The Gut Microbiome as an Epigenetic Regulator: Molecular Mechanisms, Research Methodologies, and Therapeutic Applications
This article synthesizes current research on the dynamic interplay between the gut microbiome and the host epigenome, a field with profound implications for precision medicine.
The Gut Microbiome as an Epigenetic Regulator: Molecular Mechanisms, Research Methodologies, and Therapeutic Applications
Abstract
This article synthesizes current research on the dynamic interplay between the gut microbiome and the host epigenome, a field with profound implications for precision medicine. It explores foundational molecular mechanisms, including microbial metabolite signaling via short-chain fatty acids and one-carbon metabolism, and details advanced methodological approaches such as single-cell multi-omics and AI-driven modeling. For a specialist audience of researchers and drug development professionals, the content further addresses critical challenges in research standardization and troubleshooting, validates findings through disease-specific models in cardiology, neurology, and psychiatry, and evaluates comparative therapeutic strategies like live biotherapeutics and fecal microbiota transplantation. The synthesis aims to bridge foundational science with translational clinical applications.
Decoding the Dialogue: Foundational Mechanisms of the Microbiome-Epigenome Axis
The bidirectional epigenome-microbiome axis represents a dynamic and complex communication network between the host's epigenetic machinery and gut microbiota. This axis facilitates a continuous molecular dialogue where gut microorganisms influence host gene expression through epigenetic modifications, while the host's epigenome shapes the microbial ecosystem. This review synthesizes current mechanistic insights, profiling methodologies, and translational applications of this axis, framing it within the broader context of gut microbiome's impact on host epigenome research. We provide detailed experimental protocols, analytical frameworks, and visualization tools to equip researchers with practical methodologies for investigating this emerging field.
Core Concepts and Definitions
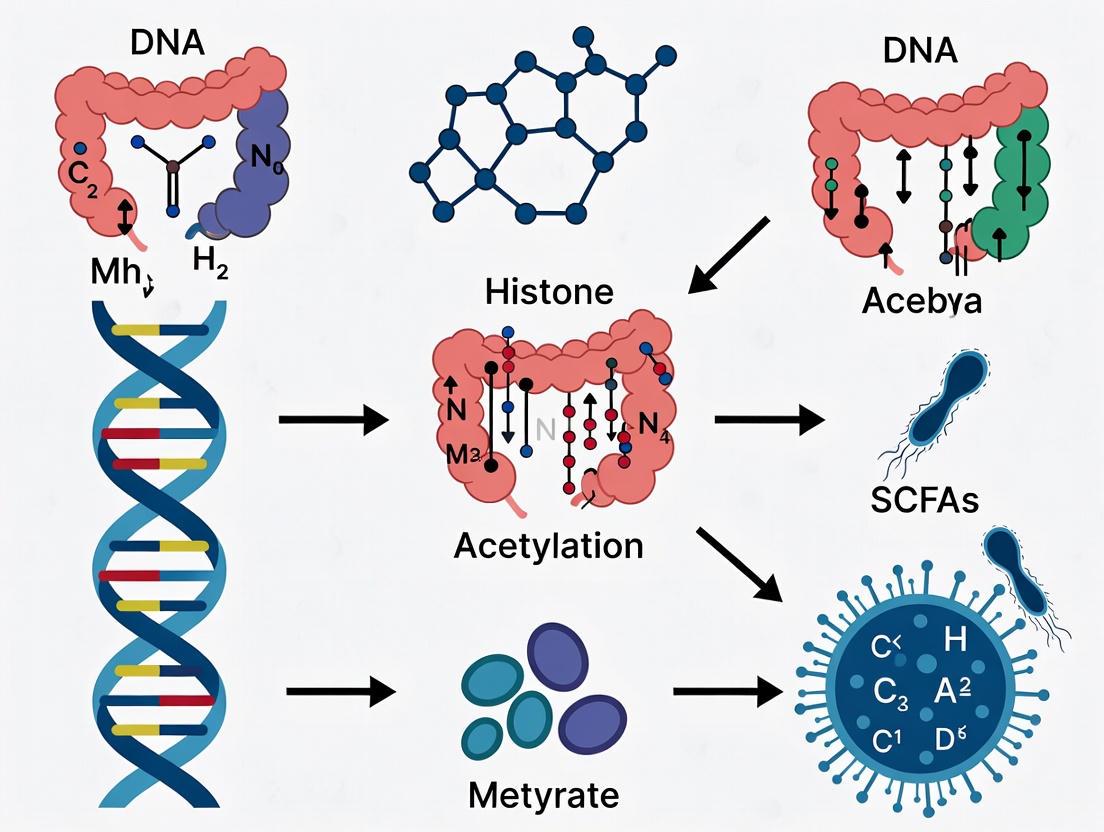
The epigenome-microbiome axis constitutes a bidirectional interface where environmental signals are translated into stable physiological responses. Epigenetics refers to heritable phenotypic changes that occur without alterations to the DNA sequence itself, primarily through three core mechanisms: DNA methylation, histone modifications, and non-coding RNA-associated gene silencing [1] [2]. The gut microbiome, a metabolically active consortium of bacteria, viruses, fungi, and other microorganisms, profoundly influences host physiology through this epigenetic interface [2].
This relationship is fundamentally bidirectional. While host epigenetic states can shape microbial composition, microbial communities reciprocally influence host epigenetic regulation through diet- and environment-dependent mechanisms [3] [2]. This reciprocity embeds environmentally induced variation, which may influence the adaptive evolution of host-microbe interactions within a holo-omic framework [3].
Molecular Mechanisms of Interaction
Microbial Metabolites as Epigenetic Regulators
Gut microbiota-derived metabolites (MDMs) form a diverse repertoire of molecules that uniquely interact with host epigenetic machinery, establishing what has been termed the "MDMs–epigenetic (MDME) axis" [4]. These metabolites function as key epigenetic modifiers through several conserved pathways.
Table 1: Key Microbial Metabolites and Their Epigenetic Functions
| Metabolite Class | Major Producing Bacteria | Epigenetic Mechanism | Biological Outcome |
|---|---|---|---|
| Short-Chain Fatty Acids (SCFAs) | Bacteroidetes, Firmicutes | Histone deacetylase (HDAC) inhibition; DNA methyltransferase modulation [1] [5] | Altered chromatin structure; gene expression changes in immunity/metabolism [2] |
| Folates | Bifidobacterium, Lactobacillus | Donors for one-carbon metabolism, influencing DNA methylation [1] | Regulation of DNA synthesis and repair |
| Polyamines | Wide range of gut bacteria | Modulators of histone and DNA methyltransferase activity [1] [2] | Cellular growth, differentiation |
| Choline/Trimethylamine N-oxide (TMAO) | Metabolic conversion by gut microbiota | Alters host cholesterol metabolism and gene methylation [5] | Impact on metabolic and inflammatory diseases |
Specific Epigenetic Mechanisms
DNA and RNA Methylation: Microbial signals can modulate both DNA and RNA methylation patterns. DNA methylation typically involves the addition of a methyl group to cytosine, forming 5-methylcytosine (5mC), which regulates gene expression. Similarly, RNA modifications like N6-methyladenosine (m6A) influence RNA stability and translation [1] [2]. Butyrate, a well-studied SCFA, acts as a potent inhibitor of histone deacetylases (HDACs), leading to increased histone acetylation and altered gene transcription [5].
Bacterial Epigenetics: Bacteria possess their own epigenetic systems, primarily involving DNA methylation—N6-methyladenine (6mA), N4-methylcytosine (4mC), and 5-methylcytosine (5mC)—which function within restriction-modification systems and influence virulence, host colonization, and antibiotic resistance [2] [6]. This adds a layer of complexity to the bidirectional communication.
Research Methodologies and Experimental Protocols
Profiling Host Epigenomic Modifications
Whole-Genome Bisulfite Sequencing (WGBS): This is the gold standard for mapping DNA methylation at single-base resolution.
- Protocol: Genomic DNA is treated with sodium bisulfite, which converts unmethylated cytosines to uracils, while methylated cytosines remain unchanged. The treated DNA is then sequenced, and the methylation status is determined by aligning sequencing reads to a reference genome and calculating the ratio of converted vs. unconverted cytosines at each CpG site [6].
- Applications: Ideal for generating comprehensive methylomes of host tissues in response to microbial changes.
Chromatin Immunoprecipitation Sequencing (ChIP-seq): This method identifies genome-wide histone modifications and transcription factor binding sites.
- Protocol: Cells or tissues are cross-linked with formaldehyde. Chromatin is sheared and immunoprecipitated with antibodies specific to a histone modification (e.g., H3K27ac). The immunoprecipitated DNA is then sequenced and mapped to the genome to identify enriched regions [2].
Analyzing Bacterial Methylomes and Composition
Single-Molecule Real-Time (SMRT) Sequencing: A third-generation sequencing technology that directly detects DNA methylation without chemical pre-treatment.
- Protocol: DNA is sequenced in real-time by observing the incorporation of fluorescently labeled nucleotides. The kinetics of nucleotide incorporation are altered by base modifications, allowing for the direct detection of 6mA, 4mC, and 5mC across the entire bacterial genome [6].
- Applications: Essential for characterizing the epigenomes of individual bacterial species within a community, identifying active restriction-modification systems, and understanding bacterial virulence.
Nanopore Sequencing: Another third-generation technology that detects methylation through changes in ionic current as DNA strands pass through a protein nanopore.
- Protocol: Native DNA is sequenced without amplification. Methylated bases cause characteristic disruptions in the current trace, which can be decoded using tools like Nanopolish or DeepSignal [6].
16S rRNA and Shotgun Metagenomic Sequencing: These methods are used to profile microbial community composition and functional potential.
- Protocol for 16S rRNA Sequencing: The 16S rRNA gene is amplified from community DNA and sequenced. Operational Taxonomic Units (OTUs) are clustered to identify taxa present.
- Protocol for Shotgun Metagenomics: Total community DNA is randomly sheared and sequenced, providing insights into both taxonomic composition and functional gene content.
Data Integration and Visualization
Visualizing Repeated Measures Microbiome Data: Longitudinal studies require specialized techniques to account for within-subject correlations.
- Method: A framework using Principal Coordinates Analysis (PCoA) adjusted via Linear Mixed Models (LMM) is recommended. The pairwise similarity matrix is calculated, and potential confounding effects are regressed out from each principal component of the similarity matrix using LMMs. The adjusted similarity matrix is then reconstructed from the model residuals for final PCoA visualization [7]. This effectively highlights microbial community variations related to the variable of interest while minimizing noise from confounders and repeated measures.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Epigenome-Microbiome Studies
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| S-adenosylmethionine (SAM) | Essential methyl donor for DNA and RNA methylation reactions in both host and bacteria [6]. | Stability and concentration are critical for in vitro methylation assays. |
| Sodium Bisulfite | Chemical agent for converting unmethylated cytosine to uracil in WGBS protocols [6]. | Reaction conditions must be optimized to prevent DNA degradation. |
| HDAC Inhibitors (e.g., Trichostatin A) | Positive controls for studying histone acetylation; mimic the effect of microbial butyrate [5]. | Specificity for different HDAC classes should be considered. |
| Type-Specific Histone Modification Antibodies | For ChIP-seq to map specific histone marks (e.g., H3K4me3, H3K27ac) in host cells. | Antibody specificity and lot-to-lot consistency are paramount. |
| Methyl-Sensitive Restriction Enzymes (MSREs) | For enzyme-based profiling of DNA methylation states at specific genomic loci [6]. | Limited to the recognition sites of available enzymes. |
| Cell-Free Transcription–Translation Systems | For in vitro recreation of specific DNA methylation patterns to overcome R-M barriers [6]. | Enables multiplex DNA methylation testing. |
| Germ-Free (GF) Mouse Models | Animals devoid of all microorganisms, essential for establishing causal roles of microbiota [5] [8]. | Require highly specialized housing and breeding facilities. |
| Gnotobiotic Mice | GF mice colonized with defined microbial communities, allowing reductionist studies. | Community composition can be precisely controlled. |
Translational Applications and Future Directions
Understanding the epigenome-microbiome axis opens transformative possibilities for clinical medicine. Key translational frontiers include:
- Biomarker Discovery: Identifying microbial and epigenetic signatures for early disease detection and monitoring [1] [2]. For instance, DNA methylation within promoters of virulence genes in pathogens like Mycobacterium tuberculosis offers potential diagnostic biomarkers [6].
- Live Biotherapeutic Products (LBPs) and Fecal Microbiota Transplantation (FMT): Precision manipulation of the microbiome to correct dysfunctional epigenetic programming in metabolic, neurological, and inflammatory diseases [1] [9].
- Microbiome-Informed Drug Development: Incorporating microbiome and epigenomic data into clinical trial designs to identify responsive subpopulations and understand mechanisms of drug action and resistance [1].
- Precision Nutrition: Developing dietary interventions tailored to an individual's microbiome to steer epigenetic outcomes toward health promotion [2].
Advancements in high-throughput methylation mapping, artificial intelligence, and single-cell multi-omics are accelerating our ability to model these complex interactions at an unprecedented resolution [1] [9]. However, this progress must be accompanied by rigorous standardization and ethical data governance, guided by frameworks such as the FAIR (Findable, Accessible, Interoperable, Reusable) and CARE (Collective benefit, Authority to control, Responsibility, Ethics) principles [1] [9].
The bidirectional epigenome-microbiome axis represents a fundamental paradigm for understanding how environmental factors, mediated through our microbial inhabitants, shape host physiology and disease susceptibility. The intricate molecular dialogue between microbial metabolites and the host's epigenetic machinery provides a mechanistic basis for the long-lasting effects of the microbiome. As profiling and engineering technologies continue to mature, the potential to harness this axis for precision medicine—developing diagnostics, therapeutics, and nutritional strategies tailored to an individual's unique microbial and epigenetic makeup—becomes increasingly tangible. This field promises to redefine our approach to health and disease by targeting the dynamic interface between our environment and our genome.
Short-chain fatty acids (SCFAs), including acetate, propionate, and butyrate, are major metabolites produced by gut microbiota through the fermentation of dietary fiber. These compounds function as potent epigenetic regulators primarily through the inhibition of histone deacetylases (HDACs) and activation of histone acetyltransferases (HATs), thereby influencing chromatin structure and gene expression. This whitepaper examines the molecular mechanisms by which SCFAs mediate epigenetic modifications and their profound implications for host immune function, metabolic health, and disease susceptibility. Emerging evidence positions SCFAs as crucial mediators in the gut microbiome-epigenome axis, offering promising therapeutic avenues for inflammatory, autoimmune, and metabolic disorders through targeted dietary and microbial interventions.
