early cancer detection and patient outcomes [110] [23].
Validation Frameworks and Performance Assessment of Epigenetic Biomarkers
Analytical validation is a critical, non-negotiable prerequisite for the clinical translation of any diagnostic biomarker. For epigenetic biomarkers in cancer early detection, it formally establishes the performance characteristics of an assay—specifically its sensitivity, specificity, and reproducibility—providing researchers and clinicians with confidence in the reliability of its results. This process ensures that the test robustly and consistently measures the intended epigenetic alterations, such as DNA methylation changes, across different sample batches, operators, and laboratory environments. In the context of cancer early detection, where biomarkers often must identify subtle signals from minimal tumor DNA within a high background of normal cell-free DNA, rigorous analytical validation becomes the foundation for clinical validity and eventual utility [5].
The transition of epigenetic biomarkers from research discoveries to clinically implemented tools has been notably limited, despite a substantial publication record [5]. This translational gap frequently stems from inadequate analytical validation, underscoring its paramount importance. This guide objectively compares the analytical performance data of various epigenetic biomarker approaches, focusing on DNA methylation-based technologies that are advancing toward clinical application. By presenting structured experimental data and methodologies, we aim to provide a clear framework for evaluating and benchmarking analytical validation in epigenetic cancer diagnostics.
Comparative Performance of Epigenetic Biomarker Assays
The performance of epigenetic biomarkers varies significantly based on technology, analyte, and cancer type. The following tables summarize key analytical validation metrics reported in recent studies for single-cancer and multi-cancer early detection tests.
Table 1: Analytical Performance of Selected Single-Cancer DNA Methylation Biomarker Tests
| Cancer Type | Methylation Biomarker(s) | Sample Type | Sensitivity | Specificity | Detection Technology |
|---|---|---|---|---|---|
| Colorectal Cancer | SDC2, SFRP2 [20] | Feces, Blood | 86.4% [20] | 90.7% [20] | Real-time PCR with fluorescent probe [20] |
| Breast Cancer | 15-marker ctDNA panel [20] | Blood (ctDNA) | AUC of 0.971 [20] | - | Whole-genome bisulfite sequencing [20] |
| Breast Cancer | TRDJ3, PLXNA4, KLRD1, KLRK1 [20] | Peripheral Blood Mononuclear Cells (PBMCs) | 93.2% [20] | 90.4% [20] | Targeted bisulfite sequencing, Pyrosequencing [20] |
| Esophageal SCC | 12-methylated CpG site panel [20] | Tissue | AUC of 96.6% [20] | - | 450K Microarray [20] |
| Bladder Cancer | CFTR, SALL3, TWIST1 [20] | Urine | Reported High Sensitivity [20] | - | Pyrosequencing [20] |
Table 2: Performance of Multi-Cancer Early Detection (MCED) Tests
| Test Name / Technology | Target Analytes | Number of Cancers Detected | Reported Overall Sensitivity | Reported Overall Specificity | Key Technology |
|---|---|---|---|---|---|
| GRAIL's Galleri [111] | ctDNA Methylation Patterns | >50 types [111] | Varies by stage [111] | >99% [111] | Targeted Methylation Sequencing & ML [111] |
| CancerSEEK [111] | Gene Mutations & Protein Biomarkers | 8 types [111] | - | - | NGS & Protein Immunoassays [111] |
| EpiSwitchCFS (for ME/CFS) [112] | 3D Chromosome Conformations (CCs) | N/A (Non-cancer diagnostic) | 92% [112] | 98% [112] | EpiSwitch Microarray & ML [112] |
Experimental Protocols for Key Epigenetic Technologies
Targeted Bisulfite Sequencing for DNA Methylation Analysis
This methodology is widely used for validating DNA methylation biomarkers due to its high sensitivity and quantitative accuracy.
Core Workflow:
- DNA Extraction and Bisulfite Conversion: Genomic DNA is extracted from the sample (e.g., plasma, tissue, PBMCs) using commercial kits. The DNA is then treated with sodium bisulfite, which deaminates unmethylated cytosines to uracils, while methylated cytosines remain unchanged [20]. This conversion is the critical step that allows for the discrimination of methylation status at single-base resolution.
- Targeted PCR Amplification: Bisulfite-converted DNA is amplified using primers designed specifically for regions of interest (e.g., promoter CpG islands of tumor suppressor genes). The PCR is often performed in a quantitative or digital PCR format to enable precise quantification [20] [5].
- Sequencing and Analysis: The amplified products are sequenced using next-generation sequencing (NGS) platforms. Bioinformatic pipelines then align the sequences and calculate the methylation percentage at each CpG site by comparing the ratio of C (methylated) to T (unmethylated) reads [20].
Key Considerations for Validation:
- Sensitivity: Must be sufficient to detect low allele frequencies of methylated ctDNA in a background of normal cfDNA. Digital PCR and NGS are favored for their ability to detect rare methylated molecules [5].
- Reproducibility: Inter-assay and intra-assay precision must be demonstrated across multiple runs, days, and operators. This includes consistency in bisulfite conversion efficiency, which can be monitored using spike-in controls [113].
Chromosome Conformation Capture (EpiSwitch) for 3D Genomic Profiling
This technology leverages changes in the 3D architecture of the genome as a diagnostic signature.
Core Workflow:
- Sample Fixation and DNA Extraction: Whole blood or PBMCs are fixed with crosslinking agents like formaldehyde or glyoxal to preserve the 3D structure of chromatin. Crosslinked DNA is then extracted and purified [112].
- Chromosome Conformation Capture: The DNA is digested with restriction enzymes, and the crosslinked fragments are ligated. This step preferentially joins DNA segments that are in close spatial proximity within the nucleus, forming unique DNA circles or "chromosome conformations" (CCs) [112].
- Microarray or Sequencing Analysis: The CCs are amplified and hybridized to a custom high-density microarray (e.g., EpiSwitch Explorer Array) or sequenced. Machine learning algorithms are then applied to identify a specific panel of CCs that serve as a diagnostic signature for a disease state [112].
Key Considerations for Validation:
- Specificity: The identified panel of CCs must be rigorously tested against relevant control cohorts to ensure the signature is disease-specific and not influenced by other confounding factors [112].
- Reproducibility: The fixation and ligation steps are critical and must be highly standardized to ensure consistent results across different sample batches [112].
Signaling Pathways and Experimental Workflows
The following diagrams illustrate the logical workflow for analytical validation and a key pathway often dysregulated in cancer and detected by epigenetic biomarkers.
Diagram 1: Analytical Validation Workflow. This flowchart outlines the key stages in the analytical validation process, from initial precision testing to final validation, ensuring an assay is robust and reliable. LOD: Limit of Detection; LOQ: Limit of Quantification.
Diagram 2: Key Pathways in Cancer Epigenetics. This diagram shows how chronic stress can lead to tumor suppressor gene silencing via DNA hypermethylation and parallel activation of pro-oncogenic JAK/STAT signaling, contributing to cancer development—a pathway detectable via methylation and chromatin profiling [112] [111].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development and validation of epigenetic biomarkers rely on a suite of specialized reagents and tools. The following table details key solutions used in the featured experiments.
Table 3: Key Research Reagent Solutions for Epigenetic Biomarker Validation
| Research Reagent / Solution | Function in Experimental Protocol | Specific Example / Note |
|---|---|---|
| Bisulfite Conversion Kits | Chemically converts unmethylated cytosine to uracil, enabling methylation status discrimination. | Critical for all bisulfite-based sequencing methods (e.g., WGBS, RRBS). Conversion efficiency must be monitored [20] [5]. |
| DNA Methylation Arrays | High-throughput profiling of methylation states at pre-defined CpG sites across the genome. | Illumina Infinium MethylationEPIC array used in EWAS; covers >850,000 CpG sites [114] [111]. |
| Methylation-Specific PCR Primers & Probes | For highly sensitive and specific amplification of methylated or unmethylated DNA sequences after bisulfite conversion. | Used in qPCR, ddPCR, and MethylLight assays for targeted validation [20]. |
| Cell-Free DNA Blood Collection Tubes | Stabilizes nucleases in blood samples to prevent degradation of cfDNA/ctDNA post-phlebotomy. | Essential for preserving the integrity of low-abundance ctDNA in liquid biopsy samples [5]. |
| Targeted Sequencing Panels | Custom panels for deep sequencing of specific genomic regions to detect low-frequency methylation events. | Used in tests like GRAIL's Galleri for MCED; allows high sensitivity at low cost per sample [111]. |
| Chromatin Fixation Reagents | Crosslinks proteins and DNA to preserve the 3D structure of chromatin for conformation capture assays. | Paraformaldehyde (PFA) and glyoxal are used in EpiSwitch technology [112]. |
| Unique Molecular Identifier (UMI) Adapters | Tags individual DNA molecules before PCR to correct for amplification bias and enable accurate quantification. | Crucial for reducing errors in NGS-based methylation and fragmentome analyses [115]. |
The analytical validation of epigenetic biomarkers for cancer early detection is a multifaceted and demanding process. As the comparative data and methodologies presented in this guide demonstrate, achieving high sensitivity and specificity requires careful selection of technology, sample type, and biomarker panel, complemented by rigorous and standardized experimental protocols. While DNA methylation remains the most advanced epigenetic marker in clinical translation, emerging areas like 3D chromatin architecture and fragmentomics, especially when powered by artificial intelligence, show significant promise for enhancing the accuracy of multi-cancer detection.
The future of this field hinges on overcoming key challenges, including the standardization of methods across laboratories, improving the detection of very early-stage cancers where ctDNA burden is minimal, and ensuring that validated assays are accessible and effective across diverse populations. A robust and transparent analytical validation framework is, and will remain, the critical first step in building the evidence base required to bring reliable epigenetic diagnostic tests from the research bench to the clinical bedside.
The validation of diagnostic and prognostic biomarkers represents a critical pathway in translational oncology research. For epigenetic biomarkers in early cancer detection, understanding the clinical validation metrics—Positive Predictive Value (PPV) and Negative Predictive Value (NPV)—is fundamental to assessing real-world utility. These predictive values move beyond intrinsic test characteristics to provide clinically actionable probabilities that inform decision-making for researchers, clinicians, and drug development professionals. This guide examines the foundational principles, calculation methodologies, and contextual factors governing PPV and NPV, with specific application to epigenetic biomarkers in oncology. Through comparative analysis of established epigenetic biomarkers and detailed experimental protocols, we provide a framework for evaluating clinical utility in cancer early detection research.
In the evaluation of diagnostic tests, particularly for early cancer detection, predictive values serve as crucial bridges between test results and clinical meaning. While sensitivity and specificity describe inherent test characteristics, PPV and NPV answer the clinically pressing questions: Given a positive test, what is the probability that the patient actually has the condition? Given a negative test, what is the probability that the patient is truly disease-free? [116] [117]. These conditional probabilities are foundational to clinical utility assessment as they directly impact patient management decisions.
The distinction between these metrics is fundamental. Sensitivity represents the proportion of true positives correctly identified by the test among all who actually have the disease, while PPV represents the proportion of true positives among all who test positive [117]. This distinction becomes critically important in translational research, where biomarkers must demonstrate not just analytical validity but clinical relevance. For epigenetic biomarkers in oncology, this translates to understanding whether a methylation signature or histone modification pattern truly predicts cancer presence or absence in specific clinical contexts [18] [17].