The human gastrointestinal tract hosts a complex ecosystem of microorganisms, collectively known as the gut microbiota, which encodes a metabolic capacity far exceeding that of the human host [10] [11]. Short-chain fatty acids (SCFAs), primarily acetate (C2), propionate (C3), and butyrate (C4), are produced in substantial quantities (reaching over 100 mM in the colon) through bacterial fermentation of indigestible dietary fibers [12] [13]. These metabolites serve as a critical link between dietary intake, microbial metabolism, and host physiology, forming the foundation of the gut microbiome-epigenome axis.
Beyond their roles in host energy metabolism, SCFAs function as potent signaling molecules that influence gene expression through epigenetic modifications—heritable changes in gene expression that do not alter the DNA sequence itself [10] [11]. The most significant mechanisms include direct inhibition of histone deacetylases (HDACs) and the recent discovery of their role in activating histone acetyltransferases (HATs) [14] [12]. This dual capacity to shape the host epigenetic landscape positions SCFAs as key regulators in maintaining health and modulating disease processes, offering novel insights into how dietary patterns and gut microbiota composition can systemically influence host physiology.
Molecular Mechanisms of SCFA-Mediated Epigenetic Regulation
Histone Deacetylase (HDAC) Inhibition
The classical mechanism underlying SCFA epigenetic function is the inhibition of histone deacetylase (HDAC) enzymes, particularly the zinc-dependent HDAC classes I, IIa, and IIb [14] [15]. HDACs normally remove acetyl groups from lysine residues on histone tails, resulting in a more condensed, transcriptionally repressive chromatin state. By inhibiting HDAC activity, SCFAs lead to the accumulation of hyperacetylated histones, promoting an open chromatin configuration that facilitates gene transcription [14].
Among SCFAs, butyrate demonstrates the most potent HDAC inhibitory activity, with half-maximal inhibitory concentration (IC50) values of approximately 0.09 mM in nuclear extracts from HT-29 human colon carcinoma cells [15]. Propionate exhibits weaker inhibition, while acetate shows minimal HDAC inhibitory effects at physiological concentrations [14] [15]. This HDAC inhibition is not limited to histone substrates but also affects numerous non-histone proteins, including transcription factors and signaling molecules, thereby amplifying the biological impact of SCFAs [14].
Table 1: HDAC Inhibitory Potency of SCFAs
| SCFA | IC50 Value | Experimental System | Reference |
|---|---|---|---|
| Butyrate | 0.09 mM | HT-29 human colon carcinoma cell nuclear extracts | [15] |
| Propionate | Less potent than butyrate | HT-29 human colon carcinoma cell nuclear extracts | [15] |
| Acetate | Minimal inhibition | HT-29 human colon carcinoma cell nuclear extracts | [15] |
Histone Acetyltransferase (HAT) Activation
Recent research has revealed a more complex picture of SCFA epigenetic activity, challenging the historical focus on HDAC inhibition as the primary mechanism. A landmark study demonstrated that propionate and butyrate induce histone hyperacetylation primarily through activation of the acetyltransferase p300, rather than solely through HDAC inhibition [12].
The proposed mechanism involves the intracellular conversion of SCFAs to their corresponding acyl-CoAs (propionyl-CoA and butyryl-CoA), which then act as cofactors to auto-acylate p300's autoinhibitory loop. This autoacylation relieves enzymatic autoinhibition, thereby activating p300 for histone and protein acetylation [12]. This discovery fundamentally shifts our understanding of how SCFAs influence the epigenetic landscape, revealing a previously unknown mechanism of HAT activation that explains global chromatin changes in response to SCFAs.
Novel Histone Acylations
Beyond conventional acetylation, SCFAs contribute to a growing family of short-chain lysine acylations on histones, including propionylation (Kpr) and butyrylation (Kbu) [12] [16]. These modifications occur when SCFAs are converted to their corresponding acyl-CoAs and are incorporated into histones by HATs, which can utilize these cofactors with similar efficiency to acetyl-CoA [16].
Genome-wide mapping studies have revealed that these novel acyl marks (H3K18pr, H3K18bu, H4K12pr, and H4K12bu) are associated with genomic regions distinct from their acetyl counterparts and are enriched at promoters of genes involved in growth, differentiation, and ion transport [16]. This suggests that SCFAs contribute to a complex epigenetic code where different acyl chains may recruit distinct reader proteins or differentially affect chromatin structure, enabling fine-tuned regulation of gene expression programs in response to metabolic inputs.
Figure 1: SCFA-Mediated Epigenetic Mechanisms. SCFAs from dietary fiber fermentation are converted to acyl-CoAs, which drive epigenetic changes through HDAC inhibition, HAT activation, and novel histone acylations, ultimately altering chromatin structure and gene expression.
Quantitative Analysis of SCFA Effects on Epigenetic Marks
The effects of SCFAs on the epigenome are concentration-dependent and exhibit distinct patterns across different compounds. Systematic quantification reveals specific dose-response relationships for various histone modifications.
Table 2: Quantitative Effects of SCFAs on Histone Modifications
| SCFA | Concentration | Histone Modification | Fold Change | Experimental System | Reference |
|---|---|---|---|---|---|
| Propionate | 10 mM | H3K18 propionylation | 1.84× (p=0.0043) | CRC cells | [16] |
| Propionate | 10 mM | H4K12 propionylation | 1.75× (p=0.0017) | CRC cells | [16] |
| Propionate | 0.1 mM | Propionyl-CoA | 0.08→0.35 ng/10^6 cells | CRC cells | [16] |
| Butyrate | 10 mM | Butyryl-CoA | 0.04→0.08 ng/10^6 cells | CRC cells | [16] |
| Butyrate | 10 mM | Acetyl-CoA | 2.25-3.81× decrease | CRC cells | [16] |
Propionate supplementation demonstrates a clear dose-dependent effect on both histone propionylation marks and intracellular propionyl-CoA pools. At 10 mM concentration, propionate significantly increases H3K18pr and H4K12pr marks by approximately 1.8-fold and 1.75-fold, respectively [16]. Similarly, propionyl-CoA levels rise dramatically from 0.08 ng/10^6 cells at 0.1 mM to 0.59 ng/10^6 cells at 10 mM supplementation [16].
Butyrate exhibits a more complex metabolic effect, increasing butyryl-CoA levels while simultaneously decreasing acetyl-CoA pools by 2.25- to 3.81-fold at 1-10 mM concentrations [16]. This reduction in acetyl-CoA may represent an important regulatory mechanism by which butyrate influences the overall epigenetic landscape.
Experimental Approaches for Studying SCFA Epigenetic Regulation
In Vitro Cell Culture Models
Cell-based systems provide controlled environments for investigating SCFA epigenetic mechanisms. Common approaches include:
- Cell lines: HCT116 colon cells and HT-29 human colon carcinoma cells are frequently used due to their colorectal origin and relevance to SCFA physiology [12] [15].
- Treatment conditions: SCFAs (sodium butyrate, sodium propionate) are typically applied at concentrations ranging from 0.1 mM to 10 mM for time periods from 1 hour to 96 hours, depending on the specific readout [17] [18] [12].
- Stimulation protocols: Immune cell differentiation studies often combine SCFAs with polarizing cytokines (e.g., TGF-β, IL-6) and activation signals (CD40 antibody, LPS, CpG) to assess SCFA effects on specific immune cell populations [17] [18].
Analytical Methods for Epigenetic Characterization
Advanced analytical techniques enable comprehensive assessment of SCFA-induced epigenetic changes:
- Histone proteomics: Mass spectrometry-based methods allow simultaneous quantification of >70 histone post-translational modifications, providing a global view of epigenetic changes [12].
- Chromatin immunoprecipitation sequencing (ChIP-seq): Genome-wide mapping of specific histone modifications (H3K18pr, H3K18bu, H4K12pr, H4K12bu) reveals their genomic distribution and association with regulatory elements [16].
- Metabolomic profiling: LC-MS/MS quantification of intracellular acyl-CoA levels (propionyl-CoA, butyryl-CoA, acetyl-CoA) correlates metabolite availability with epigenetic effects [16].
In Vivo and Disease Models
Translation to physiological contexts employs various animal models:
- Germ-free mice: Comparison with conventionally raised mice reveals microbiota-dependent epigenetic patterning [14] [12].
- Disease models: Collagen-induced arthritis (CIA), dextran sodium sulfate (DSS)-induced colitis, and high-fat diet-induced obesity models assess SCFA therapeutic potential [18] [10].
- SCFA administration: Drinking water supplementation (e.g., 100 mM SCFAs) or encapsulated formulations (e.g., BLIPs - butyrate-loaded liposomes) improve bioavailability and reduce cytotoxicity [17] [12].
Figure 2: Experimental Workflow for SCFA Epigenetic Research. Integrated approach combining in vitro models with comprehensive epigenetic analysis and in vivo validation to elucidate SCFA mechanisms and therapeutic potential.
The Scientist's Toolkit: Essential Research Reagents and Methods
Table 3: Key Research Reagents for SCFA Epigenetic Studies
| Reagent/Method | Specifications | Application | Key Findings Enabled |
|---|---|---|---|
| Sodium Butyrate | 0.1-10 mM in cell culture; 100 mM in drinking water | HDAC inhibition; B10 cell induction | Promoted B10 cell generation; inhibited HDAC activity (IC50=0.09 mM) [18] [15] |
| Sodium Propionate | 0.1-10 mM in cell culture | p300 activation; histone propionylation | Induced histone hyperacetylation via p300 activation [12] [16] |
| BLIPs | Butyrate-loaded liposomes | Enhanced SCFA delivery | Reduced cytotoxicity while maintaining immunomodulatory effects on T cells [17] |
| ChIP-seq Antibodies | H3K18pr, H3K18bu, H4K12pr, H4K12bu | Genome-wide mapping of acyl marks | Identified unique genomic locations for SCFA-induced modifications [16] |
| HDAC Activity Assay | Boc-Lys(Ac)-AMC substrate | HDAC inhibition quantification | Established butyrate as most potent SCFA HDAC inhibitor [15] |
Biological Consequences and Functional Outcomes
Immune Cell Regulation
SCFAs directly shape immune responses through epigenetic reprogramming of key immune cell populations:
- Regulatory T Cell (Treg) Enhancement: Butyrate promotes Treg differentiation and function through HDAC inhibition, particularly targeting the Foxp3 locus, thereby strengthening immunological tolerance [17] [10].
- Th17 Suppression: Butyrate suppresses pro-inflammatory Th17 cell differentiation by reducing RORγt expression and IL-17 production through chromatin remodeling [17].
- B10 Cell Generation: Butyrate and pentanoate enhance regulatory B10 cell frequency and function through HDAC inhibitory effects that activate the p38 MAPK signaling pathway [18].
Intestinal Homeostasis and Barrier Function
As the primary site of SCFA production and absorption, the intestinal epithelium exhibits profound responses to SCFA epigenetic regulation:
- Barrier Integrity: Butyrate strengthens intestinal barrier function by enhancing expression of tight junction proteins through HDAC inhibition-mediated effects on gene expression [13].
- Mucosal Immunity: SCFAs promote IgA production and regulate immune cell homing to the gut, maintaining appropriate mucosal responses to commensals and pathogens [10].
- Metabolic Programming: Colonocytes utilize butyrate as their primary energy source, with SCFAs directing metabolic gene expression programs through epigenetic mechanisms [12] [13].
Systemic Metabolic and Inflammatory Regulation
Beyond the gut, SCFAs exert systemic effects through epigenetic mechanisms:
- Obesity and Insulin Sensitivity: SCFAs improve metabolic parameters in obesity models through epigenetic regulation of genes involved in glucose homeostasis and insulin signaling [10].
- Neuroimmune Interactions: Propionate demonstrates neuroprotective effects in Parkinson's disease models through GPR41-dependent mechanisms that may involve epigenetic components [13].
- Cancer Prevention: Butyrate's HDAC inhibitory activity suppresses proliferation and induces apoptosis in colorectal cancer cells, while promoting normal colonocyte health [14] [13].
SCFAs represent a crucial class of microbial metabolites that directly interface with the host epigenome through multiple complementary mechanisms. The traditional view of SCFAs as primarily HDAC inhibitors has been expanded by recent discoveries of their role in activating HATs and contributing to novel histone acylation marks. These epigenetic mechanisms enable SCFAs to fine-tune gene expression programs across tissues, particularly influencing immune cell differentiation, intestinal barrier function, and systemic metabolic regulation.
The therapeutic implications of SCFA epigenetic regulation are substantial, with potential applications in inflammatory diseases, autoimmune conditions, metabolic disorders, and cancer. Future research directions should focus on elucidating the specific reader proteins that recognize SCFA-induced histone modifications, developing tissue-specific SCFA delivery systems, and exploring personalized nutritional approaches based on individual microbiome and epigenome profiles. As our understanding of the gut microbiome-epigenome axis deepens, SCFA-based interventions represent a promising frontier for precision medicine approaches that harness dietary components and microbial metabolites for disease prevention and treatment.
The gut microbiome serves as a critical interface between host nutrition and epigenetic regulation. This review elucidates the mechanisms by which gastrointestinal microbiota synthesize, utilize, and modulate the availability of key one-carbon (1-C) metabolism substrates—folate and vitamin B12—thereby influencing the host's epigenetic landscape. We explore how microbial contributions to methyl donor pools directly impact DNA methylation, histone modification, and non-coding RNA expression, with significant implications for host health and disease states. The integration of quantitative data on microbial metabolic capabilities, alongside standardized experimental protocols and essential research tools, provides a comprehensive resource for investigators exploring the microbiota-epigenome axis.
One-carbon (1-C) metabolism comprises an interconnected network of biochemical pathways—the folate cycle, methionine cycle, and transsulfuration pathway—that operate across cellular compartments to generate 1-C units essential for molecular biosynthesis, redox defense, and epigenetic regulation [19]. A crucial function of this system is the production of S-adenosylmethionine (SAM), the universal methyl donor required for DNA and histone methylation processes that orchestrate gene expression without altering the DNA sequence itself [19] [20]. The proper functioning of 1-C metabolism is fundamentally dependent on specific dietary nutrients and metabolites, including folate, vitamin B12, choline, betaine, and homocysteine [19].
Emerging evidence positions the gut microbiome as a central modulator of 1-C metabolism. Resident gastrointestinal bacteria directly contribute to host methyl donor availability through de novo synthesis of folate and vitamin B12, consumption of these compounds for their own metabolic needs, and production of metabolites that influence host metabolic pathways [21] [22]. This microbial influence creates a dynamic pathway through which environmental factors, particularly diet, can shape the host epigenome. Understanding these complex interactions is paramount for elucidating the pathophysiology of various diseases and developing novel therapeutic strategies targeting the microbiota-epigenome axis [22].
Microbial Contribution to Folate and Vitamin B12 Availability
Folate Synthesis and Utilization by Gut Microbiota
Folate (vitamin B9) is a essential water-soluble vitamin that functions as a critical cofactor in 1-C transfer reactions. While humans cannot synthesize folate endogenously and must obtain it from dietary sources or microbiota, numerous gut bacteria possess the enzymatic machinery for de novo folate biosynthesis [19] [21].
Key Aspects of Microbial Folate Metabolism:
- Synthesis and Bioavailability: Certain gut microbial species, including lactobacilli and bifidobacteria, can synthesize folates de novo. However, the bioavailability of microbially produced folates for the host depends on their form and location (luminal versus mucosal) [21].
- Absorption Dynamics: Dietary folates are hydrolyzed to their monoglutamated forms in the small intestine, a process facilitated by gut microbiota through enzymes like γ-glutamyl hydrolase (GGH) and glutamate carboxypeptidase II (GCPII), enabling absorption [19].
- Regulation of Host Status: The gut microbiome composition can influence host folate status by modulating the balance between synthesis and consumption of folate within the intestinal lumen, potentially affecting systemic folate levels and, consequently, methyl donor availability for epigenetic processes [21].
Vitamin B12 Dynamics in the Gut Microbiome
Vitamin B12 (cobalamin) is a complex organometallic compound synthesized exclusively by certain bacteria and archaea. It serves as an essential cofactor for two human enzymes: methionine synthase and L-methylmalonyl-CoA mutase [21] [23]. Its metabolism within the gastrointestinal tract represents a complex interplay between host and microbes.
Key Aspects of Microbial Vitamin B12 Metabolism:
- Synthesis and Competition: While some gut microbes produce vitamin B12, others are consumers. This can lead to competition for the vitamin between the host and specific bacterial species, potentially influencing host B12 status [21].
- Analog Production: Vitamin B12 not absorbed in the ileum reaches the colon, where gut bacteria convert approximately 80% into analogs (cobamides) with limited or no known vitamin activity in humans, altering the functional availability of B12 [21].
- Gene Regulation in Bacteria: Vitamin B12 is required for over a dozen enzymes in bacteria and regulates bacterial genes through B12-responsive riboswitches, making its availability a determinant of microbial community structure and function [21].
Table 1: Bacterial Genera Involved in Folate and Vitamin B12 Metabolism
| Bacterial Genus/Group | Role in 1-C Metabolism | Functional Significance |
|---|---|---|
| Lactobacillus | Folate synthesis | Contributes to host folate availability; potential probiotic candidate [21] |
| Bifidobacterium | Folate synthesis | Contributes to host folate availability; potential probiotic candidate [21] |
| Methanobrevibacter | Vitamin B12 synthesis (Archaea) | May compete with host for dietary B12 or provide it in certain contexts [22] |
| Bacteroidetes | Mixed (B12 consumers/producers) | High demand for B12; major competitors for available B12 [21] |
| Firmicutes | Mixed (B12 consumers/producers) | Includes both producers and consumers; affects net B12 balance [21] [22] |
| Akkermansia | Mucin degradation | Indirectly affects 1-C metabolism by influencing gut barrier integrity and inflammation [22] |
| Faecalibacterium | Butyrate production | Indirectly affects 1-C metabolism via anti-inflammatory effects and gut health [22] |
Impact on Host Epigenetic Mechanisms
The microbial modulation of folate and vitamin B12 availability has direct consequences for host epigenetic regulation, primarily through the provision of methyl groups for SAM-dependent methylation reactions.
- DNA Methylation: SAM donates methyl groups to DNA methyltransferases (DNMTs) for cytosine methylation in CpG islands. Deficiencies in folate or B12 can lead to hyperhomocysteinemia and reduced SAM production, potentially causing global DNA hypomethylation and altered gene-specific methylation patterns [19] [20]. This is critically important during periods of rapid cellular division, such as embryonic development [19].
- Histone Modification: SAM is the methyl donor for histone methyltransferases (HMTs). Changes in methyl donor availability can modify histone methylation marks (e.g., H3K4me3 for activation, H3K9me3 for repression), thereby altering chromatin structure and gene accessibility [19] [22].
- Intergenerational and Developmental Programming: The periconceptional period is particularly sensitive to methyl donor supply. Maternal nutrition and gut microbiome composition can influence the epigenetic reprogramming of the embryo, with potential lifelong consequences for offspring health, as posited by the "Developmental Origins of Health and Disease" hypothesis [19].
The diagram below illustrates the core pathways of host 1-C metabolism and the specific points of microbial influence.
Diagram 1: Microbial Influence on Host 1-C Metabolism and Epigenetics. The gut microbiome contributes directly by synthesizing folate and B12, and indirectly by producing B12 analogs that may compete with host uptake. MTHFR: Methylene tetrahydrofolate reductase.
Experimental Methodologies for Investigating Microbial-Epigenetic Interactions
Studying the specific contributions of the gut microbiome to host methyl donor availability and epigenetic marks requires integrated, multi-omics approaches.
Characterizing Microbial Community Structure and Functional Potential
- 16S rRNA Gene Sequencing: This standard method assesses microbial community composition (β-diversity) and diversity within a sample (α-diversity). It can identify shifts in microbial populations associated with altered folate or B12 status [21] [22].
- Protocol: Amplify the V3-V4 hypervariable region of the 16S rRNA gene using primers 341F (5'-CCTACGGGNGGCWGCAG-3') and 805R (5'-GACTACHVGGGTATCTAATCC-3'). Sequence on an Illumina MiSeq platform. Process data using QIIME2 or Mothur to assign operational taxonomic units (OTUs) and perform diversity analyses [21] [22].
- Shotgun Metagenomic Sequencing: This provides higher resolution by sequencing all microbial DNA in a sample, allowing for direct assessment of the genetic potential for folate and B12 synthesis (e.g., presence of folP, cob genes) and utilization [21].
- Protocol: Extract total DNA from fecal samples. Prepare libraries without PCR amplification to reduce bias. Sequence on an Illumina NovaSeq platform. Analyze using HUMAnN2 or MetaPhlAn2 for taxonomic profiling and pathway analysis (e.g., MetaCyc pathways for folate and B12 metabolism) [21].
- Metatranscriptomics: RNA-based sequencing reveals the actively expressed genes within the microbiome, distinguishing between functional potential and actual activity in folate and B12 pathways [21].
Assessing Host Epigenetic Modifications
- Genome-Wide DNA Methylation Analysis (Whole-Genome Bisulfite Sequencing - WGBS): This is the gold standard for quantifying DNA methylation at single-base resolution across the entire genome.
- Protocol: Extract genomic DNA from host tissues (e.g., blood, intestinal mucosa). Treat DNA with sodium bisulfite, which converts unmethylated cytosines to uracils (read as thymines), while methylated cytosines remain unchanged. Sequence the converted DNA and align to a reference genome to determine methylation status at each CpG site. Differential methylation analysis can be performed using tools like MethylKit or DSS [22].
- Histone Modification Profiling (Chromatin Immunoprecipitation Sequencing - ChIP-seq): This identifies genomic regions bound by specific histone modifications.
- Protocol: Cross-link proteins to DNA in cells or tissues. Sonicate chromatin to fragment. Immunoprecipitate the cross-linked DNA-protein complexes using antibodies specific to a histone mark (e.g., H3K4me3, H3K27me3). Reverse cross-links, purify DNA, and prepare libraries for sequencing. Analyze enriched regions to understand how methyl donor availability influences the histone landscape [22].
The following workflow diagram outlines the process of an integrated analysis to connect microbiome data with host epigenetics.
Diagram 2: Integrated Workflow for Microbial-Epigenetic Studies. This pipeline connects microbiome characterization with host epigenetic analyses to establish functional relationships.
Intervention Studies: From Correlation to Causation
- Gnotobiotic Mouse Models: Germ-free mice colonized with defined microbial communities (including communities that differ in their folate or B12 synthesis capabilities) allow for direct testing of microbial functions on host methyl donor metabolism and epigenetics [21] [22].
- Fecal Microbiota Transplantation (FMT): Transplanting fecal microbiota from human donors (e.g., with defined nutritional status or disease) into germ-free or antibiotic-treated mice can demonstrate causal effects of a microbial community on host phenotype, including epigenetic endpoints [22].
- Targeted Nutritional Interventions: Supplementation with rumen-protected methyl donors (e.g., folate, methionine, choline, betaine) or vitamin B12 in controlled studies, while monitoring changes in the gut microbiome, host 1-C metabolites (e.g., plasma homocysteine, SAM), and tissue-specific epigenetic marks [19] [20].
The Scientist's Toolkit: Essential Reagents and Methodologies
Table 2: Key Research Reagents and Resources for Investigating Microbial-Epigenetic Interactions
| Reagent / Resource | Function / Application | Example Use Case |
|---|---|---|
| Rumen-Protected Methyl Donors | Oral delivery of methyl donors (e.g., folate, choline, methionine) to the lower GI tract with minimal upper GI absorption, allowing direct modulation of the gut microbiome [20]. | Studying the direct effect of methyl donors on microbial composition and host epithelial epigenetics in animal models. |
| Vitamin B12 Assay Kits (ELISA/EIA) | Quantification of total vitamin B12 (and analogs) in serum, plasma, or fecal samples. | Correlating systemic or local B12 status with microbial metabolic potential and host DNA methylation patterns. |
| Folate Microbiological Assay | Microbiological quantification of folate using Lactobacillus casei, which responds to biologically active folate forms. | Measuring functional folate levels in biological samples to assess microbial contribution. |
| S-Adenosylmethionine (SAM) & S-Adenosylhomocysteine (SAH) ELISA Kits | Precise measurement of SAM and SAH levels in tissues or plasma. The SAM:SAH ratio is a key indicator of cellular methylation capacity. | Linking microbial-modulated methyl donor availability to the host's functional methylation potential. |
| Methylated DNA Immunoprecipitation (MeDIP) Kits | Antibody-based enrichment of methylated DNA sequences for downstream analysis (e.g., qPCR, sequencing). | Profiling DNA methylation in specific genomic regions of interest (e.g., imprinting control regions) in response to microbial shifts. |
| B12-Depleted Animal Diets | Defined diets for creating B12 deficiency in animal models to study the subsequent effects on the gut microbiome and host epigenome. | Isolating the role of B12 in maintaining microbial communities and epigenetic homeostasis. |
| BioRender | Online tool with a vast library of scientifically accurate icons and templates for creating publication-quality figures and diagrams [24]. | Visualizing complex metabolic pathways, experimental designs, and microbial-host interactions. |
The gut microbiome is an integral and modifiable component of the host's one-carbon metabolism network, significantly influencing the availability of folate and vitamin B12 for epigenetic programming. The experimental frameworks and tools detailed herein provide a roadmap for deciphering the precise mechanisms underlying this interaction. Future research leveraging multi-omic integration and targeted interventions will be crucial for translating this knowledge into novel microbiome-based diagnostics and therapeutics for a range of diseases linked to epigenetic dysregulation, from metabolic disorders to psychiatric illnesses.
The gut microbiome functions as a dynamic endocrine organ that profoundly influences host physiology. A key mechanism of this influence is through the modulation of the host epigenome—the collection of chemical modifications to DNA and histones that regulate gene expression without altering the underlying DNA sequence [1]. Within this framework, polyamine biosynthesis and extracellular vesicle (EV) communication have emerged as two pivotal, interconnected pathways. These pathways facilitate a continuous dialogue between gut microbiota and host cells, enabling microbial influence over host transcriptional programs and cellular functions. This whitepaper provides an in-depth technical analysis of these pathways, detailing their mechanisms, experimental investigation, and implications for drug development.
Polyamine Biosynthesis in the Gut Microbiome
Core Pathways and Metabolites
Polyamines, primarily putrescine (PUT) and spermidine (SPD), are small, polycationic organic compounds ubiquitous in all living cells. They are crucial for cell proliferation, differentiation, and gene expression due to their ability to bind negatively charged macromolecules like DNA and RNA [25] [26]. In the gut, the lumen of the upper small intestine primarily obtains polyamines from the diet, whereas the colon relies heavily on microbial metabolism as a source [26].
Intracellular polyamine levels are stringently regulated via biosynthesis, catabolism, and transport. The core biosynthetic pathway in mammals and microbes originates from arginine. As shown in the pathway diagram, arginine is converted to ornithine, which ornithine decarboxylase (ODC) then decarboxylates to form putrescine. Spermidine and spermine are subsequently synthesized through the sequential addition of aminopropyl groups from decarboxylated S-adenosylmethionine (dcSAM) [25] [26].
However, gut microbiota exhibit unique and complex polyamine metabolic pathways that can span multiple bacterial species. Key bacterial pathways include:
- The Ornithine Decarboxylase Pathway: Prevalent in bacteria like Escherichia coli, where constitutive (speC) and inducible (speF) ornithine decarboxylases convert ornithine to putrescine [26].
- The Arginine Decarboxylase (ADC) Pathway: Arginine is first decarboxylated to agmatine, which is then hydrolyzed to N-carbamoylputrescine and finally to putrescine. This pathway is present in species like Campylobacter jejuni and Bacteroides thetaiotaomicron [26].
- The L-Aspartate-β-Semialdehyde (ASA) Pathway: A distinct pathway in certain bacteria like Campylobacter jejuni and many Bacteroides species, where putrescine is converted to carboxyspermidine and then to spermidine [26].
A recent stable isotope-resolved metabolomics (SIRM) study using [U-13C]-inulin revealed distinct 13C enrichment profiles for SPD and PUT in the human gut microbiome, indicating that the arginine-agmatine-SPD pathway contributes to SPD biosynthesis alongside the canonical spermidine synthase pathway [27].
Quantitative Polyamine Levels in Health and Disease
Polyamine levels are tightly regulated, and their dysregulation is associated with various disease states. The table below summarizes key quantitative findings from recent research.
Table 1: Quantitative Data on Polyamine Levels in Health and Disease
| Metric | Healthy State | Disease State (Inflammatory Bowel Disease) | Context and Notes |
|---|---|---|---|
| Fecal Putrescine (PUT) | ~791.2 μM [27] | Significantly higher in IBD patients [27] | Level in healthy adults; derived from gut microbiota [27] [26] |
| Fecal Spermidine (SPD) | ~56.8 μM [27] | Significantly higher in IBD patients [27] | Level in healthy adults; derived from gut microbiota [27] [26] |
| Plasma PUT | ~5.3 μM [27] | Information Not Specified | Level in healthy individuals [27] |
| Plasma SPD | ~0.6 μM [27] | Information Not Specified | Level in healthy individuals [27] |
| Key Bacterial Contributor | Bacteroides spp. [27] | Bacteroides spp. [27] | Identified as key contributors to polyamine biosynthesis via SIRM and in silico analysis [27] |
Connection to Host Epigenetic Regulation
Polyamines exert a direct influence on the host epigenome through several mechanisms:
- Nucleosome Condensation: By binding to DNA, polyamines can promote the condensation of nucleosomes, a process intrinsically linked to histone methylation and acetylation, thereby influencing chromatin accessibility and gene transcription [28].