Foundational Principles and Calculations
Mathematical Formulations
PPV and NPV are derived from 2x2 contingency tables comparing index test results against a reference standard. The standard formulas for these metrics are [116] [118]:
PPV = True Positives / (True Positives + False Positives)
NPV = True Negatives / (True Negatives + False Negatives)
These values are most accurately estimated from cross-sectional studies or other population-based investigations where valid prevalence estimates can be obtained [118]. Predictive values can also be calculated using Bayesian principles incorporating prevalence, sensitivity, and specificity [116] [118]:
PPV = (Sensitivity × Prevalence) / [(Sensitivity × Prevalence) + (1 - Specificity) × (1 - Prevalence)]
NPV = [Specificity × (1 - Prevalence)] / [Specificity × (1 - Prevalence) + (1 - Sensitivity) × Prevalence]
Table 1: Worked Example of Predictive Value Calculations Using a Fecal Occult Blood Test for Bowel Cancer Detection
| Metric | Calculation | Result |
|---|---|---|
| Total population | 2,030 individuals | - |
| True positives | 20 cases | - |
| False positives | 180 cases | - |
| True negatives | 1,820 cases | - |
| False negatives | 10 cases | - |
| PPV | 20 / (20 + 180) | 10% |
| NPV | 1,820 / (1,820 + 10) | 99.5% |
| Sensitivity | 20 / (20 + 10) | 66.7% |
| Specificity | 1,820 / (1,820 + 180) | 91% |
| Prevalence | 30 / 2,030 | 1.48% |
The Prevalence Dependence of Predictive Values
Unlike sensitivity and specificity, PPV and NPV are profoundly influenced by disease prevalence in the tested population [116] [119] [120]. This dependence represents a critical consideration for researchers designing validation studies for epigenetic biomarkers.
The relationship follows predictable patterns: as prevalence increases, PPV increases while NPV decreases; as prevalence decreases, PPV decreases while NPV increases [119] [120]. This has direct implications for biomarker application across different clinical contexts. A test validated in a high-prevalence population (e.g., symptomatic patients) may perform differently when applied to a low-prevalence screening population (e.g., asymptomatic individuals) [121].
Table 2: Effect of Prevalence on Predictive Values for a Test with 90% Sensitivity and Specificity
| Prevalence | PPV | NPV |
|---|---|---|
| 1% | 8.3% | 99.9% |
| 10% | 50% | 99% |
| 20% | 69.2% | 97.3% |
| 50% | 90% | 90% |
This prevalence dependence creates particular challenges for early cancer detection, where target conditions are inherently rare in the general population. Even tests with excellent sensitivity and specificity may yield low PPV in screening contexts, necessitating careful consideration of target populations and confirmatory testing strategies [121] [120].
Clinical Utility Assessment Framework
Defining Clinical Utility
Clinical utility extends beyond diagnostic accuracy to encompass the practical value of a test in improving patient outcomes, informing treatment decisions, or providing other clinically actionable benefits [18] [23]. For epigenetic biomarkers in oncology, clinical utility assessment requires evaluating how test results influence clinical management and patient prognosis.
The five-phase framework for biomarker implementation provides a structured approach to establishing clinical utility [23]:
- Preclinical exploratory studies - Initial discovery of promising epigenetic markers
- Assessment in noninvasive samples - Validation in clinically relevant sample types
- Retrospective longitudinal studies - Evaluation of prognostic capabilities
- Prospective screening studies - Assessment in intended-use populations
- Prospective intervention studies - Demonstration of clinical outcome improvement
Managing Uncertainty in Predictive Values
A fundamental challenge in applying PPV and NPV lies in the inherent uncertainty of prevalence estimates, particularly for novel biomarkers or emerging diseases [121]. This uncertainty can be managed through robustness analysis, which examines how errors in prevalence estimates affect predictive value reliability [121].
Four key properties characterize this relationship [121]:
- Zeroing: Optimal PPV or NPV estimates have no robustness to uncertainty in prevalence
- Trade-off: Robustness increases as acceptable error increases
- Preference reversal: Suboptimal estimates may be more robust than putative optima
- Specificity-robustness antagonism: Robustness increases as specificity decreases
Figure 1: Relationship Between Test Characteristics, Prevalence, and Clinical Utility
Comparative Analysis of Epigenetic Biomarkers in Oncology
Epigenetic alterations, particularly DNA methylation changes, represent promising biomarkers for early cancer detection due to their stability, cancer-specific patterns, and detectability in liquid biopsies [18] [17] [85]. The clinical validation of these biomarkers requires rigorous assessment of their predictive values across different cancer types and clinical contexts.
Table 3: Comparative Performance of Established Epigenetic Biomarkers in Oncology
| Biomarker | Cancer Type | Clinical Application | PPV/NPV Data | Sample Type |
|---|---|---|---|---|
| MGMT promoter methylation | Glioblastoma | Predicts response to temozolomide [18] | 40-50% of methylated tumors respond [18] | FFPE tissue |
| SEPT9 methylation | Colorectal | Early detection screening | PPV: ~50-60% in average-risk screening [18] | Blood plasma |
| GSTP1 methylation | Prostate | Diagnostic differentiation | High NPV for ruling out cancer [23] | Tissue, urine |
| MLH1 promoter methylation | Colorectal | Identifies sporadic vs. Lynch syndrome | >95% for sporadic CRC [18] | FFPE tissue |
| SHOX2/PTGER4 methylation | Lung | Malignant vs. benign discrimination | PPV: ~75% for lung cancer [17] | Blood plasma |
MGMT Promoter Methylation in Glioblastoma
MGMT (O6-methylguanine-DNA methyltransferase) promoter methylation represents one of the most clinically validated epigenetic biomarkers in oncology [18]. This biomarker demonstrates both prognostic and predictive utility, with methylated tumors showing better response to temozolomide chemotherapy [18] [23].
Clinical validation established that approximately 40% of glioblastomas exhibit MGMT promoter methylation, with these patients demonstrating significantly improved overall survival when treated with temozolomide [18]. The predictive capacity of this biomarker has made it standard practice in therapeutic algorithms for glioma, directly influencing treatment decisions [18].
SEPT9 Methylation for Colorectal Cancer Detection
The SEPT9 methylated DNA test represents a significant advancement in non-invasive colorectal cancer screening [18]. Validated in multiple large cohorts, this blood-based test demonstrates the application of epigenetic biomarkers in early detection contexts where predictive values must be interpreted in light of disease prevalence.
In average-risk screening populations with prevalence around 0.5-1%, the test maintains PPV of approximately 50-60%, facilitating the identification of asymptomatic individuals who require colonoscopy confirmation [18]. This balance between sensitivity and specificity optimizes predictive values for the screening context, minimizing false positives while maintaining detection capability.
Experimental Protocols for Predictive Value Validation
Diagnostic Accuracy Study Design
Robust validation of predictive values requires carefully designed diagnostic accuracy studies comparing index test results against an appropriate reference standard [117] [23]. The following protocol outlines key methodological considerations:
Subject Selection and Recruitment
- Define inclusion/exclusion criteria reflecting intended-use population
- Ensure adequate sample size with power calculation for target confidence intervals
- Implement consecutive or random sampling to minimize selection bias
- Stratify recruitment to represent relevant clinical subgroups
Reference Standard Application
- Apply reference standard (e.g., histopathology, clinical follow-up) to all participants
- Ensure blinded interpretation of reference standard independent of index test results
- Document reference standard procedures and criteria for positive/negative findings
Index Test Execution
- Perform index test (epigenetic biomarker assay) using predefined protocols
- Implement blinding to reference standard results and clinical data
- Establish reproducibility through repeat testing and inter-observer agreement assessment
DNA Methylation Analysis Techniques
Validation of epigenetic biomarkers requires specialized methodological approaches for DNA methylation analysis [18] [23]:
Bisulfite Conversion-Based Methods
- Bisulfite Pyrosequencing: Provides quantitative methylation data at single-base resolution with high accuracy and reproducibility. Optimal for analyzing specific CpG sites with known clinical significance [23].
- Quantitative Methylation-Specific PCR (qMSP): Offers high sensitivity for detecting rare methylated alleles in background of normal DNA. Ideal for liquid biopsy applications where target DNA is scarce [18] [23].
- Methylation-Sensitive High-Resolution Melting (MS-HRM): Enables detection of methylation differences without requiring bisulfite conversion. Useful for screening applications but less quantitative than other methods [23].
Next-Generation Sequencing Approaches
- Whole-Genome Bisulfite Sequencing: Provides comprehensive methylation profiling across the entire genome. Optimal for discovery phases but costly for clinical application [17].
- Targeted Bisulfite Sequencing: Focuses on specific genomic regions of interest, balancing comprehensive coverage with practical clinical utility [85].
- Bisulfite-Free Methods: Emerging approaches that preserve DNA integrity while detecting methylation status, potentially improving assay performance [85] [23].
Figure 2: Experimental Workflow for Epigenetic Biomarker Validation
Research Reagent Solutions for Predictive Value Assessment
Table 4: Essential Research Materials for Epigenetic Biomarker Validation Studies
| Reagent Category | Specific Examples | Research Function | Considerations for Predictive Value Studies |
|---|---|---|---|
| DNA Extraction Kits | QIAamp DNA Blood Mini Kit, DNeasy Blood & Tissue Kit | High-quality DNA extraction from various sample types | Yield and purity critical for downstream methylation analysis; optimize for sample type (tissue, blood, etc.) |
| Bisulfite Conversion Kits | EZ DNA Methylation Kit, Epitect Bisulfite Kit | Chemical conversion of unmethylated cytosines to uracils | Conversion efficiency directly impacts assay sensitivity and specificity |
| Methylation-Specific PCR Reagents | MSP primer sets, methylated and unmethylated controls | Amplification of methylation-specific sequences | Primer design critical for specificity; controls essential for assay validation |
| Pyrosequencing Systems | PyroMark Q系列, sequencing reagents | Quantitative methylation analysis at single-base resolution | Provides continuous methylation data for cutoff optimization |
| Next-Generation Sequencing Kits | Illumina Methylation EPIC array, targeted bisulfite sequencing panels | Genome-wide or targeted methylation profiling | Comprehensive coverage balanced against cost and analytical complexity |
| Reference Standard Materials | Characterized cell lines, synthetic controls, reference DNA | Assay calibration and quality control | Essential for establishing analytical validity and reproducibility |
The clinical validation of epigenetic biomarkers for early cancer detection requires meticulous assessment of PPV and NPV within the context of intended use. These predictive values serve as critical bridges between analytical performance and clinical utility, directly informing diagnostic and therapeutic decisions. The successful translation of epigenetic biomarkers into clinical practice depends on robust validation studies that account for prevalence effects, methodological standardization, and clinical context. As the field advances, integrating multivariable biomarker panels and refining liquid biopsy technologies will further enhance the predictive capacity of epigenetic markers, ultimately improving early cancer detection and patient outcomes.
The development of epigenetic biomarkers for early cancer detection represents a transformative frontier in oncology. However, the transition from promising research findings to clinically applicable tests requires rigorous validation strategies that ensure reliability across diverse patient populations. Multi-cohort validation has emerged as an essential methodology for establishing the generalizability and robustness of epigenetic biomarkers, addressing critical challenges such as biological heterogeneity, technical variability, and demographic diversity [35] [122]. This approach involves systematically evaluating biomarker performance across multiple independent patient cohorts, often from different geographic locations, healthcare settings, and population subgroups.
The fundamental strength of multi-cohort validation lies in its ability to distinguish between biomarkers that perform well within a specific, limited dataset and those that maintain diagnostic or prognostic accuracy across heterogeneous populations. This process is particularly crucial for epigenetic biomarkers based on DNA methylation patterns, which must demonstrate consistent performance despite variations in age, ethnicity, comorbidities, and environmental exposures [35] [8]. As the field advances toward liquid biopsy applications and multi-cancer early detection tests, establishing generalizability through comprehensive validation strategies becomes increasingly important for clinical translation and regulatory approval.