- Histone Modification: Spermidine induces the expression of global regulators like LaeA and the α-NAC transcriptional coactivator in fungi, a mechanism connected to epigenetic modification of histones that controls the switch to secondary metabolite production [28].
- Methylation Cycle Interconnection: Polyamine biosynthesis is metabolically intertwined with the methionine cycle, which produces S-adenosylmethionine (SAM), the primary methyl donor for DNA and histone methyltransferases. The consumption of SAM in polyamine synthesis can directly influence the cellular capacity for epigenetic methylation [25].
Extracellular Vesicle-Mediated Communication
Biogenesis and Function of Bacterial Extracellular Vesicles
Bacterial extracellular vesicles (BEVs) are nanoscale lipid bilayer vesicles (typically 40-200 nm) secreted by both Gram-negative and Gram-positive gut bacteria [29] [30]. They are generated through the double invagination of the plasma membrane and the formation of intracellular multivesicular bodies (MVBs), which release intraluminal vesicles (exosomes) upon fusion with the plasma membrane [31].
BEVs carry a diverse cargo of proteins, nucleic acids (DNA, RNA), lipids, and metabolites from their parent cell [32]. Crucially, machine learning analysis of 16S rRNA data has revealed that the taxonomic composition of gut microbiota-derived EVs forms a distinct entity from the overall gut microbiota. This highlights that conventional microbiota composition analyses are insufficient to fully understand gut microbiota-host communication, and EVs must be reported separately [30].
BEVs as Vectors for Epigenetic Reprogramming
BEVs facilitate intercellular communication by transferring their bioactive cargo to recipient host cells, leading to functional changes and epigenetic reprogramming. The diagram below illustrates how BEVs modify the epigenome of a recipient host cell.
The following Dot language code defines the elements and relationships in the BEV-mediated epigenetic reprogramming process:
The specific epigenetic mechanisms are:
- Modulation of DNA Methylation: BEVs derived from leukemia cells have been shown to increase global DNA methylation in recipient cells. This occurs through the transfer of RNA that upregulates DNA methyltransferases (DNMT3a, DNMT3b), leading to hypermethylation and silencing of tumor-suppressor genes like P53 and RIZ1 [32].
- Delivery of Regulatory Non-Coding RNAs: BEVs are enriched with miRNAs and other non-coding RNAs. Upon delivery, these miRNAs can directly bind to and regulate host mRNA targets, representing a powerful form of post-transcriptional epigenetic regulation [31] [33].
- Transfer of Histone-Modifying Enzymes: Bioinformatic analyses suggest that BEV cargoes are enriched with mRNAs and proteins involved in histone acetylation, deacetylation, and ubiquitination, indicating a potential role in directly altering the histone landscape of host cells [32].
Experimental Protocols and Methodologies
Tracking Polyamine Biosynthesis with Stable Isotope-Resolved Metabolomics (SIRM)
SIRM is a powerful approach for dynamically tracking the incorporation of labeled atoms into metabolites, enabling the elucidation of active metabolic pathways.
Table 2: Research Reagent Solutions for Microbiome Polyamine SIRM
| Reagent / Material | Function / Application | Example Source / Specification |
|---|---|---|
| [U-13C]-Inulin | Stable isotope tracer to track microbial metabolic pathways using an effective substrate for the gut microbiome. | IsoLife bv (≥97 atom % 13C) [27] |
| Fresh Human/Mouse Feces | Source of viable gut microbial cells for ex vivo incubations. | Donors with no recent antibiotics/probiotics [27] |
| Gifu Anaerobic Medium (GAM) | Culture medium for supporting the growth and activity of anaerobic gut microbes during incubation. | Hopebio Co., Ltd [27] |
| Anaerobic Glove Bags/Chambers | Provides an oxygen-free environment for sample processing and incubation to maintain microbiome vitality. | NPS Corporation; with anaerobic gas production bags [27] |
| N-(9-fluorenylmethoxycarbonyloxy)succinimide (Fmoc-OSu) | Derivatization reagent for polyamines to enable their detection and analysis via LC-MS. | Sigma-Aldrich (purity ≥ 98.0%) [27] |
| Liquid Chromatography-High Resolution Mass Spectrometry (LC-HRMS) | Analytical platform for separating and detecting 13C-labeled polyamines and related metabolites with high precision. | N/A [27] |
Detailed SIRM Protocol:
- Fecal Microbiome Separation: Fresh fecal samples from healthy human donors or mice are collected and immediately transferred to an anaerobic glove bag. Samples are suspended in culture medium (e.g., GAM) and subjected to low-speed centrifugation (35 × g, 10 min) to remove large, undigested particles. The supernatant is then centrifuged at 865 × g for 10 min to pellet the microbial cells, which are washed and resuspended in fresh medium [27].
- Anaerobic Incubation with Tracer: The pelleted microbial cells are incubated anaerobically at 37°C for 24 hours in medium containing 2 g/L of [U-13C]-inulin. Control groups are incubated with unlabeled (12C) inulin [27].
- Sample Quenching and Metabolite Extraction: After incubation, samples are centrifuged to separate the culture medium from the microbial cells. The cells are immediately quenched with acetonitrile containing 0.2% formic acid. The culture medium is lyophilized, and the dried powder is reconstituted in acetonitrile with 0.2% formic acid [27].
- Derivatization of Polyamines: A 50 μL aliquot of the sample is mixed with 50 μL of carbonate buffer (pH 10.2) and 50 μL of 5 mM Fmoc-OSu solution in acetonitrile. The mixture is shaken at room temperature for 15 min. The reaction is quenched with formic acid, and the derivatized polyamines are extracted into ethyl acetate [27].
- LC-HRMS Analysis: The extracted samples are analyzed using LC-HRMS. The derivatization facilitates the sensitive detection and quantification of polyamines. The high mass resolution allows for the precise measurement of 13C enrichment in PUT, SPD, and related metabolites, revealing the active biosynthetic pathways [27].
Isolating and Analyzing Gut Microbiota-Derived EVs
The following workflow outlines the key steps for isolating and analyzing BEVs from fecal samples, which is critical for studying their epigenetic effects.
The following Dot language code defines the steps for isolating and analyzing BEVs:
Key Methodological Steps:
- EV Isolation: Differential ultracentrifugation is a standard method. Sequential centrifugation steps at increasing speeds (e.g., 2,000 × g to remove bacteria and debris, followed by 100,000 × g to pellet EVs) are used to isolate EVs from fecal supernatants or bacterial culture media [30].
- EV Characterization: Isolated EVs are characterized for size, concentration, and morphology using techniques like Nanoparticle Tracking Analysis (NTA) and transmission electron microscopy (TEM) [30].
- Taxonomic and Functional Profiling: 16S rRNA gene sequencing of the EV-associated DNA is performed and analyzed with bioinformatic tools and machine learning models to determine the taxonomic origin of the EVs and confirm their distinct nature from the whole microbiota [30]. The protein and RNA cargo is analyzed via proteomics and RNA sequencing to identify potential epigenetic effectors [32] [31].
Implications for Drug Development
The intricate pathways of polyamine metabolism and EV communication present novel targets for therapeutic intervention.
- Targeting Polyamine Metabolism in Leukemia: Functional alterations in polyamine metabolism are observed in acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL). Promising therapeutic targets include MAT2A and PRMT5, enzymes at the crossroads of polyamine metabolism and epigenetic regulation. Selective inhibitors of these enzymes are under investigation [25].
- Polyamine Modulation in IBD: The finding that Bacteroides spp. drive upregulated polyamine levels in IBD opens avenues for precision therapies. Modulating the gut microbiome or specific bacterial pathways to normalize polyamine levels could be a strategy to manage intestinal inflammation [27].
- BEVs as Diagnostic Biomarkers and Drug Delivery Vehicles: The distinct molecular cargo of BEVs makes them excellent non-invasive biomarkers for diseases like cancer and IBD [32] [30]. Furthermore, their natural ability to cross biological barriers, including the blood-brain barrier, and their biocompatibility make them promising engineered platforms for targeted drug delivery, including for epigenetic therapies [29] [31] [33].
Polyamine biosynthesis and extracellular vesicle communication represent two fundamental, synergistic pathways through which the gut microbiome influences the host epigenome. Technical advances in SIRM and EV isolation/multi-omics are enabling researchers to deconstruct these complex interactions with unprecedented detail. For drug development professionals, a deep understanding of these pathways is no longer a niche interest but a critical component of developing next-generation therapeutics targeting epigenetic dysregulation in oncology, gastroenterology, and beyond.
The traditional view of the host epigenome as a system solely influenced by host genetics and environmental factors is undergoing a paradigm shift. Emerging evidence compellingly demonstrates that the gut microbiome serves as a crucial interface between the external environment and the host's internal genomic regulation, giving rise to the concept of the holoepigenome. This framework conceptualizes the host and its microbiome as an integrated, co-adaptive unit where microbial communities actively shape the host's epigenetic landscape, influencing physiology, disease susceptibility, and evolutionary potential [34] [35]. Within the broader context of gut microbiome research, understanding the holoepigenome is paramount for deciphering the mechanisms through which gut microbes exert their profound effects on host health and disease. This whitepaper delves into the molecular mechanisms of microbiome-epigenome crosstalk, outlines key experimental methodologies, and explores the therapeutic implications of targeting the holoepigenome, providing a technical guide for researchers and drug development professionals.
Core Mechanisms of Microbiome-Epigenome Crosstalk
The communication between the gut microbiota and the host epigenome is primarily mediated by a diverse array of microbially derived metabolites and components. These molecules influence all major epigenetic mechanisms, including DNA methylation, histone modifications, and non-coding RNA expression [36] [4] [37].
Table 1: Key Microbiota-Derived Metabolites and Their Epigenetic Effects
| Metabolite/Component | Primary Microbial Sources | Epigenetic Target | Molecular Outcome & Functional Impact |
|---|---|---|---|
| Short-Chain Fatty Acids (SCFAs) | Faecalibacterium, Roseburia, Eubacterium (Firmicutes) [22] [36] | Histone Deacetylases (HDACs) [36] [38] | HDAC inhibition → Increased histone acetylation → Altered gene expression in immunity & metabolism [36] [38] |
| Folate | Bifidobacterium, Lactobacillus [36] | DNA Methyltransferases (DNMTs) [36] | Donor for S-adenosylmethionine (SAM) → Altered DNA methylation patterns → shifts in host cell transcriptome [36] |
| Lipopolysaccharide (LPS) | Gram-negative bacteria (e.g., Escherichia, Bacteroides) [36] | DNA Methylation | Altered methylation of immune-related genes (e.g., TLR4) → modulation of inflammatory responses [36] |
| Genotoxins (e.g., Colibactin) | pks+ E. coli [39] | DNA Integrity | DNA double-strand breaks & crosslinks → replication stress → genomic instability in colon epithelial cells [39] |
The holoepigenome is not a static entity but a dynamic system responsive to dietary and environmental perturbations. For instance, a high-fat diet can reduce populations of butyrate-producing bacteria, thereby diminishing the pool of a critical endogenous HDAC inhibitor and fundamentally altering the host's epigenetic state [36]. This metabolic signaling represents a primary pathway through which the microbiome integrates environmental cues to fine-tune host gene expression.
Visualizing the Signaling Pathways and Workflows
The complex interactions within the holoepigenome can be visualized through key signaling pathways and standardized research workflows.
SCFA-Mediated Epigenetic Regulation
The following diagram illustrates the primary pathway through which microbiota-derived SCFAs, particularly butyrate, influence host gene expression by modulating histone acetylation.
Experimental Workflow for Holoepigenome Analysis
A typical integrated workflow for investigating the holoepigenome involves multi-omics data collection and correlation analysis, as outlined below.
The Scientist's Toolkit: Key Research Reagents & Models
Advancing holoepigenome research requires a specific toolkit of experimental models, reagents, and analytical techniques.
Table 2: Essential Research Reagents and Models for Holoepigenome Studies
| Category | Item / Model | Key Function & Application |
|---|---|---|
| In Vivo Models | Germ-Free (Gnotobiotic) Mice | Provides a microbiome-free baseline to assess causal effects of defined microbial communities on the host epigenome [36] [38]. |
| Genetically Engineered Mouse Models (e.g., Apcmin/+) | Used in conjunction with microbial interventions to study microbiome-epigenome interactions in disease contexts like colorectal cancer [39]. | |
| Experimental Interventions | Fecal Microbiota Transplantation (FMT) | Transfers entire microbial communities from donor to recipient to investigate their causal role in reshaping the host epigenome and phenotype [22]. |
| Antibiotic Cocktails | Depletes the gut microbiota to study the consequences of its absence on host epigenetic marks and gene expression [38]. | |
| Defined Microbial Consortia | Used to colonize gnotobiotic mice with a simplified, known community to dissect specific host-microbe interactions. | |
| Analytical Reagents & Kits | HDAC Inhibitors (e.g., Sodium Butyrate) | Pharmacological tools used in vitro to mimic the epigenetic effects of SCFAs and study downstream transcriptional effects [36]. |
| DNA Methylation Kits (e.g., for WGBS) | Reagents for genome-wide analysis of DNA methylation patterns (5mC) in host tissues following microbial manipulation [39] [40]. | |
| Chromatin Immunoprecipitation (ChIP) Kits | Kits for mapping histone modifications (e.g., H3K9ac, H3K27me3) in host cells in response to microbial signals [38]. |
Detailed Experimental Protocols
To ensure reproducibility and rigor in holoepigenome research, the following core protocols are essential.
Protocol for Fecal Microbiota Transplantation (FMT) in Murine Models
Objective: To directly test the causal impact of a donor microbiome on the recipient host's epigenome. Materials: Donor mice (e.g., disease model or specific genotype), recipient mice (germ-free or antibiotic-treated), anaerobic workstation, sterile PBS, homogenizer, gavage needles. Procedure:
- Donor Inoculum Preparation: Harvest fresh fecal pellets from donor mice. Weigh and resuspend in anaerobic, sterile PBS (e.g., 100 mg/mL). Homogenize thoroughly and filter through a sterile mesh to remove large particulates. Process and use the inoculum rapidly under anaerobic conditions to preserve microbial viability [22].
- Recipient Preparation: Recipient mice should be either germ-free or pre-treated with a broad-spectrum antibiotic cocktail in their drinking water for 2-3 weeks to deplete the endogenous microbiota.
- Transplantation: Administer the prepared donor inoculum (e.g., 200 µL) to each recipient mouse via oral gavage. Control groups should receive a vehicle (PBS) only.
- Post-FMT Monitoring: House recipients in appropriate caging and monitor for phenotypic changes. Collect fecal samples over time to verify engraftment of the donor microbiota via 16S rRNA sequencing.
- Endpoint Analysis: Euthanize mice and collect target tissues (e.g., colon, liver, brain). Analyze epigenetic marks (e.g., via WGBS or ChIP-seq) and correlate with microbial engraftment data [22].
Protocol for Assessing Microbiome-Induced DNA Damage
Objective: To evaluate the genotoxic potential of specific bacteria or communities on host epithelial cells. Materials: pks+ E. coli (test), pks- E. coli (control), human colonic epithelial cell line (e.g., HCT116), cell culture facilities, gamma-H2AX antibody for immunofluorescence. Procedure:
- Cell Culture & Infection: Culture colonic epithelial cells in standard conditions. At ~70% confluence, infect cells with either pks+ E. coli or an isogenic pks- control strain at a defined multiplicity of infection (MOI). Co-culture for 4-6 hours.
- DNA Damage Staining: Fix cells and permeabilize. Stain with a primary antibody against phospho-histone H2AX (gamma-H2AX), a sensitive marker for DNA double-strand breaks, followed by a fluorescently labeled secondary antibody. Counterstain nuclei with DAPI [39].
- Imaging & Quantification: Image cells using a fluorescence microscope. Quantify the number of gamma-H2AX foci per nucleus. A statistically significant increase in foci in pks+ E. coli-infected cells compared to controls indicates microbiota-induced DNA damage, a precursor to potentially stable epigenetic and genetic changes [39].
Implications for Drug Development and Therapeutic Innovation
The holoepigenome concept opens novel avenues for therapeutic intervention. Strategies can target the microbiome to indirectly steer the host epigenome toward a healthier state or target the host's epigenetic machinery that responds to microbial signals.
- Live Biotherapeutic Products (LBPs): Engineered bacterial strains, such as those producing high levels of SCFAs like butyrate, can be developed to deliver targeted epigenetic-modifying signals to the gut [22]. For example, increasing Faecalibacterium abundance could enhance HDAC inhibition, promoting an anti-inflammatory state.
- Precision Prebiotics and Diets: Nutritional interventions can be designed to selectively nourish beneficial taxa that produce favorable epigenetic metabolites. This approach leverages diet to manage the holoepigenome for chronic disease prevention and management [36].
- Epigenetic Drugs Informed by Microbiome: The efficacy of existing epigenetic drugs, such as HDAC inhibitors used in oncology, may be influenced by the patient's microbiome. Understanding this interaction could lead to microbiome-based biomarkers for drug response and the development of combination therapies that modulate both the microbiome and the epigenome [38] [39].
The evidence is compelling: the host and its microbiome function as a cohesive, co-adaptive unit—the holoepigenome—that is fundamental to understanding mammalian biology and disease etiology. The bidirectional communication, mediated largely by microbial metabolites, seamlessly integrates environmental cues with host gene regulation. Future research must focus on longitudinal human studies to track holoepigenome dynamics over time and in response to interventions, and on developing more sophisticated multi-omics integration tools to move from correlation to causation. For drug developers, the message is clear: the microbiome is not merely a passive passenger but an active participant in shaping the host's epigenetic landscape. Embracing this complexity is no longer optional but essential for pioneering the next generation of targeted, effective therapeutics.
From Bench to Bedside: Advanced Methodologies and Therapeutic Translation
The human gut microbiome, a complex ecosystem of bacteria, viruses, and fungi, profoundly influences host physiology through dynamic crosstalk with human cells. A key mechanism of this interaction is epigenetic regulation, where microbial metabolites and signals modify host gene expression without changing the underlying DNA sequence [1] [2]. These modifications include DNA methylation, histone modifications, and RNA methylation, which collectively regulate phenotypic plasticity and disease susceptibility [1] [41] [2]. Cutting-edge genomic tools are now unveiling the precise mechanisms of this interaction, revealing that microbial metabolites such as short-chain fatty acids (SCFAs), polyamines, and nutrients from bacterial one-carbon metabolism serve as substrates and signals for host epigenetic machinery [1]. This review details the single-cell multi-omics and high-throughput methylation mapping technologies that are revolutionizing our understanding of the gut microbiome's impact on the host epigenome, providing a technical guide for researchers and drug development professionals.
Single-Cell Multi-Omic Technologies for Host-Microbe Analysis
scEpi2-seq: Simultaneous Profiling of Histone Modifications and DNA Methylation
Single-cell Epi2-seq (scEpi2-seq) is a groundbreaking method that enables the joint readout of histone modifications and DNA methylation in single cells, overcoming previous limitations of studying these marks in isolation [42].
- Core Principle: The technique leverages a pA–MNase fusion protein tethered to specific histone modifications (e.g., H3K9me3, H3K27me3, H3K36me3) via antibodies. After single-cell sorting and MNase digestion, the released fragments are processed for library preparation. A critical innovation is the use of TET-assisted pyridine borane sequencing (TAPS) for DNA methylation detection, which converts methylated cytosine (5mC) to uracil without damaging the adaptor sequences, unlike traditional bisulfite sequencing [42].
- Workflow Output: From each sequencing read, researchers can extract three key pieces of information:
- Histone mark location from mapped genomic positions.
- DNA methylation status from C-to-T base conversions.
- Nucleosome spacing from distances between sequencing read start sites [42].
- Performance Metrics: Applied to K562 cells, scEpi2-seq successfully profiled over 50,000 CpGs per single cell with high specificity (Fraction of Reads in Peaks/FRiP ranging from 0.72 to 0.88) and a C-to-T conversion rate of ~95% [42]. This allows for the direct observation of epigenetic interactions, such as the finding that regions marked by repressive histone marks H3K27me3 and H3K9me3 exhibit much lower DNA methylation levels (~8-10%) compared to regions marked by the active transcription-associated mark H3K36me3 (~50%) [42].
Table 1: Key Performance Metrics of scEpi2-seq in Model Cell Lines
| Parameter | K562 Cells | RPE-1 hTERT Cells |
|---|---|---|
| Cells Profiled | 2,660 across 3 histone marks | 3,420 across 3 histone marks |
| Cells Passing QC | 60.2% - 77.9% | 35.4% - 40.6% |
| CpGs Detected per Cell | > 50,000 | Data not specified |
| Average FRiP | 0.72 - 0.88 | Data not specified |
| TAPS Conversion Rate | ~95% | Data not specified |
Integrated Multi-Omic Analysis in Complex Tissues
The power of single-cell multi-omics extends to complex tissues and disease contexts, such as the intestinal mucosa, where host and microbiome interactions are direct. A seminal study on paediatric ulcerative colitis (UC) combined mucosal microbiome profiling with host epigenomics and transcriptomics from intestinal biopsies [43].
- Experimental Design: The study analyzed 201 biopsies from 56 treatment-naïve children with UC. Multi-omics data included:
- Mucosal Microbiome: 16S rRNA sequencing to determine microbial diversity and composition.
- Host Epigenome: DNA methylation profiling.
- Host Transcriptome: Gene expression profiling [43].
- Data Integration and Findings: Machine learning models integrating microbiome and epigenome data outperformed models using either dataset alone in predicting future clinical relapse. This integration revealed that children who relapsed had lower bacterial diversity and specific microbial shifts, including fewer butyrate producers (e.g., F. prausnitzii, E. rectale) and an increase in oral-associated bacteria like Veillonella parvula, which was shown to induce pro-inflammatory responses in experimental models [43]. This demonstrates how multi-omics can directly link specific microbial taxa to host immune responses and clinical outcomes through epigenetic and transcriptional pathways.
High-Throughput Methylation Mapping Platforms
The Methylation Screening Array (MSA): A Targeted, Ternary-Code Platform
The Methylation Screening Array (MSA) represents a conceptual shift in array-based epigenomics, moving from broad genomic coverage to targeted, trait-associated profiling with the ability to distinguish between cytosine modifications [44].
- Design Philosophy and Probe Content: Unlike previous arrays like the Illumina Infinium BeadChip, which prioritized wide genomic coverage, the MSA condenses probe content to 284,317 probes specifically curated and prioritized from over 1,000 EWAS publications and high-resolution methylome studies. This design enriches for trait-associated and cell-type-specific CpG sites, including those from rare cell types like neuronal subpopulations [44].
- Discrimination of 5mC and 5hmC: A major innovation of the MSA is its partnership with the bisulfite-APOBEC3A deamination (bACE-seq) protocol. This combination allows for the scalable dissection of the "ternary methylation code," generating matched profiles for total cytosine modification (5modC, representing 5mC + 5hmC) and 5-hydroxymethylcytosine (5hmC) from the same sample [44]. This is a significant advance because 5hmC, enriched in brain and other tissues, is a stable epigenetic mark with distinct regulatory roles but was previously indistinguishable from 5mC in standard bisulfite-based arrays.
- Utility in Context-Aware EWAS: The MSA's enriched content enables more accurate interpretation of EWAS findings within their tissue and cell-type context. For example, the platform demonstrates that CpGs associated with Alzheimer's disease show the most variable methylation in brain tissue, while those linked to irritable bowel syndrome are most dynamic in the colon [44].
Table 2: Comparison of Methylation Screening Array (MSA) with Illumina EPICv2
| Feature | Methylation Screening Array (MSA) | Illumina EPICv2 Array |
|---|---|---|
| Number of Probes | 284,317 | > 900,000 |
| Probe Selection Strategy | Trait-associated and cell-type-specific loci from curated literature/databases | Broad, even genomic coverage |
| CpG Context | Tertiary code (5mC, 5hmC, unmodified C) | Binary code (5modC vs. unmodified C) |
| 5hmC Detection | Yes, via integrated bACE-seq protocol | No |
| Primary Application | Trait-centric EWAS, functional screening | Broad discovery EWAS |
| Sample Throughput | 48-sample format | 96-sample format |
High-Throughput Methylation Analysis for Newborn Screening
Automated, high-throughput methylation analysis is also making its way into clinical screening applications. A 2025 study compared two automated systems for bisulfite conversion and quantitative melt analysis—the magnetic-bead-based IsoPure and the column-based QIAcube HT—for methylation-based newborn screening of fragile X syndrome (FMR1) and chromosome 15 imprinting disorders (SNRPN) from archival blood spots [45].
- Performance Comparison: Both methods achieved 100% diagnostic sensitivity and specificity on fresh samples. However, the IsoPure system demonstrated superior performance on archival samples stored for over 10 years, with significantly lower reaction failure rates (0.365% for SNRPN and 0.74% for FMR1) compared to the QIAcube HT (19.34% and 2.56%, respectively) [45]. This highlights the critical importance of platform selection when working with challenging sample materials like archival dried blood spots.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for Single-Cell Multi-Omics and Methylation Mapping
| Reagent / Material | Function | Example Use Case |
|---|---|---|
| pA-MNase fusion protein | Enzyme-antibody fusion that cleaves DNA around specific histone modifications. | Targeted chromatin cleavage in scEpi2-seq for mapping histone marks [42]. |
| TAPS Reagents | Enzymatic conversion kit for detecting 5mC without DNA degradation. | Gentle and efficient methylation calling in scEpi2-seq and MSA/bACE workflows [42] [44]. |
| Bisulfite Conversion Kits | Chemical conversion of unmethylated cytosine to uracil for standard methylation analysis. | DNA methylation analysis in newborn screening and other bisulfite-dependent protocols [45]. |
| Methylation Screening Array (MSA) | Next-generation BeadChip for targeted, high-throughput profiling of 5mC and 5hmC. | Trait-centric EWAS in large cohort studies [44]. |
| Single-cell Bisulfite Sequencing Kits | Kits for whole-genome methylation sequencing at single-cell resolution. | Constructing methylation profiles of super-enhancers in muscle stem cells [46]. |
| ALLCools package | Bioinformatics tool for processing and analyzing single-cell methylation data. | Analysis of scBS-seq data to identify differentially methylated regions [46]. |
Detailed Experimental Protocols
Protocol: scEpi2-seq for Joint Histone and DNA Methylation Profiling
This protocol outlines the key steps for simultaneous profiling of histone modifications and DNA methylation in single cells [42].
- Cell Preparation and Permeabilization: Harvest and wash cells. Permeabilize cells to allow antibody access to nuclear antigens.
- Antibody Incubation: Incubate cells with specific primary antibodies against the histone mark of interest (e.g., H3K27me3).
- pA-MNase Binding: Add the pA-MNase fusion protein, which binds to the primary antibodies.
- Single-Cell Sorting: Use Fluorescence-Activated Cell Sorting (FACS) to sort individual cells into a 384-well plate containing a mild lysis buffer.
- MNase Digestion: Initiate targeted chromatin cleavage by adding Ca²⁺, the essential cofactor for MNase. This releases DNA fragments bound to the modified histones.
- Library Preparation for Chromatin Modality:
- Repair and A-tail the MNase-released DNA fragments.
- Ligate adaptors containing a single-cell barcode, a Unique Molecular Identifier (UMI), a T7 promoter, and Illumina sequencing handles.
- TAPS Conversion for Methylation Modality: Pool material from the 384-well plate and subject it to TET-assisted pyridine borane sequencing (TAPS). This step chemically converts 5mC to uracil, preserving the adaptor sequences.
- Final Library Preparation and Sequencing:
- Perform in vitro transcription (IVT) from the T7 promoter.
- Conduct reverse transcription and PCR amplification to generate the final sequencing library.
- Sequence using paired-end sequencing on an Illumina platform.
Protocol: Super-Enhancer Methylation Analysis in Stem Cells
This protocol describes a bioinformatic workflow for identifying and analyzing the methylation profile of super-enhancers using public and newly generated data, as applied to skeletal muscle stem cells (MuSCs) [46].
- Data Acquisition:
- Download H3K27ac ChIP-seq data from the ENCODE database to define enhancer regions.
- Obtain single-cell bisulfite sequencing (scBS-seq) data from the Gene Expression Omnibus (GEO) for methylation analysis.
- Super-Enhancer Identification:
- Use the ROSE software in a Python environment to identify super-enhancers from the H3K27ac ChIP-seq data.
- Rank enhancers by H3K27ac signal intensity, stitch enhancers within 12.5 kb, and identify the inflection point to define SEs.
- Methylation Data Processing:
- Align scBS-seq reads to a reference genome (e.g., mm10 for mouse) using Bismark.