Comparative Analysis of Multi-Cohort Validation Approaches
Table 1: Comparison of Multi-Cohort Validation Strategies in Recent Cancer Epigenetics Studies
| Study Focus | Validation Cohorts | Key Biomarkers/Model | Performance Range (AUC) | Generalizability Assessment |
|---|---|---|---|---|
| Osteosarcoma Prognosis [123] [124] | Internal + 2 external (TARGET, GEO) | Epigenetic RSF Model (OLFML2B, ACTB, C1QB) | 0.832-0.929 (external); >0.997 (internal) | Demonstrated pan-cancer applicability across multiple cancer types |
| Prostate Cancer Diagnosis [125] | 5 cohorts (TCGA + 4 GEO) | 9-gene diagnostic panel (AOX1, B3GNT8, etc.) | Mean AUC: 0.91 across cohorts | Validated in cell lines and clinical plasma samples |
| Oral Squamous Cell Carcinoma [126] | Multiple GEO cohorts + TCGA | 3-gene signature (CXCL12, PLAU, PXDN) | Consistent prognostic stratification | Assessed across clinical subgroups and stages |
| Diabetes/Cancer Risk Prediction [8] | NHANES database | 30 epigenetic age acceleration biomarkers | Varied by disease and model | Evaluated contribution of different epigenetic biomarkers |
Table 2: Advantages and Limitations of Multi-Cohort Validation Approaches
| Validation Approach | Key Advantages | Potential Limitations | Suitable Context |
|---|---|---|---|
| Cross-institutional cohorts | Reduces site-specific biases; assesses technical variability | Potential batch effects; requires harmonization protocols | Early clinical development phase |
| Multi-omics integration [127] [128] | Captures complementary biological signals; enhances sensitivity | Increased complexity; higher computational requirements | Complex cancer types with heterogeneous biology |
| Prospective clinical cohorts [127] | Assesses real-world performance; includes pre-analytical variables | Time-consuming; expensive; requires large sample sizes | Pivotal validation before clinical implementation |
| Pan-cancer validation [123] | Demonstrates broad biological relevance; identifies universal markers | May miss cancer-specific nuances | Platform technology development |
Experimental Protocols for Multi-Cohort Validation
Epigenetic Random Survival Forest Model Development
The development and validation of the epigenetic random survival forest (RSF) model for osteosarcoma exemplifies a comprehensive multi-cohort approach [123] [124]. The experimental workflow comprised several critical stages:
Data Acquisition and Preprocessing: Researchers analyzed single-cell transcriptomes from five primary osteosarcoma samples from the Gene Expression Omnibus (GEO) database (GSE152048), specifically excluding recurrent and metastatic samples to minimize heterogeneity. They incorporated 801 epigenetics-related genes from the EpiFactors database and obtained additional validation datasets from the TARGET project (88 OS samples) and an independent GEO cohort (54 samples) [124].
Single-Cell Analysis Pipeline: Data preprocessing and quality control were performed using Seurat (version 5.0.0) in R, filtering cells based on quality metrics (200-5,000 genes, UMI counts <20,000, mitochondrial gene percentage <10%). Batch effects were corrected using the Harmony algorithm, followed by principal component analysis and UMAP dimensionality reduction. Cell type annotation was performed using the SingleR package with the Human Primary Cell Atlas reference, verified through canonical cell type-specific markers [124].
Machine Learning Framework: The RSF model was constructed using the curated epigenetic factors, with key predictive genes identified including OLFML2B, ACTB, and C1QB. Model performance was rigorously evaluated through internal validation and multiple external cohorts, assessing prognostic accuracy and pan-cancer applicability [123].
Figure 1: Multi-Cohort Validation Workflow for Epigenetic Biomarker Development
Integrated Machine Learning for Diagnostic Biomarker Discovery
The prostate cancer diagnostic study employed an extensive machine learning framework to identify robust biomarkers across multiple cohorts [125]:
Multi-Algorithm Integration: Researchers integrated 12 machine learning algorithms to construct 113 combinatorial models, screening for optimal diagnostic panels across five datasets from TCGA and GEO databases. Algorithms included Lasso, Ridge, Elastic Net, Stepglm, SVM, glmBoost, LDA, plsRglm, RandomForest, GBM, XGBoost, and NaiveBayes.
Feature Selection and Model Optimization: A two-step approach implemented feature selection using LASSO, Ridge, and Elastic Net, with optimal λ parameters determined through 10-fold cross-validation. Predictive modeling utilized SVM with RBF kernel, with hyperparameters optimized through grid search. RandomForest was built using 1000 decision trees, and XGBoost hyperparameters were fine-tuned using Bayesian optimization.
Biological and Clinical Validation: The optimal model was validated in prostate epithelial and cancer cell lines, followed by clinical validation in plasma samples from prostate cancer and benign prostatic hyperplasia patients. The final 9-gene diagnostic panel (including JPH4, RASL12, AOX1, SLC18A2, PDZRN4, P2RY2, B3GNT8, KCNQ5, and APOBEC3C) demonstrated superior diagnostic efficacy (mean AUC = 0.91) compared to PSA alone [125].
Multi-Omics Integration in Validation Frameworks
The PROMISE study (NCT04972201) exemplifies the emerging trend of multi-omics integration in validation frameworks for cancer detection [127]. This research explored a multi-omics liquid biopsy strategy for multi-cancer early detection across nine cancer types.
Experimental Design: The study prospectively collected blood samples from 1,706 participants (840 non-cancer; 866 cancer) randomly divided into training and validation sets. Researchers investigated complementarity between various omics modalities and carefully selected specific omics features for multimodal model construction.
Performance Comparison: The methylation-based classifier outperformed both mutation-based and protein-based classifiers. However, protein markers provided complementary value to the methylation-based classifier, as 14.0% of protein-positive samples were missed by methylation analysis alone [127].
Multimodal Integration: The multimodal classifier combining methylation and protein features exhibited improved sensitivity of 75.1% (95% CI: 69.3-80.3%) at the same specificity of 98.8%, with accuracy of top predicted origin of 73.1% (95% CI: 66.2-79.2%). Notably, the accuracy reached 100% in liver and ovarian cancers with negative results from the methylation-based classifier, demonstrating the critical value of multi-omics approaches for comprehensive validation [127].
Figure 2: Multi-Omics Integration in Validation Frameworks
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Multi-Cohort Epigenetic Studies
| Reagent/Platform | Function | Application in Validation |
|---|---|---|
| Illumina MethylationEPIC BeadChip [8] | Genome-wide DNA methylation profiling | Standardized methylation assessment across cohorts |
| EpiFactors Database [123] [124] | Curated collection of epigenetic regulators | Reference for epigenetic feature selection |
| Seurat Package (v5.0.0) [124] | Single-cell RNA sequencing analysis | Cell type identification and characterization |
| Harmony Algorithm [124] | Batch effect correction | Data integration across multiple cohorts |
| CIBERSORT/xCell [128] | Immune cell deconvolution | Tumor microenvironment analysis across populations |
| CellChat Package [124] | Cell-cell communication analysis | Intercellular signaling network mapping |
| Monocle2 [124] | Single-cell trajectory analysis | Developmental pseudotime reconstruction |
| WGCNA R Package [124] | Weighted gene co-expression network analysis | Identification of clinically relevant gene modules |
Analytical Considerations for Robust Multi-Cohort Validation
Addressing Technical and Biological Variability
Successful multi-cohort validation requires meticulous attention to technical and biological variability. The osteosarcoma study implemented rigorous batch effect correction using the Harmony algorithm to minimize technical variations across different samples [124]. This approach is particularly crucial when integrating datasets from different sequencing platforms, processing times, or laboratory protocols.
Biological variability must be addressed through appropriate cohort selection and stratification. The prostate cancer diagnostic study ensured robustness by validating findings across five independent cohorts with different demographic characteristics [125]. Similarly, the investigation of epigenetic biomarkers in diabetes and cancer risk utilized the NHANES database to assess performance across diverse population subgroups [8].
Statistical Frameworks for Generalizability Assessment
Advanced statistical frameworks are essential for quantifying generalizability in multi-cohort studies. Researchers should employ:
- Cross-validation Techniques: Implementation of k-fold cross-validation within discovery cohorts to assess model stability [125].
- Performance Metric Consistency: Evaluation of consistent performance across cohorts using AUC, sensitivity, specificity, and predictive values [123] [125].
- Feature Importance Analysis: Utilization of SHAP values or similar approaches to visualize the contribution of individual epigenetic biomarkers [8].
- Subgroup Analysis: Assessment of performance across clinical and demographic subgroups to identify potential biases or limitations [126].
Multi-cohort validation represents the gold standard for establishing the generalizability and clinical utility of epigenetic biomarkers in cancer detection and prognosis. The integration of diverse patient populations, standardized analytical protocols, and advanced computational approaches provides a robust framework for translating epigenetic discoveries into clinically applicable tools. As the field evolves, several emerging trends will shape future validation strategies.
Longitudinal Cohort Designs: Future studies will increasingly incorporate longitudinal sampling to assess biomarker dynamics during disease progression and treatment response [128]. This approach will be particularly valuable for monitoring minimal residual disease and early detection of recurrence.
Artificial Intelligence Integration: Advanced machine learning and deep learning algorithms will enhance the ability to identify complex, multi-modal epigenetic signatures that transcend single-biomarker limitations [35]. Explainable AI approaches will be crucial for clinical adoption and regulatory approval.
Standardization Initiatives: The development of consensus protocols for epigenetic biomarker validation will facilitate more systematic multi-center collaborations and accelerate clinical translation [5]. Standardized reporting frameworks will improve transparency and reproducibility across studies.
As these advancements converge, multi-cohort validation will continue to serve as the critical bridge between epigenetic biomarker discovery and genuine clinical impact, ultimately enabling more precise, personalized, and equitable cancer care across diverse patient populations.
The development of effective multi-cancer early detection (MCED) tests represents a paradigm shift in oncology, with the potential to significantly improve patient survival rates through earlier intervention [65] [78]. The selection of optimal biomarker types is fundamental to this endeavor, as it directly influences test sensitivity, specificity, and clinical utility. Currently, the field is dominated by three primary biomarker categories: epigenetic (notably DNA methylation patterns), genetic (such as somatic mutations in circulating tumor DNA), and protein (including circulating proteins and autoantibodies) [65] [129] [78].
Each biomarker class offers distinct advantages and faces unique challenges. Genetic mutations are canonical cancer drivers but can be heterogeneous, while proteins are often abundant but may lack specificity. Epigenetic alterations, particularly DNA methylation, provide a stable and pervasive record of cellular dysregulation, often occurring early in tumorigenesis [76] [105]. This review provides a comparative analysis of the performance characteristics of these biomarker classes, focusing on their application in early cancer detection within the broader context of validating epigenetic biomarkers for cancer research.
Performance Comparison of Biomarker Classes
Direct comparisons and hybrid approaches in recent studies reveal the relative strengths and weaknesses of each biomarker class. The table below summarizes key performance metrics and characteristics.