- Process BAM files (filter, sort, remove duplicates) and generate ALLC files (base-level methylation information) using the ALLCools package.
- Integration and Differential Analysis:
- Integrate the SE genomic locations with the single-cell methylation data from ALLC files.
- Identify Differentially Methylated Regions (DMRs) between conditions (e.g., aged vs. young) within SEs using statistical packages like Methylpy.
- Functional Annotation:
- Animate SE-associated target genes using algorithms from Young's laboratory.
- Perform motif enrichment analysis within SEs using HOMER.
- Conduct functional pathway analysis (KEGG, GO) on SE-target genes using ClusterProfiler.
The integration of single-cell multi-omics and high-throughput methylation mapping is providing an unprecedented, high-resolution view of the dynamic interplay between the gut microbiome and the host epigenome. Tools like scEpi2-seq allow for the direct observation of how microbial signals correlate with coordinated changes in histone modifications and DNA methylation within individual cells. Meanwhile, platforms like the MSA enable large-scale, cost-effective screening of methylation patterns associated with microbiome-driven traits across diverse populations. As these technologies continue to mature and become more accessible, they will accelerate the translation of basic research into clinical applications, such as microbiome-informed diagnostics, live biotherapeutic products, and dietary interventions designed to favorably modulate the host epigenome for improved health outcomes [1] [47]. The future of this field lies in further refining these tools to capture even more layers of regulatory complexity and in applying them within robust longitudinal studies to decipher the causal pathways linking specific microbial members to host epigenetic reprogramming in health and disease.
The Role of Artificial Intelligence in Modeling Complex Host-Microbe Interactions
The human gut microbiome, a complex ecosystem of bacteria, viruses, fungi, and other microorganisms, exerts profound influence on host physiology through multiple mechanisms, including the modulation of the host epigenome [2]. This microbial consortium regulates host epigenetic mechanisms such as DNA and RNA methylation, shaping gene expression and phenotypic plasticity in response to environmental factors like diet and microbial metabolites [2]. Understanding these interactions is critical for advancing precision medicine, yet their inherent complexity—involving high-dimensional data, dynamic feedback loops, and cross-kingdom communication—presents formidable analytical challenges.
Artificial intelligence (AI) has emerged as a transformative tool to decipher this complexity. By leveraging machine learning (ML) and deep learning (DL), AI can identify intricate patterns within large-scale multi-omics datasets that traditional statistical methods often miss [48] [49]. The integration of AI is particularly crucial for moving beyond correlative studies toward causal inference and predictive modeling in host-microbe-epigenome interactions [50]. This technical guide details how AI methodologies are enabling a systems-level understanding of how microbial communities influence host epigenetic landscapes, thereby accelerating the development of microbiome-based diagnostics and therapeutics.
AI and Multi-Omics Data Integration for Hypothesis Generation
The application of AI in host-microbe research begins with the integration of heterogeneous, high-volume datasets. Sequencing techniques and metabolomics generate vast amounts of information on microbial community structure, gene function, and metabolic output, which AI tools are uniquely positioned to analyze [49].
Machine Learning for Pattern Recognition and Biomarker Discovery
Machine learning algorithms excel at identifying microbial signatures associated with specific host states, including epigenetic markers.
- Classification Models: Supervised learning models are trained on metagenomic data to distinguish between health and disease states. For example, Support Vector Machines (SVM), Random Forests, and Graph Neural Networks have been used to diagnose diseases like colorectal cancer and liver cirrhosis based on gut microbiome composition, with area under the receiver operating characteristic curve (AUROC) values often exceeding 0.8 [48].
- Interpretable AI: The "black box" nature of complex AI models is a limitation for clinical adoption. Techniques like SHapley Additive exPlanations (SHAP) provide local explanations for model predictions, identifying which bacterial species (e.g., Fusobacterium nucleatum in colorectal cancer) contributed most to an individual's diagnosis, thereby revealing personalized biomarkers [48].
- Network-Based Analysis: Advanced models like the Weighted Signed Graph Convolutional Neural Network for Microbial Biomarker Identification (WSGMB) analyze microbial co-occurrence networks rather than just abundance. By perturbing microbial nodes in a network, this method can identify disease-related microbes with an AUROC of >0.7 for known colorectal cancer-related bacteria, offering insights into community-level disruptions [48].
Table 1: Machine Learning Models in Microbiome-Based Disease Diagnosis
| ML Model | Application | Key Microbiome Features | Performance (AUROC) |
|---|---|---|---|
| Support Vector Machine (SVM) | Diagnosing liver cirrhosis [48] | 15 gut microbiome biomarkers | 0.838 |
| Graph Neural Network | Predicting 9 health phenotypes (8 diseases + healthy) [48] | Species-level faecal microbiome profiles | 0.67 - 0.90 (across phenotypes) |
| Random Forest with SHAP | Diagnosing Colorectal Cancer (CRC) & identifying personalized biomarkers [48] | Abundance of species like Fusobacterium nucleatum | Not Specified |
| Weighted Signed GCNN (WSGMB) | Identifying CRC-related bacteria via microbial interactions [48] | Microbial co-occurrence networks | >0.7 |
Genome-Scale Metabolic Modeling (GEM) Enhanced by AI
Genome-scale metabolic models (GEMs) provide a mathematical framework to investigate host-microbe interactions at a systems level by simulating metabolic fluxes and cross-feeding relationships [51] [52]. GEMs are built from annotated genomes and represent the complete set of metabolic reactions within an organism.
- Model Reconstruction and Integration: The process involves:
- Reconstruction: Collecting genomic data and using automated pipelines (e.g., ModelSEED, CarveMe, RAVEN) or manual curation to generate metabolic models for host and microbial species [51].
- Integration: Combining individual models into a unified host-microbiota model, which requires standardizing nomenclatures using resources like MetaNetX and removing thermodynamically infeasible reactions [51].
- Simulation and Analysis: Integrated models are simulated using Constraint-Based Reconstruction and Analysis (COBRA) methods. A core technique is Flux Balance Analysis (FBA), which optimizes an objective function (e.g., maximum biomass production) to predict flux distributions through the metabolic network under steady-state assumptions [51].
- AI's Enhancing Role: While GEMs are powerful, AI enhances their utility by processing the vast, multi-omic data required to constrain and validate these models. AI tools can predict enzyme kinetics and reaction rates from omics data, thereby refining the model's constraints and improving the accuracy of metabolic flux predictions in the holobiont system [51].
Experimental Protocols for Validating AI-Generated Hypotheses
AI models generate hypotheses that require rigorous experimental validation. The following protocols outline key methodologies for confirming the functional impact of AI-predicted host-microbe-epigenome interactions.
Protocol: Validating Microbial Metabolite-Induced Epigenetic Changes
Objective: To experimentally verify that microbial metabolites, identified by AI models, directly cause host epigenetic reprogramming.
In Vitro Cell Culture Treatment
- Cell Line Selection: Use relevant host cell lines (e.g., intestinal epithelial cells, immune cells, or patient-derived organoids).
- Metabolite Exposure: Treat cells with physiological concentrations of short-chain fatty acids (SCFAs) like butyrate or other AI-predicted microbial metabolites (e.g., from polyamine biosynthesis or one-carbon metabolism pathways) [2].
- Control Groups: Include untreated controls and cells treated with non-bioactive compounds.
Epigenomic Analysis
- DNA Methylation Profiling: Perform whole-genome bisulfite sequencing (WGBS) to map 5-methylcytosine (5mC) patterns after metabolite exposure [2].
- Histone Modification Analysis: Use chromatin immunoprecipitation followed by sequencing (ChIP-seq) for marks like H3K27ac, which are influenced by microbial SCFAs [2].
- RNA Methylation Analysis: Employ miCLIP or MeRIP-seq to profile modifications such as N6-methyladenosine (m6A) [2].
Functional Transcriptomic and Phenotypic Assays
- RNA-seq: Conduct transcriptomic profiling to link epigenetic changes to altered gene expression.
- Phenotypic Assays: Assess functional outcomes such as barrier integrity (Transepithelial Electrical Resistance), proliferation, or cytokine secretion.
Protocol: Spatial Profiling of Host-Microbe-Epigenome Interactions
Objective: To characterize the spatial relationships between specific microbes, host cell types, and epigenetic marks within a tissue context, moving beyond bulk tissue analysis.
Sample Preparation and Sectioning
- Tissue Collection: Preserve gut tissue samples from animal models or human biopsies, optimally using methods that retain RNA and protein integrity (e.g., flash-freezing or specific fixatives).
- Cryosectioning: Generate thin tissue sections (5-10 μm) for downstream staining.
Spatial Multi-omics
- Spatial Metatranscriptomics: Utilize technologies like Visium Spatial Gene Expression to simultaneously map active microbial communities and host gene expression profiles across the tissue architecture [50].
- Multiplexed Fluorescent In Situ Hybridization (FISH): Employ techniques to visually identify and localize specific bacterial taxa (e.g., with 16S rRNA-targeting probes) alongside host nuclei [50].
Spatial Epigenomics and Integration
- Immunofluorescence (IF) Staining: Use antibodies against specific histone modifications (e.g., H3K4me3, H3K27me3) or DNA methylation marks on adjacent tissue sections.
- Data Integration: Correlate the spatial localization of microbes with the epigenetic and transcriptomic states of neighboring host cells using computational image analysis and AI-based data fusion tools [50].
The Scientist's Toolkit: Key Research Reagents and Platforms
Table 2: Essential Research Reagents and Platforms for AI-Driven Host-Microbe-Epigenome Studies
| Category & Item | Function & Application | Example Tools / Sources |
|---|---|---|
| Computational Modeling & Analysis | ||
| Genome-Scale Metabolic Model (GEM) | Mathematical framework to simulate metabolic interactions between host and microbes [51] [52]. | AGORA, BiGG, Recon3D, ModelSEED, CarveMe |
| Constraint-Based Analysis Software | Simulates metabolic fluxes in GEMs using linear programming [51]. | COBRA Toolbox |
| AI/ML Model Interpretation | Explains output of complex AI models, identifying key predictive features [48]. | SHAP (SHapley Additive exPlanations) |
| Multi-Omic Wet Lab Reagents | ||
| Spike-in Bacteria / Internal Standards | Added to samples to normalize for microbial load and technical variation, critical for AI model accuracy [50]. | Commercial synthetic communities (e.g., ZymoBIOMICS) |
| Antibodies for Histone Modifications | Detect specific chromatin marks (e.g., H3K9ac, H3K27me3) in spatial and ChIP-seq assays [2]. | Various commercial suppliers |
| FISH Probes for Bacterial Taxa | Visually localize specific microbes in tissue sections for spatial analysis [50]. | Custom-designed 16S/23S rRNA probes |
| Data Resources & Databases | ||
| Curated Metabolic Model Repository | Source of pre-built, quality-controlled metabolic models for integration [51]. | AGORA, BiGG, APOLLO |
| Comprehensive Antibiotic Resistance Database | Reference for annotating antimicrobial resistance genes in metagenomic data [50]. | CARD |
| Standardized Microbiome Protocols | Ensure reproducibility in sample collection, DNA extraction, and sequencing [50]. | International Human Microbiome Standards (IHMS) |
The synergy between AI and experimental microbiome research is poised to unlock a new era of precision medicine. Future advancements will depend on several key areas:
- Causal Inference Frameworks: Integrating Mendelian randomization and other causal inference methods with AI models will be crucial to distinguish true microbial drivers of epigenetic change from mere correlations [50].
- Enhanced GEMs with AI: Future GEMs will be more dynamically constrained by AI-predicted parameters from real-time, multi-omic data, creating more predictive "digital twins" of the holobiont [51].
- Standardization and Rigor: Adherence to standardized protocols (e.g., STORMS checklist) and robust analytical practices is non-negotiable for generating high-quality, reproducible data for AI training [50].
In conclusion, AI is not merely an analytical tool but a catalyst for a fundamental shift in how we study host-microbe-epigenome interactions. By bridging computational prediction with mechanistic experimental validation, researchers can translate complex biological relationships into actionable insights for diagnostics, microbial therapeutics, and personalized health strategies.
Live biotherapeutic products (LBPs) and engineered probiotics represent a frontier in targeting the gut microbiome to influence host epigenetics. These interventions leverage microbial viability, genetic precision, and metabolic activity to correct dysbiosis-induced epigenetic dysregulation, such as aberrant DNA methylation and histone modifications. This review synthesizes current advances in LBP design, efficacy data, and mechanistic pathways linking microbial signals to host epigenome reprogramming. We also provide standardized protocols and toolkits to facilitate translational research.
The gut microbiome regulates host physiology through epigenetic mechanisms, including DNA methylation, histone modifications, and non-coding RNA expression [11] [53]. Microbial metabolites (e.g., short-chain fatty acids/SCFAs) serve as substrates for epigenetic enzymes, while dysbiosis disrupts these pathways, contributing to inflammatory bowel disease (IBD), colorectal cancer, and neurological disorders [11] [54]. LBPs and engineered probiotics are designed to restore microbial balance and deliver targeted epigenetic modifiers.
Current Landscape of Live Biotherapeutics
Definitions and Regulatory Status
- LBPs: Pharmaceutical products containing live microorganisms (e.g., bacteria) for disease treatment, regulated under FDA drug pathways.
- Probiotics: Dietary supplements for general health, not requiring drug approval [55]. Table: Differentiating LBPs from Probiotics
| Feature | Live Biotherapeutic Products (LBPs) | Conventional Probiotics |
|---|---|---|
| Regulatory Pathway | FDA pharmaceutical approval | Dietary supplement guidelines |
| Target Population | Diseased individuals (e.g., IBD, rCDI) | Healthy populations |
| Efficacy Evidence | Clinical trials for specific indications | General health claims |
| Examples | MTC01 (15-strain consortium), SER-109 | Lactobacillus spp., Bifidobacterium spp. |
Efficacy and Challenges in Inflammatory Diseases
Meta-analyses reveal that LBPs show limited efficacy in active inflammatory diseases like ulcerative colitis due to colonization resistance and microbial inactivation in inflamed guts [55]. For example, Escherichia coli Nissle 1917 fails to induce remission in active IBD but maintains remission in non-inflamed states [55]. In recurrent Clostridioides difficile infection (rCDI), LBPs like MTC01 demonstrate comparable efficacy to fecal microbiota transplantation (FMT) with superior engraftment [56].
Engineering Strategies for Next-Generation Probiotics
Genetic and Evolutionary Engineering
- CRISPR-Cas Systems: Knock in genes for SCFA production (e.g., butyrate synthases) or epigenetic enzyme delivery [57].
- In Vivo Domestication: Sequential passaging of probiotics (e.g., Lactiplantibacillus plantarum) in host guts selects mutants with enhanced acid resistance and colonization traits [58].