Table 1: Comparative Analysis of Biomarker Classes for Early Cancer Detection
| Feature | Epigenetic (DNA Methylation) | Genetic (Mutations, ctDNA) | Protein Biomarkers |
|---|---|---|---|
| Inherent Stability | Highly stable in blood, FFPE tissues, and other biospecimens [76] | ctDNA is fragmented and can be low abundance, especially in early-stage cancer [130] | Generally stable and abundant in serum/plasma [129] |
| Early Appearance in Carcinogenesis | Often precedes genetic changes, occurs in precancerous stages [105] | Typically accumulates as cancer develops and progresses | Variable; can appear early or late depending on the specific protein |
| Tissue of Origin (TOO) Identification | High accuracy due to tissue-specific methylation patterns [65] [131] | Limited without extensive profiling; can indicate origin for some mutations | Possible with specific protein panels; some tests show high TOO accuracy [129] |
| Analytical Sensitivity Requirement | High sensitivity needed, but patterns are consistent across regions [105] | Requires ultra-deep sequencing to find rare mutant molecules in a background of normal cfDNA [129] | Lower sensitivity required due to higher abundance of target proteins [129] |
| Multi-Cancer Detection Potential | High; pan-cancer methylation panels can detect >50 cancer types [65] [131] | Moderate; limited by the heterogeneity of driver mutations across cancer types | High; panels of cancer-associated proteins and antibodies can detect multiple cancers [129] |
| Representative Performance (Sensitivity/Specificity) | 51.5% sensitivity/99.5% specificity (Galleri test) [65]; 63.7% sensitivity/99.5% specificity (HarbingerHx) [131] | Sensitivity can be low for early-stage cancers; part of multi-modal tests like CancerSEEK (62% sensitivity/>99% specificity) [65] | Can achieve very high performance; one study reported 100% sensitivity/97% specificity for 5 cancers [129] |
Experimental Data from Integrated Assays
The performance of biomarker classes is best understood not in isolation, but through their integration in modern MCED tests. The following table synthesizes key experimental findings from recent studies and clinical trials, highlighting how different biomarkers contribute to overall test performance.
Table 2: Performance of Selected MCED Tests Utilizing Different Biomarker Classes
| Test Name (Company/Institution) | Primary Biomarker Class(es) | Key Experimental Findings | Clinical Context |
|---|---|---|---|
| Galleri (GRAIL) [65] | Epigenetic (Targeted Methylation Sequencing) | 51.5% sensitivity, 99.5% specificity across >50 cancer types. | Large-scale studies; demonstrates the broad detection potential of methylation. |
| HarbingerHx [131] | Epigenetic (Methylation + Machine Learning) | Achieved 63.7% sensitivity/99.5% specificity (PPV 54.8%) and 55.1% sensitivity/99.89% specificity (PPV 80.7%) in different analytical tiers. | CORE-HH study; highlights how novel bioinformatics can enhance methylation-based test performance. |
| Carcimun Test [130] | Protein (Conformational Changes) | 90.6% sensitivity, 98.2% specificity in cohort including inflammatory conditions. Effectively distinguished cancer from inflammation. | Prospective blinded study; demonstrates robustness of protein-based markers against inflammatory confounders. |
| Exact Sciences MCED Test [132] | Multi-target (Methylation + Protein) | Overall sensitivity 50.9% at 98.5% specificity. Sensitivity increased for later stages: 15.4% (Stage I) to 85.5% (Stage IV). | Large prospective study (n=6,352); shows real-world performance of a combined biomarker approach. |
| Protein-Based MCED (Kazmierczak et al.) [129] | Protein (xPKA activity, cancer-associated antibodies) | 100% sensitivity, 97% specificity across breast, lung, colorectal, ovarian, and pancreatic cancers; 100% detection of Stage I cancers. | Case-control study; illustrates the potential for very high early-stage sensitivity with protein panels. |
Detailed Experimental Protocols
Understanding the methodologies behind biomarker analysis is crucial for interpreting performance data. This section outlines standard and emerging protocols for analyzing each biomarker class.
Epigenetic Biomarker Analysis (DNA Methylation)
DNA methylation analysis typically relies on bisulfite conversion of DNA, where unmethylated cytosines are deaminated to uracils, while methylated cytosines remain unchanged. Subsequent analysis differentiates these states [105].
- Whole-Genome Bisulfite Sequencing (WGBS): This is the gold standard for comprehensive methylation profiling, providing single-base resolution across the entire genome. The workflow involves bisulfite conversion of DNA, library preparation, and deep next-generation sequencing (NGS). While highly informative, it requires high DNA input (≥100 ng) and is costly [105].
- Reduced Representation Bisulfite Sequencing (RRBS): This cost-effective method uses restriction enzymes to target CpG-rich regions (e.g., promoters, CpG islands), covering about 10% of CpGs. It requires less DNA input (≥30 ng) and is suitable for large-scale studies [105].
- Bisulfite-Free Methods: Newer techniques like Enzymatic Methylation Sequencing (EM-Seq) and Tet-Assisted Pyridine Borane Sequencing (TAPS) are gaining traction. They avoid the DNA degradation associated with bisulfite treatment, preserve DNA integrity better, and are highly suitable for low-input samples like liquid biopsies [105].
- Targeted Methylation Sequencing: Panels focusing on cancer-specific methylated regions are commonly used in commercial MCED tests (e.g., Galleri). This involves bisulfite conversion followed by targeted enrichment and NGS, offering a balance between depth, cost, and clinical applicability [105] [65].
Genetic Biomarker Analysis (Mutations, ctDNA)
The core challenge is detecting rare mutant alleles amidst a high background of wild-type cell-free DNA.
- Next-Generation Sequencing (NGS) Panels: Targeted NGS panels simultaneously sequence multiple cancer-associated genes (e.g., KRAS, TP53, EGFR). These can be designed with unique molecular identifiers (UMIs) to correct for sequencing errors and achieve high sensitivity [65] [78].
- Whole-Exome/Genome Sequencing (WES/WGS): These untargeted approaches sequence all protein-coding genes or the entire genome from ctDNA. While comprehensive, they are less sensitive for detecting low-frequency variants due to high cost and lower sequencing depth at any given locus [78].
- Digital PCR (dPCR) and Droplet Digital PCR (ddPCR): These methods partition a sample into thousands of individual reactions, allowing absolute quantification of specific mutations with very high sensitivity (down to 0.1%). They are ideal for validating specific mutations and monitoring minimal residual disease but are limited in the number of targets that can be interrogated simultaneously [105].
Protein Biomarker Analysis
Protein biomarkers are typically measured using immunoassays, which leverage the specific binding of antibodies to their target antigens.
- Enzyme-Linked Immunosorbent Assay (ELISA): This workhorse technique immobilizes a capture antibody on a plate. The sample is added, and the target antigen binds. A detection antibody with an enzyme conjugate is then used, which produces a colorimetric, fluorescent, or chemiluminescent signal upon adding a substrate. It is robust and widely used but generally low-plex [129] [11].
- Multiplex Immunoassays: Technologies such as planar arrays or bead-based systems (e.g., Luminex) allow for the simultaneous measurement of dozens of proteins from a small sample volume. This is crucial for developing multi-protein cancer signature panels [65] [129].
- Innovative Protein Conformation Assays: Some tests, like the Carcimun test, move beyond simple concentration measurements. They detect cancer-induced conformational changes in plasma proteins by measuring shifts in optical extinction under controlled physicochemical conditions (e.g., with acetic acid), offering a pan-cancer screening approach [130].
Visualizing Workflows and Relationships
MCED Biomarker Integration Workflow
The following diagram illustrates how different biomarker classes can be integrated into a single MCED assay workflow, from sample collection to final report.
Biomarker Class Characteristics
This diagram summarizes the core functional relationships and comparative advantages of the three biomarker classes within the context of early cancer detection.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development of biomarker-based assays requires a suite of specialized reagents and tools. The following table catalogues key solutions for researchers in this field.
Table 3: Essential Research Reagents and Materials for Biomarker Analysis
| Reagent/Material | Function | Primary Application |
|---|---|---|
| Bisulfite Conversion Kit | Chemically converts unmethylated cytosine to uracil for downstream methylation detection. | DNA Methylation Analysis [105] |
| MBD Domain or 5mC Antibody | Affinity-based capture or immunoprecipitation of methylated DNA for enrichment prior to sequencing. | Methylated DNA Capture (MeDIP-seq, MethylCap) [105] |
| Cell-free DNA Blood Collection Tubes | Preserves blood samples and stabilizes nucleated blood cells to prevent genomic DNA contamination of plasma cfDNA. | Liquid Biopsy; ctDNA Analysis [132] |
| Unique Molecular Identifiers (UMIs) | Short random nucleotide sequences added to DNA fragments during library prep to tag unique molecules and correct for PCR and sequencing errors. | Ultrasensitive NGS for ctDNA [78] |
| Methylation-Specific PCR (MS-PCR) Primers | Primers designed to amplify either the methylated or unmethylated sequence following bisulfite conversion. | Targeted Methylation Validation [105] |
| Multiplex Immunoassay Panel | A pre-configured set of antibodies for simultaneous quantification of multiple protein biomarkers from a single sample. | Protein Biomarker Discovery & Validation [129] |
| Next-Generation Sequencing Library Prep Kit | Prepares DNA fragments for sequencing by adding platform-specific adapters. Includes kits for bisulfite-converted or native DNA. | All NGS-based Genetic and Epigenetic Profiling [105] |
The comparative analysis of epigenetic, genetic, and protein biomarkers reveals a compelling narrative for the validation of epigenetic marks, particularly DNA methylation, in early cancer research. While each biomarker class has distinct merits, epigenetic biomarkers offer a unique combination of early appearance in tumorigenesis, high stability in clinical specimens, and superior ability to identify the tissue of origin [76] [105] [65].
However, the future of MCED does not lie in a single biomarker type. The most promising assays, as evidenced by recent clinical data, are multi-modal, integrating the complementary strengths of epigenetic, protein, and sometimes genetic biomarkers [132]. This integrated approach mitigates the limitations of any single class, enhancing overall sensitivity and specificity. For researchers and drug developers, this underscores the importance of a holistic biomarker strategy. The continued refinement of analytical protocols, including bisulfite-free sequencing and advanced bioinformatics, will further solidify the role of epigenetic biomarkers as a cornerstone of precision oncology and a fundamental component of the next generation of cancer diagnostic tools.
Real-world evidence (RWE) has emerged as a critical component in oncology research, bridging the gap between controlled clinical trials and routine clinical practice. Derived from real-world data (RWD)—healthcare information collected from electronic health records, medical claims, and disease registries—RWE provides clinical insights about the usage, benefits, and risks of medical products [133]. In the specific context of validating epigenetic biomarkers for early cancer detection, RWE studies offer unique advantages by generalizing findings from controlled settings to diverse patient populations, capturing the natural history of disease, and providing insights into long-term outcomes and safety surveillance [133]. This guide objectively compares the performance of retrospective studies and prospective clinical trials within the RWE spectrum, providing researchers with methodological frameworks for validating epigenetic biomarkers in cancer detection.
Comparative Frameworks: Retrospective Studies vs. Prospective Trials
The selection between retrospective and prospective real-world study designs involves strategic trade-offs across time, resources, data quality, and evidentiary strength. The table below summarizes the key operational and methodological differences:
| Characteristic | Retrospective Studies | Prospective Clinical Trials |
|---|---|---|
| Time Requirements | Shorter duration (analysis of existing data) [134] | Longer duration (months to years for follow-up) [135] [134] |
| Cost Considerations | More cost-effective (uses existing data) [134] | Expensive (requires patient recruitment and monitoring) [135] [134] |
| Data Collection | Historical data from records, claims, or registries [133] [134] | Active collection of new data tailored to research objectives [136] |
| Patient Population | Existing patients with documented outcomes [134] | Patients enrolled before outcome development [135] |
| Ethical Approval | Variable by region; may be exempt in some cases [137] | Generally required with informed consent [137] |
| Key Advantages | Efficient for rare diseases; multiple outcome analysis [134] [138] | Establishes temporal relationships; causal inference [135] [138] |
| Key Limitations | Vulnerable to missing data and biases (recall, selection) [134] [138] | Requires large subject pools; time-consuming [135] |
Experimental Applications in Epigenetic Biomarker Validation
For epigenetic biomarker validation, each study design addresses distinct research questions through different methodological approaches:
Retrospective Study Protocols typically utilize archived biospecimens and clinical data to conduct initial validation. A common approach involves:
- Biomarker Analysis: Using quantitative methylation-specific PCR (QMSP) or bisulfite pyrosequencing on stored tissue or liquid biopsy samples [32]. QMSP offers high sensitivity with minimal DNA input, while bisulfite pyrosequencing provides absolute methylation quantification [32].
- Outcome Correlation: Linking epigenetic markers (e.g., DNA methylation patterns) to clinical outcomes documented in electronic health records.
- Statistical Analysis: Assessing sensitivity, specificity, and predictive values of biomarkers for cancer detection.
Prospective Clinical Trial Designs for epigenetic biomarkers incorporate intentionally collected new data:
- Baseline Assessment: Enrolling participants before cancer diagnosis and collecting comprehensive biomarker data [135] [136].
- Longitudinal Monitoring: Following participants over time to observe development of cancer outcomes [135].
- Endpoint Evaluation: Comparing biomarker status with subsequent cancer diagnoses to establish predictive value [136].
The Prospective Clinico-Genomic (PCG) Study in metastatic non-small cell lung cancer exemplifies this approach, successfully enrolling approximately 1,000 patients across 24 sites by leveraging existing clinical infrastructure with minimal additional data collection burden [136].
Methodological Workflows and Experimental Protocols
Retrospective Validation Workflow
The following diagram illustrates the structured pathway for validating epigenetic biomarkers through retrospective study designs:
Prospective Validation Workflow
The prospective clinical trial approach follows a fundamentally different pathway focused on forward-looking data collection:
Essential Research Reagent Solutions for Epigenetic Biomarker Studies
The following table details key reagents and technologies essential for conducting epigenetic biomarker validation studies:
| Research Reagent/Tool | Primary Function | Application Context |
|---|---|---|
| Bisulfite Conversion Kits | Chemical treatment converting unmethylated cytosines to uracils while preserving methylated cytosines [32] | DNA methylation analysis in both retrospective and prospective designs |
| QMSP (Quantitative Methylation-Specific PCR) | Sensitive detection and quantification of methylated DNA sequences [32] | High-throughput biomarker validation with minimal DNA input |
| Bisulfite Pyrosequencing | Quantitative analysis providing absolute methylation levels at specific CpG sites [32] | Validation requiring precise methylation quantification across multiple CpGs |
| Next-Generation Sequencing (NGS) | Genome-wide methylation profiling through bisulfite-seq or methyl-CpG binding domain sequencing [79] [139] | Comprehensive discovery and validation of novel epigenetic biomarkers |
| Liquid Biopsy Platforms | Non-invasive collection of circulating tumor DNA (ctDNA) for methylation analysis [79] [78] | Prospective monitoring and early detection applications |
| Electronic Health Record (EHR) Systems | Structured data capture including clinical outcomes, treatments, and patient demographics [133] [136] | Retrospective data abstraction and prospective data collection |
Performance Metrics and Clinical Applications
Analytical Validation Metrics
Epigenetic biomarker validation requires rigorous assessment across multiple performance dimensions:
| Performance Metric | Retrospective Study Applications | Prospective Trial Applications |
|---|---|---|
| Sensitivity/Specificity | Initial calculation using historical cases and controls [78] | Validation in intended-use population with future outcomes [136] |
| Area Under Curve (AUC) | Discriminatory power assessment using stored specimens [78] | Real-world performance in asymptomatic populations [79] |
| Positive Predictive Value | Estimation based on historical disease prevalence [78] | Direct calculation from observed outcome incidence [79] |
| Clinical Utility | Association with documented clinical outcomes [32] | Demonstration of impact on early detection and survival [78] |
Representative Epigenetic Biomarkers in Clinical Development
Several epigenetic biomarkers illustrate the progression from retrospective validation to prospective application:
- MGMT Promoter Methylation: Initially validated retrospectively in glioblastoma patients, now used prospectively to predict response to alkylating agents [32].
- SEPT9 Methylation: Developed through retrospective testing of stored blood samples, now implemented in prospective colorectal cancer screening [78].
- Multi-Cancer Early Detection (MCED) Tests: Emerging biomarkers like those in the Galleri test undergoing large-scale prospective validation for detecting multiple cancer types simultaneously [79].
Integration Strategies and Future Directions
The most effective epigenetic biomarker validation programs strategically integrate both retrospective and prospective approaches. Initial retrospective analyses on existing biospecimen collections provide proof-of-concept and refine biomarker panels, while subsequent prospective studies generate the highest-quality evidence for clinical utility and regulatory approval [32] [136].
Future developments in real-world evidence generation for epigenetic biomarkers will likely focus on:
- Hybrid Study Designs: Combining retrospective data analysis with targeted prospective data collection to optimize efficiency and evidence strength [136].
- Artificial Intelligence Integration: Using machine learning to identify complex methylation patterns across multi-omics datasets [79] [139].
- Decentralized Approaches: Leveraging digital health technologies and liquid biopsies to enable more inclusive, efficient prospective studies [78].
This comparative guide demonstrates that both retrospective studies and prospective clinical trials offer complementary value in the validation pathway for epigenetic biomarkers in cancer early detection. Research programs that strategically employ both approaches throughout the development lifecycle will maximize efficiency while generating the robust evidence needed for clinical implementation.
The clinical adoption of epigenetic biomarkers for early cancer detection represents a frontier in precision oncology. These biomarkers, particularly DNA methylation patterns, offer a promising, minimally invasive solution for identifying cancer in its earliest stages. DNA methylation involves the addition of a methyl group to cytosine bases in CpG dinucleotides, regulating gene expression without altering the DNA sequence itself [5]. In cancer, these patterns are frequently altered, with tumors typically displaying both genome-wide hypomethylation and site-specific hypermethylation of CpG-rich gene promoters, often leading to the silencing of tumor suppressor genes [5]. The inherent stability of DNA and the fact that methylation alterations often emerge early in tumorigenesis make them ideal biomarker candidates [5] [140]. This guide objectively compares the performance of various epigenetic biomarker technologies and delineates the regulatory pathways for their clinical translation, providing researchers and drug development professionals with a framework for validating and securing approval for these innovative diagnostic tools.
Established vs. Emerging Epigenetic Biomarkers
The transition from traditional to novel epigenetic biomarkers marks a significant evolution in cancer diagnostics. The table below compares the key characteristics and performance metrics of established and emerging biomarker classes.
Table 1: Performance Comparison of Epigenetic Biomarker Classes for Early Cancer Detection
| Biomarker Class | Key Technology/Assay | Cancer Types Validated | Reported Sensitivity/Specificity | Clinical Readiness |
|---|---|---|---|---|
| Single-Gene Methylation | qPCR, dPCR (e.g., Epi proColon) | Colorectal Cancer | Varies by stage (e.g., ~68% sensitivity for stages I-II) [5] | FDA-approved; Clinical use |
| Methylation Panels | Microarrays, Targeted NGS (e.g., Shield) | Colorectal, Lung, Bladder | Superior to single-gene; e.g., >90% specificity for CRC [79] [5] | FDA Breakthrough Device; CLIA-Lab Use |
| Multi-Cancer Early Detection (MCED) | Whole-Genome Bisulfite Sequencing (e.g., Galleri) | >50 Cancer Types | Detects cancer signals with ~50% sensitivity overall [79] | Clinical Trials; LDT Availability |
| Fragmentomics/5hmC | Immunohistochemistry, Sequencing | Bladder, Glioblastoma | 5hmC loss associated with tumor aggressiveness in bladder cancer [33] | Research Phase |
The performance of these biomarkers is heavily influenced by the liquid biopsy source. Blood plasma is the most common source, but local fluids like urine for bladder cancer or bile for biliary tract cancers can offer higher biomarker concentration and reduced background noise, significantly improving detection accuracy [5]. A study on TERT mutations in bladder cancer, for instance, showed a sensitivity of 87% in urine versus only 7% in plasma [5].
FDA Regulatory Pathways for Biomarker Approval
Navigating the U.S. Food and Drug Administration (FDA) regulatory landscape is a critical step for clinical adoption. The FDA offers several pathways tailored to innovative diagnostics and therapies, each with distinct requirements and benefits.
Table 2: Key FDA Regulatory Pathways for Diagnostic Biomarkers and Bespoke Therapies
| Regulatory Pathway | Purpose & Eligibility | Key Requirements | Benefits for Developers |
|---|---|---|---|
| Premarket Approval (PMA) | Standard pathway for high-risk Class III devices (e.g., novel diagnostics) | Valid scientific evidence demonstrating safety and effectiveness from clinical studies [5] | Full market authorization for widespread clinical use |
| Breakthrough Device | Expedites development of devices for life-threatening/irreversible conditions | Demonstrate potential to address unmet medical need; more effective than existing alternatives [5] | Interactive communication with FDA; prioritized review |
| Fast Track Designation | Expedites development and review of drugs for serious conditions with unmet need | Preclinical/clinical data showing potential to address unmet need (e.g., for a drug-biomarker combination) [141] | Frequent FDA interactions; eligibility for Accelerated Approval |
| "Plausible Mechanism" Pathway | New pathway for bespoke therapies (e.g., CRISPR-based) for ultra-rare diseases [142] | Therapy directed at known biological cause; well-characterized historical data; confirmation of target engagement [142] | Expedited development and review for N-of-1 or small population therapies |
The Breakthrough Device designation has been particularly impactful for DNA methylation tests. For example, the multi-cancer early detection tests Galleri and OverC have received this designation, facilitating their development [5]. Similarly, the Fast Track designation has been granted to novel epigenetic therapies, such as ZEN-3694, a BET inhibitor for treating the aggressive NUT carcinoma, underscoring the FDA's role in accelerating targeted epigenetic agents [141].
Most recently, the FDA has proposed a novel "plausible mechanism" pathway to address the challenge of bespoke therapies for extremely rare genetic diseases. This pathway is designed for situations where traditional randomized trials are not feasible. It requires that the therapy targets the known biological cause of a disease and that developers provide well-characterized historical data on the disease's natural progression, along with confirmation that the treatment successfully engages its intended target [142].
Experimental Protocols for Biomarker Validation
The journey from discovery to clinical application requires rigorous validation. The following protocols outline the core methodologies for establishing the analytical and clinical validity of DNA methylation biomarkers.
Protocol 1: Genome-Scale Methylation Discovery and Analysis
This protocol is used for the unbiased discovery of novel methylation biomarkers, as demonstrated in studies on lung and colorectal cancer [33].
- Sample Collection and cfDNA Extraction: Collect peripheral blood in EDTA or cell-stabilizing tubes. Isolate cell-free DNA (cfDNA) from plasma using silica-membrane or magnetic bead-based kits, typically yielding 6-10 ng of cfDNA per sample [33].
- Library Preparation (cfRRBS): Perform cell-free Reduced Representation Bisulfite Sequencing (cfRRBS). Digest DNA with the MspI restriction enzyme, which cuts at CCGG sites, enriching for CpG-rich regions. Follow with end-repair, adapter ligation, and bisulfite conversion using a kit like the EZ DNA Methylation-Lightning Kit, which converts unmethylated cytosines to uracils while leaving methylated cytosines unchanged [33].
- Sequencing and Bioinformatic Analysis: Sequence the libraries on a high-throughput platform (e.g., Illumina). Process the raw data through a bioinformatics pipeline that includes:
- Alignment: Map bisulfite-converted reads to a reference genome using tools like Bismark or BSMAP.
- Methylation Calling: Calculate methylation levels at each CpG site as the percentage of reads showing a cytosine versus a thymine.