- Synthetic Biology Circuits: Engineer sense-and-respond systems activated by disease biomarkers (e.g., inflammation-linked mRNAs).
Formulation and Delivery Technologies
Microbiome-active drug delivery systems (MADDS) use:
- Polymer-based encapsulation (e.g., chitosan) to protect probiotics from gastric acid.
- Quorum-sensing triggers for localized drug release in the gut [59].
Epigenetic Mechanisms of Microbiome-Based Interventions
Key Microbial Metabolites and Epigenetic Modifications
Table: Microbial Metabolites and Their Epigenetic Roles
| Metabolite | Producing Bacteria | Epigenetic Mechanism | Host Effect |
|---|---|---|---|
| Butyrate | Faecalibacterium prausnitzii | HDAC inhibition; histone hyperacetylation | Anti-inflammation; neural function [11] [54] |
| Folate | Bifidobacterium spp. | Methyl donor for DNA methylation | Immune cell differentiation [53] |
| S-adenosylmethionine (SAM) | Lactobacillus spp. | Substrate for DNMTs (DNA methylation) | Gene silencing in IBD/CRC [11] |
| Propionate | Bacteroides spp. | HDAC inhibition; histone lactylation | Metabolic regulation [53] |
Signaling Pathways in Microbiome-Epigenome Crosstalk
The diagram below illustrates how gut microbiota signals influence the host epigenome:
Title: Microbiome-Epigenome Signaling Pathway
Experimental Protocols for Efficacy Validation
In Vivo LBP Domestication and Engraftment Assay
Objective: Evolve probiotics for enhanced gut persistence [58]. Steps:
- Administration: Gavage mice with Lactiplantibacillus plantarum (10^9 CFU/day).
- Fecal Sampling: Collect daily feces, isolate bacterial colonies on selective media.
- Genomic Analysis:
- Short-read sequencing (Illumina) to identify single-nucleotide variants (SNVs).
- Long-read sequencing (Nanopore) to detect structural variations (SVs).
- Reinoculation: Administer evolved strains to new hosts; track colonization via qPCR.
Epigenetic Impact Assessment
Method:
- Tissue Collection: Isolate intestinal epithelial cells (IECs) from germ-free vs. LBP-treated mice.
- DNA Methylation Profiling:
- Whole-genome bisulfite sequencing (WGBS) to map 5-methylcytosine.
- Identify differentially methylated regions (DMRs) near IBD/CRC-related genes.
- Histone Modification Analysis:
- Chromatin immunoprecipitation (ChIP-seq) for H3K27ac marks.
- Functional Validation:
- Treat IEC organoids with SCFAs; assay gene expression via RNA-seq.
Table: Essential Reagents for LBP and Epigenetics Research
| Reagent/Technology | Function | Examples/Sources |
|---|---|---|
| Gnotobiotic Mice | Define causality in microbiome-epigenome interactions | Germ-free C57BL/6 models [11] |
| Single-Cell Multi-omics | Simultaneously profile microbiome/transcriptome | 10x Genomics scRNA-seq + ATAC-seq |
| HDAC/DNMT Inhibitors | Validate metabolite-epigenetic enzyme links | Sodium butyrate, 5-azacytidine |
| Synthetic Consortia | Test LBP interactions in reduced complexity | MTC01 (15-strain LBP for rCDI) [56] |
| Metabolomics Kits | Quantify SCFAs, SAM, folate in gut contents | GC-MS, LC-MS platforms |
LBPs and engineered probiotics offer a scalable, targeted approach to correct epigenetic dysregulation. Key priorities include:
- Personalization: Match LBPs to host microbiome/genetic background [57].
- Delivery Innovation: Use MADDS for spatial control in the gut [59].
- Safety: Address horizontal gene transfer risks in engineered strains [58]. By integrating microbial ecology, epigenetics, and bioengineering, these strategies will advance precision medicine for microbiome-related diseases.
The therapeutic application of Fecal Microbiota Transplantation (FMT) is undergoing a pivotal transformation, moving from a broad-spectrum intervention to a precision tool guided by biomarker discovery. This evolution is critically framed within the broader thesis of gut microbiome's impact on the host epigenome. The gut microbiome regulates host physiological processes through epigenetic mechanisms such as DNA methylation and histone modification, primarily via microbiota-derived metabolites (MDMs) [1]. This interaction forms what recent research has termed the "MDMs–epigenetic (MDME) axis" [4], a conceptual framework essential for understanding how FMT-induced microbial changes can produce durable therapeutic effects through epigenetic reprogramming.
The efficacy of FMT varies substantially across different disease states. While it achieves remarkable >90% success rates in acute conditions like recurrent Clostridium difficile infection, its effectiveness diminishes to >60% for intestinal functional diseases, <60% for chronic intestinal inflammations, and <50% for extraintestinal diseases without gastrointestinal symptoms [60]. This variability underscores the critical need for biomarkers that can predict treatment response and guide patient selection. Current research focuses on identifying translatable biomarkers to enable precision use of microbiota-directed therapies [61], ultimately allowing clinicians to target FMT to patient subpopulations most likely to achieve durable remission.
Biomarker Discovery for Predicting FMT Response
Serum and Metabolic Biomarkers
Serum and metabolic biomarkers offer promising non-invasive approaches for predicting FMT success. The most significant recent advancement comes from a 2025 cohort study investigating bile acid malabsorption (BAM) in inflammatory bowel disease (IBD) patients.
Table 1: Serum and Metabolic Biomarkers for FMT Response Prediction
| Biomarker Category | Specific Marker | Predictive Value | Mechanistic Insight | Clinical Context |
|---|---|---|---|---|
| Serum Bile Acid Precursor | Serum 7α-hydroxy-4-cholesten-3-one (C4) [61] | High C4 predicts better clinical response and remission in IBD patients with BAM [61] | Reflects hepatic bile acid synthesis; decreases significantly post-FMT (P < 0.001) [61] | Especially predictive in Crohn's disease with ileal resection or ileal/ileocolonic type [61] |
| Serum Lipidome | Specific lipid profiles [61] | Potential diagnostic potential in bile acid diarrhoea [61] | Linked to bile acid metabolism pathways [61] | Emerging biomarker requiring further validation |
| Inflammatory Cytokines | Serum IL-6, IL-10, TNF-α [62] | Modification predicted to be related to FMT efficacy in Ulcerative Colitis [62] | Indicates systemic immunomodulatory effects of FMT [62] | Suggests immune profiling as a complementary predictive strategy |
The 2025 clinical trial demonstrated that IBD patients with BAM, identified by serum C4, achieved superior clinical response (66.67% vs. 49.41%) and remission (52.38% vs. 40.00%) at 3 months post-FMT compared to non-BAM patients [61]. This positions serum C4 as a leading translatable biomarker for precision FMT application.
Microbial Diversity and Taxonomic Biomarkers
Baseline microbial features and their dynamic changes following FMT provide powerful predictors of treatment outcome. Systematic analyses reveal consistent patterns across multiple studies.
Table 2: Microbial Biomarkers of FMT Response
| Microbial Feature | Association with FMT Response | Clinical Context | Supporting Evidence |
|---|---|---|---|
| Pre-FMT Alpha Diversity | Higher fecal species richness at baseline predicts response [63] | Ulcerative Colitis [63] | Systematic Review |
| Post-FMT Alpha Diversity | Increase in alpha diversity post-FMT associated with response [63] [62] | CDI and Ulcerative Colitis [63] [62] | Multiple Clinical Trials |
| Specific Taxa Enrichment (Post-FMT) | Clostridiales clusters (order), Bacteroides genus, Ruminococcaceae, Lachnospiraceae [63] [62] | Ulcerative Colitis and CDI [63] [62] | Systematic Review, Cohort Studies |
| Specific Taxa Depletion (Post-FMT) | Enterobacteriaceae [62], Proteobacteria [63] [62] | CDI and Ulcerative Colitis [63] [62] | Systematic Review, Cohort Studies |
| Donor-Recipient Similarity | Baseline similarity between recipient and donor microbiota predicts response [63] | Ulcerative Colitis [63] | Systematic Review |
Random forest classifiers have successfully utilized differential Operational Taxonomic Units (OTUs) to predict BAM in IBD patients, achieving an area under the curve (AUC) of 0.92 with 18 OTUs and 0.83 with the top 4 OTUs [61]. This demonstrates the potential for minimal microbial signatures to guide clinical decision-making.
Metabolomic Biomarkers
Metabolites serve as functional readouts of microbial activity and host-microbe interactions. Short-chain fatty acids (SCFAs)—including butyrate, acetate, and propionate—are consistently identified as critical metabolomic biomarkers for FMT success [63]. Butyrate, in particular, demonstrates an inverse correlation with symptom severity in conditions like irritable bowel syndrome (IBS) [62]. SCFAs are not only endpoints but also active mediators of therapeutic effects, in part through their influence on host epigenetic mechanisms [1].
The Epigenetic Interface: Connecting Microbiota to Host Physiology
The MDME axis represents the core mechanistic pathway through the gut microbiome influences host gene expression and health outcomes. FMT exerts its therapeutic effects significantly through this axis by altering the production of microbiota-derived metabolites that serve as epigenetic substrates or inhibitors.
The MDME axis illustrates the sequential pathway from FMT intervention to physiological outcome, with metabolite-mediated epigenetic regulation as the crucial intermediary step. Key metabolite classes involved in this epigenetic regulation include:
- Short-chain fatty acids (SCFAs): Butyrate functions as a histone deacetylase (HDAC) inhibitor, while acetate serves as a substrate for histone acetyltransferases (HATs), directly influencing chromatin accessibility and gene expression [1].
- One-carbon metabolites: Folate and other metabolites involved in one-carbon metabolism provide methyl donors for DNA methylation processes, directly linking microbial metabolism to epigenetic marking [1].
- Polyamines: Spermidine and related compounds can influence histone acetylation and have been implicated in cellular longevity pathways [1].
This epigenetic machinery explains how FMT can produce sustained therapeutic benefits even after the initial microbial community changes have stabilized—through durable reprogramming of host gene expression patterns.
Experimental Workflows for Biomarker Discovery
Integrated Multi-Omics Pipeline
A comprehensive approach to FMT biomarker discovery requires the integration of multiple analytical platforms.
This workflow outlines the core parallel processes of microbiome and metabolome analysis that must be integrated for comprehensive biomarker discovery. Key methodological details for each stage include:
- Sample Collection: Sequential fecal and serum samples collected pre- and post-FMT (e.g., at screening, every 4 weeks during treatment, and 8 weeks after FMT therapy) [61]. Samples must be immediately processed or frozen at -80°C to preserve microbial composition and metabolite integrity.
- DNA Extraction and 16S rRNA Sequencing: Microbial DNA is extracted using standardized kits (e.g., QIAamp PowerFecal Pro DNA Kit). The 16S rRNA gene (V3-V4 region) is amplified and sequenced on platforms such as Illumina MiSeq, followed by bioinformatic processing using QIIME 2 or Mothur pipelines [61].
- Untargeted Metabolomics: Liquid chromatography-mass spectrometry (LC-MS) performed on platforms like Thermo Q-Exactive HF-X. Chromatographic separation typically uses C18 columns with gradient elution (water/acetonitrile both with 0.1% formic acid). Data processing utilizes software such as XCMS or Progenesis QI [61].
- Data Integration and Biomarker Identification: Multi-omics data integration through multivariate statistics (PLS-DA), correlation networks, and machine learning classifiers (Random Forest). Biomarker panels are validated in independent cohorts [61] [63].
In Vivo Validation Models
Promising biomarkers from human observational studies require validation in controlled animal models to establish causality. The following protocol has been successfully employed:
- Animal Model Selection: C57BL/6 mice (8-10 weeks old) are commonly used for colitis studies [61].
- Colitis Induction: Administration of primary bile acids (e.g., cholic acid) or dextran sulfate sodium (DSS) in drinking water to induce colitis phenotypes [61].
- FMT Intervention: Mice receive FMT from human donors (either responsive or non-responsive profiles) via oral gavage daily for 5-7 days.
- Outcome Assessment: Disease activity index (weight loss, stool consistency, bleeding), histological scoring of colon tissue, and analysis of biomarker levels (e.g., serum C4) [61].
This approach has confirmed that primary bile acid-induced colitis in mice can be exacerbated by specific microbial profiles and treated by FMT, reinforcing human findings [61].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for FMT Biomarker Discovery
| Reagent / Solution | Manufacturer Examples | Critical Function | Application Notes |
|---|---|---|---|
| QIAamp PowerFecal Pro DNA Kit | QIAGEN | Standardized microbial DNA extraction from complex fecal samples | Ensures high yield and reproducibility for downstream sequencing [61] |
| 16S rRNA Gene Primers (V3-V4) | Custom synthesized | Amplification of hypervariable regions for bacterial community profiling | Primers 341F/806R commonly used; critical for taxonomic resolution [61] |
| MiSeq Reagent Kit v3 | Illumina | 16S rRNA amplicon sequencing | 600-cycle kit typically used for paired-end 2x300 bp sequencing [61] |
| Bioinformatic Pipelines (QIIME 2) | Open source | Processing raw sequencing data into analyzed microbial communities | Incorporates DADA2 for ASV calling; superior to OTU-based methods [61] |
| C18 LC Columns (e.g., Hypersil Gold) | Thermo Scientific | Chromatographic separation for untargeted metabolomics | 1.9μm particle size, 100mm x 2.1mm dimensions recommended [61] |
| Serum C4 ELISA Kits | Commercial suppliers | Quantification of 7α-hydroxy-4-cholesten-3-one | Critical for bile acid malabsorption assessment; requires validation [61] |
| SCFA Standards (Butyrate, Acetate, Propionate) | Sigma-Aldrich | Reference standards for quantification in metabolomic studies | Used for calibration curves in GC-MS or LC-MS analyses [63] |
The discovery and validation of biomarkers for FMT response represent a fundamental shift toward precision microbiome medicine. The integration of serum, microbial, and metabolomic biomarkers provides a multidimensional assessment that can accurately identify patients most likely to benefit from FMT. The MDME axis provides the mechanistic link between microbial restructuring and durable host physiological changes, positioning FMT as a powerful intervention capable of reprogramming host physiology through epigenetic mechanisms. As biomarker panels become refined and validated, the field moves closer to realizing a truly personalized, biomarker-driven 'treat to microbiome/metabolome' target approach that maximizes therapeutic efficacy while minimizing unnecessary treatments and associated risks.