- Differential Analysis: Identify significantly hypermethylated or hypomethylated regions between case and control samples using statistical packages like
DSSormethylKitin R [33].
- Tissue of Origin Deconvolution: Apply deep-learning models to the methylation data to predict the tissue origin of the cfDNA, which is crucial for diagnosing cancer and guiding follow-up care [33].
Protocol 2: Targeted Methylation Validation and Assay Development
Once candidate biomarkers are identified, they must be validated in larger cohorts using targeted, cost-effective methods suitable for clinical use.
- Assay Design: Design PCR primers and probes specific for the methylated regions of interest. For quantitative analysis, Methylation-Specific PCR (qMSP) is commonly used.
- Digital PCR (dPCR) for Absolute Quantification: For high-sensitivity detection, use digital PCR. Partition the bisulfite-converted DNA sample into thousands of individual reactions. Perform PCR amplification with fluorescent probes specific for the methylated allele. Count the number of positive partitions to absolutely quantify the number of methylated template molecules, allowing for detection of very low allele frequencies (e.g., <0.1%) in a background of normal cfDNA [5].
- Analytical Validation: Establish the assay's limit of detection (LOD), precision (repeatability and reproducibility), and linearity using contrived samples and a large set of clinical specimens [5].
- Clinical Validation: Conduct a blinded case-control study to establish the clinical sensitivity and specificity of the biomarker panel for its intended use, such as distinguishing early-stage lung cancer patients from individuals with non-malignant respiratory illnesses [33].
Visualizing the Clinical Translation Workflow
The path from biomarker discovery to FDA approval and clinical adoption is a multi-stage process, summarized in the workflow below.
Figure 1: Biomarker Clinical Translation Workflow
The Scientist's Toolkit: Key Research Reagents and Solutions
Successful development and validation of epigenetic biomarkers rely on a suite of specialized reagents and technologies.
Table 3: Essential Research Reagent Solutions for Epigenetic Biomarker Development
| Category / Reagent | Specific Example | Function in Workflow |
|---|---|---|
| Sample Collection & Stabilization | Cell-free DNA BCT Tubes (Streck) | Preserves cfDNA profile by preventing white blood cell lysis during blood transport [5]. |
| Nucleic Acid Extraction | QIAamp Circulating Nucleic Acid Kit (Qiagen) | Silica-membrane based isolation of high-purity, short-fragment cfDNA from plasma [5]. |
| Bisulfite Conversion | EZ DNA Methylation-Lightning Kit (Zymo Research) | Rapid chemical conversion of unmethylated cytosine to uracil for downstream methylation analysis [33]. |
| Discovery Sequencing | Illumina MethylationEPIC BeadChip | Microarray for profiling ~850,000 CpG sites across the genome at a lower cost than WGBS [8]. |
| Targeted Detection | ddPCR Methylation Assays (Bio-Rad) | Ultrasensitive, absolute quantification of specific methylated DNA targets without the need for standard curves [5]. |
| Bioinformatics | Bismark Alignment Tool / methylKit R Package |
Aligns bisulfite-seq reads and performs differential methylation analysis and visualization [33]. |
The pathway for clinical adoption and FDA approval of epigenetic biomarkers is well-defined yet demanding. The evolving regulatory landscape, including the Breakthrough Device and "plausible mechanism" pathways, provides avenues to accelerate the delivery of these transformative tools to patients. Success hinges on a rigorous, multi-phase process—from robust genome-scale discovery and analytical validation in CLIA-certified labs to definitive clinical trials that demonstrate a clear benefit in patient outcomes. For researchers and developers, a deep understanding of both the technical requirements for biomarker validation and the nuances of the regulatory pathways is paramount to successfully integrating epigenetic biomarkers into the standard of care for early cancer detection.
The global burden of cancer continues to rise, with an estimated 20 million new cases and 9.7 million deaths reported in 2022 alone [79]. This escalating prevalence places tremendous strain on healthcare systems worldwide and underscores the urgent need for cost-effective early detection strategies. Epigenetic biomarkers, particularly DNA methylation signatures detectable through liquid biopsies, represent a transformative approach to cancer screening with significant potential for population-level implementation [5] [78]. The fundamental economic premise is that earlier cancer detection enables less invasive, more successful, and ultimately less expensive interventions, while simultaneously improving survival rates and quality of life [78].
The clinical rationale for this economic analysis stems from the current limitations in cancer screening. Many cancers, such as pancreatic and esophageal cancer, lack effective early detection methods, leading to diagnosis at advanced stages when treatment options are limited, costly, and less effective [79]. Even for cancers with established screening methods, limitations in sensitivity and specificity result in false positives, unnecessary invasive procedures, and associated costs [79]. DNA methylation biomarkers offer distinct advantages in this context, as methylation alterations often emerge early in tumorigenesis and remain stable throughout tumor evolution, making them particularly valuable for early detection [5]. The stability of DNA methylation patterns, combined with the relative enrichment of methylated DNA fragments in circulation, provides technical advantages that translate to improved reliability and potentially better cost-effectiveness profiles [5].
This analysis examines the economic validation of epigenetic biomarkers for population-level implementation, focusing on the cost-benefit considerations of DNA methylation-based screening tests compared to established methodologies. By synthesizing current evidence on test performance, implementation costs, and potential economic impacts, we provide a framework for evaluating the economic viability of these emerging technologies in real-world healthcare settings.
Comparative Performance Analysis of Screening Modalities
The economic value of any screening modality is fundamentally tied to its diagnostic performance characteristics. Table 1 summarizes the key performance metrics of emerging epigenetic biomarkers alongside traditional screening methods, highlighting the potential advantages of DNA methylation-based approaches.
Table 1: Performance Comparison of Cancer Screening Modalities
| Screening Method | Target Cancer(s) | Sensitivity Range | Specificity Range | Sample Type | Key Limitations |
|---|---|---|---|---|---|
| Multi-cancer DNA methylation tests | >50 cancer types [79] | Varies by cancer type and stage | ~90% for some tests [79] | Blood | False positives/negatives occur [79] |
| SEPT9 methylation test | Colorectal [20] [143] | 86.4% [20] | 90.7% [20] | Blood (plasma) | Lower sensitivity for precancerous lesions |
| SDC2 methylation test | Colorectal [20] [143] | High (specific values not provided) | High (specific values not provided) | Stool, Blood | Patient acceptance of fecal sampling [20] |
| Traditional PSA | Prostate [79] | Variable | Variable | Blood | Limited specificity, leads to overdiagnosis [79] |
| Traditional CA-125 | Ovarian [79] | Variable | Variable | Blood | Not cancer-specific, elevated in benign conditions [79] |
| Mammography | Breast | Not covered in search results | Not covered in search results | Tissue | Radiation exposure, variable sensitivity |
The performance advantages of DNA methylation biomarkers are particularly evident in direct comparative studies. For example, the ColonSecure study evaluating a DNA methylation test for colorectal cancer detection demonstrated superior sensitivity compared to conventional serum markers (CEA, CRP, and CA19-9) for diagnosing early-stage disease [20]. Similarly, DNA methylation biomarkers for breast cancer detection have demonstrated sensitivities of 93.2% and specificities of 90.4% in peripheral blood mononuclear cells (PBMCs), outperforming traditional protein biomarkers [20].
The economic implications of these performance characteristics are substantial. Higher specificity reduces false positives, thereby decreasing the costs associated with unnecessary follow-up procedures, additional testing, and patient anxiety. Higher sensitivity, particularly for early-stage cancers, can lead to detection at more treatable stages, potentially reducing late-stage treatment costs, which are typically 2-5 times higher than early-stage treatment costs.
Economic Modeling Framework and Key Metrics
Evaluating the cost-effectiveness of epigenetic biomarkers requires consideration of both direct and indirect economic factors. The framework for economic validation incorporates multiple dimensions, as illustrated in the following conceptual model:
Key economic metrics for evaluating epigenetic biomarkers include:
Incremental Cost-Effectiveness Ratio (ICER): Represents the additional cost per quality-adjusted life year (QALY) gained compared to existing screening strategies. The acceptable ICER threshold varies by healthcare system but typically ranges from $50,000 to $150,000 per QALY in high-income countries.
Test Performance Economics: The balance between sensitivity (ability to correctly identify cancer cases) and specificity (ability to correctly identify non-cancer cases) directly impacts economic outcomes through false-positive and false-negative rates [79].
Implementation Cost Structure: Includes development costs, equipment, reagents, personnel training, and infrastructure requirements. The epigenetics diagnostics market, valued at $15.5 billion in 2024 with kits and reagents representing the largest product segment at $7.6 billion, reflects the significant investment in these technologies [144].
Downstream Economic Impacts: Include reduced late-stage treatment costs, productivity gains from earlier return to work, and reduced caregiver burden. Early detection enables less invasive treatments, resulting in more effective disease management and improved patient outcomes with potentially lower costs [78].
Market Analysis and Implementation Cost Drivers
The rapidly expanding epigenetics diagnostics market provides important context for understanding the economic landscape. The global epigenetics diagnostics market was valued at $15.5 billion in 2024 and is projected to grow at a compound annual growth rate (CAGR) of 16.5% to reach $70.7 billion by 2034 [144]. This growth trajectory reflects both technological advancements and increasing clinical adoption of epigenetic testing methodologies.
Market segmentation analysis reveals several key trends with economic implications:
Oncology Dominance: The oncology diagnostics segment commanded a dominant 68.7% market share in 2024, propelled by demand for early and precise cancer detection using epigenetic markers [144].
Technology Segmentation: DNA methylation technologies represented the largest technology segment at $6.3 billion in 2024, projected to reach $28.5 billion by 2034 [144].
Regional Distribution: North America held the largest regional share (39.7%) in 2024, with the U.S. alone valued at $5.4 billion, reflecting robust healthcare infrastructure and high adoption of precision diagnostics [144].
Table 2: Key Cost Drivers in Epigenetic Biomarker Implementation
| Cost Category | Specific Components | Economic Considerations | Impact Level |
|---|---|---|---|
| Technology Development | Discovery research, clinical validation, regulatory approval | High initial investment required; economies of scale possible | High |
| Reagents and Consumables | Bisulfite conversion kits, PCR reagents, sequencing kits | Kits and reagents segment valued at $7.6 billion in 2024 [144] | High |
| Instrumentation and Equipment | NGS platforms, PCR systems, automated sample processing | High capital investment but amortizable over time | Medium-High |
| Personnel and Training | Specialized technicians, bioinformaticians, pathologists | Requires expertise in both molecular biology and data analysis | Medium |
| Infrastructure and Facilities | Laboratory space, computational resources, data storage | Varies significantly by region and healthcare setting | Medium |
| Regulatory and Compliance | FDA submissions, CLIA certification, quality control | Essential for clinical implementation and reimbursement | Medium |
The concentration of market share among leading companies - including Thermo Fisher Scientific, Illumina, QIAGEN, Agilent Technologies, and Roche Diagnostics, which collectively hold approximately 65% of the market - influences pricing structures and competitive dynamics [144]. This consolidation may impact implementation costs through economies of scale but could also potentially limit price competition in certain market segments.
Analytical Methodologies and Experimental Protocols
Robust experimental protocols are essential for generating reliable data for economic analyses of epigenetic biomarkers. The following workflow outlines a standardized approach for evaluating DNA methylation biomarkers:
Sample Collection and Processing Protocols
Standardized sample collection is critical for reproducible results. For blood-based DNA methylation tests, plasma is preferred over serum due to higher ctDNA enrichment and less contamination from genomic DNA from lysed cells [5]. Sample processing should occur within a narrow timeframe (typically within 2-6 hours of collection) to prevent DNA degradation, with centrifugation protocols optimized to isolate cell-free DNA [5]. For local cancers, site-specific samples often provide superior performance - urine for urological cancers, bile for biliary tract cancers, stool for colorectal cancer, and cerebrospinal fluid for brain tumors [5].
DNA Extraction and Bisulfite Conversion
Cell-free DNA extraction should utilize commercially available kits specifically validated for low-concentration samples. The quantity and quality of extracted DNA should be quantified using fluorometric methods rather than spectrophotometry due to superior accuracy with fragmented DNA. Bisulfite conversion represents a critical step that converts unmethylated cytosines to uracils while leaving methylated cytosines unchanged, enabling downstream discrimination of methylation status. Conversion efficiency should be monitored using control sequences with known methylation status [20].
Methylation Analysis Methods
The choice of analysis method depends on the application and required sensitivity:
- Whole-genome bisulfite sequencing (WGBS): Provides comprehensive methylome coverage but requires significant bioinformatic resources and higher DNA input [20].
- Reduced representation bisulfite sequencing (RRBS): Offers a cost-effective alternative that enriches for CpG-rich regions [20].
- Methylation-specific PCR: Highly sensitive for detecting specific methylation markers, with detection limits approaching 0.1% methylated alleles in a background of unmethylated DNA [143].
- Digital PCR: Provides absolute quantification of methylation status at specific loci without the need for standard curves, offering particular advantages for low-abundance targets [5].
- Microarray-based methods: Balance throughput and cost for analyzing predefined CpG sites, with the Illumina Infinium MethylationEPIC BeadChip covering approximately 850,000 CpG sites [145] [146].
Bioinformatic Analysis Pipeline
The analytical workflow typically includes:
- Quality control of sequencing data using FastQC or similar tools
- Adapter trimming and alignment to bisulfite-converted reference genomes
- Methylation calling and quantification at individual CpG sites
- Identification of differentially methylated regions (DMRs)
- Development of classification algorithms using machine learning approaches
- Validation in independent cohorts to assess generalizability
Essential Research Reagents and Technologies
The experimental protocols for epigenetic biomarker development require specialized reagents and technologies. Table 3 outlines key solutions and their applications in DNA methylation analysis.
Table 3: Essential Research Reagent Solutions for DNA Methylation Analysis
| Reagent/Technology | Primary Function | Key Considerations | Representative Vendors |
|---|---|---|---|
| Bisulfite Conversion Kits | Chemical conversion of unmethylated cytosine to uracil | Conversion efficiency critical; DNA degradation during process must be minimized | Zymo Research, Qiagen, Thermo Fisher |
| DNA Methylation Kits & Reagents | Locus-specific or genome-wide methylation analysis | Market valued at $7.6B in 2024; extensive validation required for clinical use [144] | Illumina, Roche, Agilent, Diagenode |
| Next-Generation Sequencing Platforms | High-throughput methylation profiling | Enables discovery of novel methylation markers; requires significant bioinformatics infrastructure | Illumina, PacBio, Element Biosciences |
| PCR/QPCR Reagents | Targeted methylation analysis | Must be optimized for bisulfite-converted templates; digital PCR offers superior quantification | Thermo Fisher, Bio-Rad, Roche |
| Methylation-Specific Antibodies | Enrichment-based methylation analysis (MeDIP) | Alternative to bisulfite conversion; preserves DNA integrity | Diagenode, Abcam, Merck Millipore |
| Bioinformatic Software | Data analysis, visualization, and interpretation | Critical for translating raw data into biological insights; AI/ML tools increasingly important | Open-source and commercial solutions |
The selection of appropriate reagents and technologies significantly impacts both the technical performance and economic aspects of epigenetic biomarker development. The dominance of kits and reagents in the product segment ($7.6 billion in 2024) reflects their fundamental role in epigenetic diagnostics workflows [144]. When establishing laboratory capabilities for DNA methylation analysis, researchers must balance performance requirements with cost considerations, particularly for population-level screening applications where scalability and cost-effectiveness are paramount.
The economic validation of epigenetic biomarkers for population-level implementation represents a critical step in translating promising technologies into clinically impactful screening tools. The current evidence suggests that DNA methylation-based biomarkers, particularly those detectable in liquid biopsies, offer performance characteristics that could support cost-effective population screening for multiple cancer types. The growing epigenetics diagnostics market, projected to reach $70.7 billion by 2034, reflects significant confidence in the clinical and economic potential of these technologies [144].
Key considerations for achieving economic viability at the population level include:
Demonstrated Clinical Utility: Beyond analytical performance, biomarkers must demonstrate impact on clinically relevant endpoints, including stage shift at diagnosis, reduction in cancer-specific mortality, and improvement in quality of life [79] [78].
Standardization and Automation: Reducing variability through standardized protocols and implementing automated processes can significantly improve reproducibility while reducing costs [5].
Appropriate Target Population Selection: Identifying populations with sufficiently high pre-test probability to ensure positive predictive value remains acceptable while maximizing detection rates [79].
Integration with Existing Care Pathways: Successful implementation requires efficient integration with current diagnostic and treatment pathways to minimize disruption and additional costs [78].
The ongoing development of multi-cancer early detection (MCED) tests, such as the Galleri test currently undergoing clinical trials, represents a particularly promising approach that could further enhance the economic value proposition of epigenetic biomarkers [79]. As these technologies continue to mature and evidence accumulates, epigenetic biomarkers are positioned to play an increasingly important role in economically viable, population-level cancer screening strategies that improve outcomes while managing healthcare costs.
Conclusion
The validation of epigenetic biomarkers represents a paradigm shift in early cancer detection, offering unprecedented opportunities for non-invasive, sensitive, and specific multi-cancer screening. The convergence of advanced profiling technologies, AI-driven analytics, and robust validation frameworks is accelerating the translation of epigenetic discoveries into clinically actionable tools. Future progress depends on addressing remaining challenges including standardization across platforms, validation in diverse populations, and integration of multi-omics approaches. As evidenced by emerging MCED tests and novel network biomarkers, successfully validated epigenetic biomarkers will fundamentally transform cancer screening paradigms, enable earlier therapeutic interventions, and ultimately improve patient outcomes through precision oncology. The next decade will likely see epigenetic biomarkers becoming standard tools in the clinical oncology arsenal, provided the field maintains rigorous validation standards while embracing innovative computational and technological advances.
References
- 1. Recent advances on gene-related DNA methylation in cancer ... [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-025-01884-2]
- 2. Advance and challenge of DNA methylation as cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12010373/]
- 3. The Role of DNA Methylation and DNA Methyltransferases ... [https://pubmed.ncbi.nlm.nih.gov/36350516/]
- 4. DNA Methylation Cancer Biomarkers: Translation to the Clinic [https://pmc.ncbi.nlm.nih.gov/articles/PMC6870840/]
- 5. a roadmap for DNA methylation biomarkers in liquid biopsies [https://www.nature.com/articles/s41388-025-03624-5]
- 6. DNA methylation landscapes of 1538 breast cancers ... [https://www.nature.com/articles/s41467-021-25661-w]
- 7. An overview of DNA methylation markers for early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10407555/]
- 8. The relationship between epigenetic biomarkers and ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1509458/full]
- 9. Genetic and epigenetic alterations as biomarkers for cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5543860/]
- 10. Epigenetic biomarkers for cancer diagnosis and prognosis [https://dailyreporter.esmo.org/molecular-analysis-for-precision-oncology-congress-map-2025/epigenetic-information-could-harbour-biomarkers-of-diagnosis-and-prognosis]
- 11. Current advances in detecting genetic and epigenetic ... [https://www.sciencedirect.com/science/article/pii/S0956566323005535]
- 12. Novel Approach May Improve Early Cancer Detection [https://news.feinberg.northwestern.edu/2025/09/23/novel-approach-may-improve-early-cancer-detection/]
- 13. Clinical validation of a DNA methylation biomarker ... [https://pubmed.ncbi.nlm.nih.gov/41175040/]
- 14. Epigenetic aging and DNA methylation biomarker changes ... [https://www.nature.com/articles/s41398-025-03683-y]
- 15. Emerging biomarkers for early cancer detection and diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359849/]
- 16. DNA hypomethylation in cancer cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2873040/]
- 17. Methylation biomarkers for early cancer detection and ... [https://www.sciencedirect.com/science/article/pii/S0959804922013089]
- 18. Prognostic and Predictive Epigenetic Biomarkers in Oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC6394434/]
- 19. DNA methylation profiles in cancer: functions, therapy, and ... [https://www.cancerbiomed.org/content/21/2/111]
- 20. Advancements in DNA methylation technologies and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12309559/]
- 21. Leveraging locus-specific epigenetic heterogeneity to improve ... [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-020-00939-w]
- 22. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3978461/]
- 23. Clinical promise and applications of epigenetic biomarkers [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-024-01806-8]
- 24. From DNA Methylation and Histone Modifications to Non- ... [https://www.mdpi.com/2076-3417/15/18/9940]
- 25. The Emergence of Liquid Biopsy and Epigenetic Markers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12433903/]
- 26. A histone-centric multi-omics study shows that increased ... [https://www.nature.com/articles/s41467-025-63745-z]
- 27. Targeting epigenetic regulators as a promising avenue to ... [https://www.nature.com/articles/s41392-025-02266-z]
- 28. CGE2025v13n2 [https://sophiapublisher.com/medscipublisher/CGE/Vol.13/No.2/39/]
- 29. Non‐coding RNAs as key player in cancer diagnosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12401177/]
- 30. Non-coding RNAs as novel biomarkers and therapeutic ... [https://www.frontiersin.org/journals/oncology-reviews/articles/10.3389/or.2025.1621144/full]
- 31. Computational identification and validation of non-coding ... [https://link.springer.com/article/10.1007/s10142-025-01747-2]
- 32. Clinical promise and applications of epigenetic biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC11682640/]
- 33. Clinical cancer epigenetics [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-025-01948-3]
- 34. Epigenetics and CTCs: New biomarkers and impact on ... [https://www.sciencedirect.com/science/article/abs/pii/S1937644824000418]
- 35. Artificial Intelligence in cancer epigenomics: a review on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12166640/]
- 36. 5-hydroxymethylcytosine analysis reveals stable ... [https://www.nature.com/articles/s42003-025-09017-4]
- 37. Systematic Epigenomic Analysis Reveals Chromatin States ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5473172/]
- 38. Epigenetic analysis for early cancer detection [https://www.nature.com/articles/d42473-020-00273-y]
- 39. Molecular basis of epigenetic regulation in cancer ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.885635/full]
- 40. The relationship between epigenetic biomarkers and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11968389/]
- 41. Profiling DNA Methylation Based on Next-Generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6162482/]
- 42. The impact of next-generation sequencing on the DNA ... [https://www.sciencedirect.com/science/article/pii/S1931524415004077]
- 43. Comparison of current methods for genome-wide DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12376410/]
- 44. Characterisation and reproducibility of the ... - BMC Genomics [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10027-5]
- 45. A Comprehensive Guide to DNA Methylation Sequencing ... [https://www.epicypher.com/resources/blog/a-comprehensive-guide-to-dna-methylation-sequencing-methods/]
- 46. Comparison of DNA methylation based classification ... [https://www.nature.com/articles/s41698-024-00718-3]
- 47. How to Validate DNA Methylation Sequencing Results [https://www.cd-genomics.com/resource-how-to-validate-dna-methylation-sequencing-results.html]
- 48. A Review of Circulating Tumor DNA (ctDNA) and the Liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12032849/]
- 49. Circulating tumor DNA to monitor treatment response in ... [https://www.nature.com/articles/s41698-025-00876-y]
- 50. Circulating tumor DNA predicts prognosis at different time ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1608872/full]
- 51. Clinical applications of cell-free DNA-based liquid biopsy ... [https://www.sciencedirect.com/science/article/pii/S1936523325002505]
- 52. Cell-free DNA testing for the detection and prognosis ... [https://www.nature.com/articles/s41467-025-61890-z]
- 53. Discovery and validation of cell-free DNA methylation ... [https://pubmed.ncbi.nlm.nih.gov/40524177/]
- 54. Circulating tumour DNA assays in focus - Nature [https://www.nature.com/articles/s44276-025-00181-y]
- 55. The Emergence of Liquid Biopsy and Epigenetic Markers [https://pubmed.ncbi.nlm.nih.gov/40959208/]
- 56. DNA methylation and machine learning - Clinical Epigenetics [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-025-01967-0]
- 57. Comparison of DNA methylation based classification models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11447224/]
- 58. Explainable artificial intelligence of DNA methylation ... [https://www.nature.com/articles/s41467-025-57078-0]
- 59. GUIDE: a prospective cohort study for blood-based early ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02367-x]
- 60. Enhancing the sensitivity of non-invasive cervical cancer ... [https://www.nature.com/articles/s41598-025-20050-5]
- 61. Accounting for differences between Infinium ... [https://www.life-science-alliance.org/content/8/9/e202403155]
- 62. Methods in DNA methylation array dataset analysis: A review [https://www.sciencedirect.com/science/article/pii/S2001037024001624]
- 63. GRAIL PATHFINDER 2 Results Show Galleri® Multi ... [https://grail.com/press-releases/grail-pathfinder-2-results-show-galleri-multi-cancer-early-detection-blood-test-increased-cancer-detection-more-than-seven-fold-when-added-to-uspstf-a-and-b-recommended-screenings/]
- 64. A large-scale, multi-centre validation study of an AI ... [https://www.nature.com/articles/s41698-025-01105-2]
- 65. the potential of multi-cancer early detection (MCED ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11785667/]
- 66. 肿瘤DNA甲基化标志物检测及临床应用专家共识(2024版) [https://www.caclp.com/article/?detail_12224.html]
- 67. Real-world data and clinical experience from over ... [https://www.nature.com/articles/s41467-025-64094-7]
- 68. Salivary biomarkers in cancer detection and management [https://pmc.ncbi.nlm.nih.gov/articles/PMC12614111/]
- 69. DNA Methylation in Urine and Feces Indicative of Eight Major ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11943902/]
- 70. An innovative PCR-free approach for DNA methylation ... [https://www.sciencedirect.com/science/article/abs/pii/S0925400523014132]
- 71. Stool shed cell transcriptomics mirrors tumor biology and ... [https://www.nature.com/articles/s41598-025-17411-5]
- 72. Johns Hopkins Investigators Create New Urine-based Test ... [https://www.hopkinsmedicine.org/news/newsroom/news-releases/2025/09/johns-hopkins-investigators-create-new-urine-based-test-to-id-prostate-cancers]
- 73. Advancing cancer detection with portable salivary sialic ... [https://www.nature.com/articles/s44328-024-00001-2]
- 74. Detection and Validation of Organic Metabolites in Urine for ... [https://pubmed.ncbi.nlm.nih.gov/39452927]
- 75. Utility of Stool-Based Tests for Colorectal Cancer Detection [https://pmc.ncbi.nlm.nih.gov/articles/PMC11353969/]
- 76. Epigenetic biomarkers: Current strategies and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6733278/]
- 77. Artificial Intelligence for Network-Based Oncomarker ... [https://www.mdpi.com/journal/cancers/special_issues/6T3943C7WW]
- 78. Emerging biomarkers for early cancer detection and diagnosis [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03003-6]
- 79. Cancer Biomarkers: Reflection on Recent Progress, Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468363/]
- 80. Quantitative comparison of DNA methylation assays for ... [https://www.nature.com/articles/nbt.3605]
- 81. Epigenomics Workshop 2025! - Read the Docs [https://nbis-workshop-epigenomics.readthedocs.io/]
- 82. 2025 VAI Epigenomics Workshop [https://www.vai.org/event/2025-vai-epigenomics-workshop/]
- 83. Benchmark of cellular deconvolution methods using a multi ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03552-3]
- 84. Community assessment of methods to deconvolve cellular ... [https://www.nature.com/articles/s41467-024-50618-0]
- 85. Epigenetics opens the door to faster cancer detection [https://www.nature.com/articles/d42473-024-00231-y]
- 86. Evaluating performance and applications of sample-wise cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11114236/]
- 87. Robustness and resilience of computational deconvolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159287/]
- 88. Comparison between 5 extractions methods in either plasma ... [https://cmbl.biomedcentral.com/articles/10.1186/s11658-023-00452-x]
- 89. Applying blood-derived epigenetic algorithms to saliva [https://pmc.ncbi.nlm.nih.gov/articles/PMC12016411/]
- 90. Promising applications of human-derived saliva biomarker ... [https://www.nature.com/articles/s41368-022-00209-w]
- 91. Salivary DNA Methylation Profiling: Aspects to Consider for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5644718/]
- 92. Comparison and Optimization of DNA Extraction Methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11932244/]
- 93. Comparison of three genomic DNA extraction methods to ... [https://plantmethods.biomedcentral.com/articles/10.1186/s13007-016-0152-4]
- 94. The impact of preanalytical variables on the analysis of cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11111958/]
- 95. Preanalytic Methodological Considerations and Sample ... [https://www.sciencedirect.com/science/article/pii/S1525157823000594]
- 96. Fresh frozen vs FFPE samples for next-generation ... [https://www.lexogen.com/blog/fresh-frozen-vs-ffpe-samples-for-next-generation-sequencing-studies/]
- 97. Estimation of age-related DNA degradation from formalin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5609301/]
- 98. Identification and validation of candidate epigenetic ... [https://www.nature.com/articles/srep35807]
- 99. DNA Quantity and Quality Comparisons between ... [https://www.mdpi.com/1718-7729/31/5/183]
- 100. Fresh and frozen cardiac tissue are comparable in DNA ... [https://www.nature.com/articles/s41598-023-43788-2]
- 101. Comparative Analysis of Aging-related Metabolic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527973/]
- 102. Cancer and Aging Biomarkers: Classification, Early ... [https://www.mdpi.com/2079-6374/15/11/737]
- 103. Clinical biomarker-based biological aging and risk of ... [https://www.nature.com/articles/s41416-023-02288-w]
- 104. Alzheimer blood biomarkers: practical guidelines for study ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11095038/]
- 105. DNA methylation in breast cancer: early detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12020129/]
- 106. A review of the use of tumour DNA methylation for breast ... [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-025-01922-z]
- 107. Role of circulating MicroRNAs in prostate cancer diagnosis ... [https://www.nature.com/articles/s41598-025-01373-9]
- 108. Comparability and reproducibility of biomedical data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3713713/]
- 109. Understanding biomarker validation, qualification... | TechTarget [https://www.techtarget.com/pharmalifesciences/feature/Understanding-biomarker-validation-qualification-challenges]
- 110. International Reproducibility Efforts in Clinical ... | Today's Clinical Lab [https://www.clinicallab.com/international-reproducibility-efforts-in-clinical-flow-cytometry-26666]
- 111. a review on advances in pan-cancer detection and precision ... [https://epigeneticsandchromatin.biomedcentral.com/articles/10.1186/s13072-025-00595-5]
- 112. Journal of Translational Medicine - BioMed Central [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07203-w]
- 113. Development and validation of peripheral blood DNA ... [https://pubmed.ncbi.nlm.nih.gov/40614748/]
- 114. Integrative DNA methylation and transcriptome analysis reveal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574575/]
- 115. Open chromatin-guided interpretable machine learning ... [https://www.nature.com/articles/s42003-025-08920-0]
- 116. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 117. Sensitivity, Specificity, and Predictive Values: Foundations, ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2017.00307/full]
- 118. Positive and negative predictive values [https://en.wikipedia.org/wiki/Positive_and_negative_predictive_values]
- 119. Statistics | Sensitivity, Specificity, PPV and NPV [https://geekymedics.com/sensitivity-specificity-ppv-and-npv/]
- 120. Understanding PPV and NPV in Healthcare Testing [https://harbinger-health.com/2024/09/26/understanding-ppv-and-npv-in-healthcare-testing-crucial-tools-for-diagnostic-accuracy/]
- 121. Interpreting PPV and NPV of Diagnostic Tests with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11294685/]
- 122. Clinically focused multi-cohort benchmarking as a tool for ... [https://www.nature.com/articles/s41598-022-16514-7]
- 123. Development and pan-cancer validation of an epigenetics ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1529525/full]
- 124. Development and pan-cancer validation of an epigenetics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11803151/]
- 125. Integrating multi-cohort machine learning and clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12016064/]
- 126. Development and Multi-cohort Validation of a Prognostic ... [https://www.sciencedirect.com/science/article/abs/pii/S2210776225001152]
- 127. Exploration of multi-omics liquid biopsy approaches for ... [https://www.sciencedirect.com/science/article/pii/S2666675825002796]
- 128. Beyond single biomarkers: multi-omics strategies to predict ... [https://link.springer.com/article/10.1007/s10238-025-01902-w]
- 129. A Protein-Based Blood Test for Multi-Cancer Diagnostics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561768/]
- 130. Evaluation of an innovative multi-cancer early detection test [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1520869/full]
- 131. Harbinger Health Unveils Promising New Data on Early ... [https://www.biospace.com/press-releases/harbinger-health-unveils-promising-new-data-on-early-cancer-detection-platform-at-aacr-2025]
- 132. Performance of a multi-target, multi-cancer early detection ... [https://www.medrxiv.org/content/10.1101/2025.08.24.25334244v1]
- 133. Introduction to real-world evidence studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8323556/]
- 134. Retrospective Studies: When Are They Used In Clinical Trials [https://www.allclinicaltrials.com/blog/what-is-a-retrospective-study]
- 135. Understanding Prospective Clinical Trials Dynamics [https://www.eclevarmedtech.com/en/understanding-prospective-clinical-trials-dynamics/]
- 136. Why prospective studies hold so much promise for clinical ... [https://resources.flatiron.com/clinical-research/why-prospective-real-world-studies-hold-so-much-promise-for-clinical-research]
- 137. Retrospective observational studies: Lights and shadows for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9686178/]
- 138. Overview of clinical study designs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11009715/]
- 139. Cancer epigenetics: from laboratory studies and clinical ... [https://www.nature.com/articles/s41420-024-01803-z]
- 140. Advance and challenge of DNA methylation as cancer ... [https://www.sciencedirect.com/science/article/pii/S2667005425000146]
- 141. FDA Fast Track Designation Accelerates Novel Therapy for ... [https://www.targetedonc.com/view/fda-fast-track-designation-accelerates-novel-therapy-for-nut-carcinoma]
- 142. FDA unveils new regulatory roadmap for bespoke drug ... [https://www.biopharmadive.com/news/fda-plausible-mechanism-pathway-n-of-1-crispr/805235/]
- 143. The Role of Epigenetic Biomarkers as Diagnostic ... [https://www.mdpi.com/2072-6694/17/16/2632]
- 144. Epigenetics Diagnostics Market Analysis 2025-2034 [https://www.globenewswire.com/news-release/2025/06/17/3100406/28124/en/Epigenetics-Diagnostics-Market-Analysis-2025-2034-Oncology-Led-with-68-7-Share-in-2024-Driven-by-Demand-for-Early-and-Precise-Cancer-Detection-Through-Epigenetic-Markers.html]
- 145. Epigenetic biomarkers of socioeconomic status are associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12041747/]
- 146. Associations between indicators of socioeconomic position ... [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-021-01189-0]