The human gut microbiome, a complex ecosystem of bacteria, viruses, fungi, and other microorganisms, exerts a profound influence on host physiology and disease susceptibility. A key mechanism through which it achieves this is by modulating the host epigenome—a collection of heritable changes in gene expression that occur without altering the underlying DNA sequence [11] [2]. Historically, research has focused on how microbial signals shape host epigenetic marks. However, a new paradigm is emerging: the deliberate manipulation of these host epigenetic pathways to steer microbial community composition and function, a field we term Epigenetic Engineering. This approach recognizes the relationship as fundamentally bidirectional; just as the microbiome calibrates host transcriptional programs, the host's epigenetically regulated responses—particularly in intestinal epithelial and immune cells—create a microenvironment that selectively encourages or discourages specific microbial residents [2]. This technical guide explores the core mechanisms, methodologies, and therapeutic potential of engineering the host epigenome to shape our microbial partners, framed within the broader context of gut microbiome and host epigenome research.
Foundational Mechanisms of Microbiome-Epigenome Communication
The gut microbiota influences the host epigenome through several primary mechanisms, with microbial metabolites serving as key intermediary signals. Understanding these pathways is a prerequisite for their targeted manipulation.
Key Microbial Metabolites and Epigenetic Modifications
The table below summarizes the major microbial metabolites involved in epigenetic regulation and their effects on the host.
Table 1: Key Microbiota-Derived Metabolites and Their Epigenetic Effects
| Metabolite | Producing Bacteria (Examples) | Epigenetic Mechanism | Host Gene/Pathway Affected | Functional Outcome |
|---|---|---|---|---|
| Short-Chain Fatty Acids (SCFAs): Butyrate, Propionate | Faecalibacterium prausnitzii, Eubacterium rectale, Ruminococcus [11] [43] | Inhibition of Histone Deacetylases (HDACs); Regulation of DNA methyltransferases (DNMTs) [11] | Immune pathways; Inflammation genes [11] | Enhanced gut barrier integrity; anti-inflammatory effects; immune regulation [11] [64] |
| Folate | Various gut microbes [11] | Serves as methyl donor for one-carbon metabolism, influencing DNA methylation [11] | Global DNA methylation patterns [11] | Cellular proliferation and differentiation |
| S-adenosylmethionine (SAM) | Various gut microbes [11] | Primary methyl donor for DNA and histone methyltransferases [11] | Global DNA and histone methylation [11] | Regulation of gene expression and chromatin structure |
DNA Methylation and Histone Modifications
DNA methylation, involving the addition of a methyl group to cytosine bases in CpG dinucleotides, is a well-studied epigenetic mark heavily influenced by the microbiome. Conventionally raised mice exhibit significantly lower global DNA methylation in their intestinal epithelial cells compared to germ-free mice, demonstrating the microbiota's role in shaping the host epigenome [11]. This is often mediated by microbial metabolites; for instance, SCFAs like butyrate and propionate can modulate the activity of enzymes like ten-eleven translocation (TET) proteins, which are involved in DNA demethylation [11]. Similarly, histone modifications—such as acetylation, methylation, and lactylation—are dynamically regulated by microbial signals. Butyrate, a potent HDAC inhibitor, leads to the accumulation of acetylated histones, promoting an open chromatin state and increased expression of genes involved in immune tolerance and barrier function [11] [2].
The following diagram illustrates the core signaling pathways through which gut microbiota-derived metabolites influence the host epigenome.
Experimental Approaches for Investigating Microbiome-Epigenome Interactions
To engineer the host epigenome, one must first be able to rigorously measure its relationship with the microbiome. This requires integrated multi-omics approaches and sophisticated experimental models.
Multi-Omics Integration and Machine Learning
Linking specific microbial features to host epigenetic states is a central challenge. The most successful strategies involve profiling the host epigenome (e.g., using Illumina MethylationEPIC arrays) alongside deep microbial sequencing (16S rRNA and shotgun metagenomics) from the same individual [43] [65]. For instance, a landmark epigenome-wide association study (EWAS) in Dutch cohorts identified and replicated specific CpG sites in blood (e.g., cg16586104 near RWDD3 and cg12234533 in ULK4) whose methylation levels were significantly associated with the abundance of the gut bacterium Eggerthella [65]. These observational findings in human cohorts provide critical starting points for experimental validation.
The power of this approach is greatly enhanced by machine learning. A study on pediatric ulcerative colitis (UC) demonstrated that combining mucosal microbiome data with host epigenomic and transcriptomic data in a multi-omics ML model significantly outperformed models using any single data type in predicting future disease relapse [43]. This integrative workflow is depicted below.
Table 2: Key Multi-Omics Data Types and Analytical Tools for Epigenetic Engineering Research
| Data Type | Common Assay/Method | Key Information Output | Relevant Analysis Tools |
|---|---|---|---|
| Host Epigenome | Illumina Infinium MethylationEPIC Array; Whole-genome bisulfite sequencing (WGBS) | Genome-wide DNA methylation levels at CpG sites | R packages: minfi, missMethyl; EWAS analysis pipelines |
| Gut Microbiome | 16S rRNA gene sequencing; Shotgun metagenomics | Microbial taxonomy; functional pathway abundance | QIIME 2, MOTHUR; HUMAnN2, MetaPhlAn |
| Host Transcriptome | RNA Sequencing (RNA-Seq) | Global host gene expression | STAR, HISAT2 for alignment; DESeq2, edgeR for differential expression |
| Data Integration & Modeling | - | Combined models predicting outcome from multi-omics data | Random Forest; Support Vector Machines (SVM); Custom ML scripts in R/Python |
Functional Validation in Model Systems
Observational associations must be tested for causality and mechanism using experimental models. A powerful approach is to use gnotobiotic (germ-free) mice colonized with defined microbial communities, combined with targeted epigenetic manipulations in the host.
Sample Experimental Protocol: Validating a Pro-Inflammatory Bacterium's Effect
- Bacterial Selection: Based on human multi-omics data, select a candidate bacterium linked to disease and epigenetic change (e.g., Veillonella parvula, which is enriched in relapsing pediatric UC [43]).
- In Vitro Co-culture: Culture the bacterium and prepare its conditioned media. Apply this to human intestinal epithelial cell lines (e.g., Caco-2, HT-29).
- Epigenetic & Transcriptomic Analysis: Post-exposure, profile host cells using:
- Chromatin Immunoprecipitation Sequencing (ChIP-seq): For histone modifications (e.g., H3K27ac) at promoter/enhancer regions of inflammatory genes.
- RNA-seq: To measure corresponding changes in gene expression (e.g., upregulation of IFN-γ signaling pathways [43]).
- In Vivo Validation: Orally gavage the bacterium (e.g., V. parvula) into susceptible mouse models (e.g., IL10−/− mice, which develop colitis). Analyze colonic tissue for expected epigenetic changes, inflammatory markers, and disease severity compared to controls [43].
The Scientist's Toolkit: Reagents and Research Solutions
This section details essential reagents, models, and tools for conducting research in epigenetic engineering of the host-microbiome axis.
Table 3: Research Reagent Solutions for Host-Microbiome Epigenetic Studies
| Category / Item | Function / Purpose | Example Application |
|---|---|---|
| Epigenetic Modifying Compounds | ||
| HDAC Inhibitors (e.g., Sodium Butyrate) | Induces histone hyperacetylation, promoting open chromatin | Testing the effect of increased acetylation on host antimicrobial peptide expression and subsequent microbiome shifts [11] [64]. |
| DNMT Inhibitors (e.g., 5-Azacytidine) | Causes DNA hypomethylation, potentially activating silenced genes | Investigating how reduced methylation in intestinal stem cells alters the niche for specific bacteria. |
| Biological Models | ||
| Germ-Free (GF) Mice | Provide a microbe-free host for colonization with defined communities | Establishing causal links between specific bacteria (or communities) and host epigenetic reprogramming [11]. |
| Gnotobiotic Mice | GF mice colonized with a known set of microorganisms | Studying interactions between a simplified microbiome and host epigenome in a controlled setting. |
| Organoid Cultures (e.g., Intestinal Organoids) | 3D in vitro models derived from stem cells that mimic the intestinal epithelium | High-throughput screening of microbial metabolites on host epithelial epigenetics without animal use. |
| Molecular Biology Assays | ||
| Illumina Infinium MethylationEPIC Kit | Profiles >850,000 CpG sites for genome-wide DNA methylation analysis | EWAS discovery in human cohorts or mouse models to link microbiome to host methylome [65]. |
| ChIP-seq Grade Antibodies | Target specific histone modifications (e.g., H3K27ac, H3K4me3) for chromatin immunoprecipitation | Mapping changes in histone marks in intestinal epithelial cells after probiotic or pathogenic bacterial exposure. |
| Microbiome Interventions | ||
| Probiotics (e.g., Lactobacillus, Bifidobacterium strains) | Live beneficial bacteria used to modulate the community | Assessing whether probiotic administration can reverse disease-associated epigenetic marks [11] [64]. |
| Fecal Microbiota Transplantation (FMT) | Transfer of entire microbial community from a donor to a recipient | Determining if a "healthy" microbiome can overwrite a "diseased" host epigenetic state in a recipient. |
Epigenetic engineering represents a frontier in manipulating host-microbiome interactions for therapeutic benefit. The evidence is clear: the gut microbiota continuously shapes the host epigenome, and this relationship is malleable. The future of this field lies in moving from association to causal engineering—using dietary interventions, prebiotics, probiotics, and potentially next-generation drugs like epigenetic editors to deliberately sculpt a host epigenetic landscape that fosters a resilient, health-promoting microbiome. This approach offers a promising strategy for managing complex diseases like IBD, CRC, and metabolic disorders, where both dysbiosis and epigenetic dysregulation are hallmarks. As high-throughput multi-omics, single-cell technologies, and machine learning continue to advance, the precision with which we can perform this epigenetic engineering will only increase, opening new avenues for personalized medicine and microbiome-based therapeutics.
Navigating Complexities: Standardization, Dysbiosis, and Intervention Challenges
Addressing Methodological Heterogeneity in Microbiome Research
The investigation into the impact of the gut microbiome on the host epigenome represents a frontier in molecular biology with profound implications for understanding disease etiology and developing novel therapeutics. However, this promising field is significantly challenged by methodological heterogeneity—inconsistencies in experimental and analytical approaches across studies that compromise the reproducibility, reliability, and translational potential of research findings. Microbiome data are inherently complex, characterized by high dimensionality, compositionality, and significant sparsity (frequent zero values) [66]. When compounded with variability in laboratory protocols, sequencing technologies, and computational methods, these inherent challenges create substantial barriers to drawing consistent conclusions about microbiome-epigenome interactions.
The urgency for standardization is particularly acute in studies examining how microbial communities influence host epigenetic mechanisms such as DNA methylation and histone modifications [1] [67]. Discrepancies in methodology can obscure genuine biological signals, such as the role of short-chain fatty acids (SCFAs) and other microbial metabolites in modulating host epigenetic states [2]. This technical guide provides a comprehensive framework for identifying, managing, and minimizing methodological heterogeneity throughout the research pipeline, from study design through data analysis, with a specific focus on investigating the gut microbiome's impact on the host epigenome.
Methodological heterogeneity in microbiome research arises from multiple sources across the experimental workflow, each introducing specific biases that can affect downstream results and interpretations.
Pre-Analytical and Technical Variability
- Sample Collection and Storage: Differences in collection methods (e.g., stool collection kits, swabs), stabilization solutions, storage conditions (temperature, duration), and DNA extraction kits can significantly alter microbial community profiles. These factors directly impact the quality and quantity of genetic material available for both microbiome and subsequent epigenomic analyses [68].
- Sequencing Technology Selection: The choice between 16S ribosomal RNA (rRNA) gene sequencing and shotgun metagenomics represents a major source of heterogeneity. While 16S sequencing (targeting specific hypervariable regions like V1-V3 or V4) is cost-effective for taxonomic profiling, it offers limited taxonomic resolution and cannot directly assess functional potential. In contrast, shotgun metagenomics captures all genetic material, enabling reconstruction of whole genomes and functional pathways but at higher cost and computational burden [66] [68].
- Host-Specific Confounding Factors: In gut microbiome-host epigenome studies, failure to account for clinical covariates such as host diet, medications (especially antibiotics), age, genetics, and comorbid metabolic conditions (e.g., obesity, type 2 diabetes) can lead to spurious associations. For instance, microbial signatures attributed to a disease state may actually reflect an unaccounted-for comorbidity [69].
Analytical and Computational Variability
- Data Processing Pipelines: The use of different bioinformatic tools for tasks such as quality filtering, OTU clustering, or amplicon sequence variant (ASV) calling (e.g., Mothur, QIIME, DADA2) introduces substantial variation in the resulting microbial community profiles [66] [68].
- Data Transformation Choices: The application of different data transformations—such as Total Sum Scaling (TSS), Centered Log-Ratio (CLR), or presence-absence (PA)—can significantly influence feature selection in machine learning models, even when classification accuracy remains comparable [70]. This is particularly critical when identifying microbial biomarkers potentially linked to host epigenetic changes.
- Statistical Methods for Differential Abundance: The selection of statistical models (e.g., edgeR, DESeq2, ANCOM, corncob) with different underlying assumptions about data distribution (e.g., accounting for zero-inflation, overdispersion, or compositionality) can yield divergent results regarding which taxa are significantly associated with host phenotypes or epigenetic markers [66].
Table 1: Impact of Data Transformation on Machine Learning Feature Selection
| Transformation Method | Key Characteristics | Impact on Feature Selection | Suitability for Epigenome Integration |
|---|---|---|---|
| Total Sum Scaling (TSS) | Converts to relative abundance; preserves compositionality | High variability in important features; sensitive to sparsity | Moderate; requires careful interpretation with epigenetic data |
| Centered Log-Ratio (CLR) | Log-transformed relative abundance; addresses compositionality | More stable than TSS; but performance varies | High; handles compositional nature of both microbiome and epigenomic data |
| Presence-Absence (PA) | Ignores abundance; focuses on occurrence | Surprisingly robust; consistent feature sets | Useful for initial screening of microbes associated with epigenetic marks |
| Arcsine Square Root (aSIN) | Variance-stabilizing transformation | Intermediate performance | Moderate; can be applied to proportional DNA methylation data |
Standardization Frameworks and Reporting Guidelines
Addressing methodological heterogeneity requires the implementation of standardized frameworks throughout the research lifecycle. Several international initiatives have established guidelines to enhance reproducibility and comparability across microbiome studies.
Quality Control and Benchmarking Initiatives
- Human Microbiome Action Project: This initiative works to establish standardized protocols for sample collection, processing, and analysis, facilitating cross-study comparisons and meta-analyses [71].
- Microbiome Quality Control (MBQC) Project: The MBQC baseline provides a framework for monitoring and improving measurement reproducibility across laboratories through inter-laboratory studies and reference materials [71].
- International Human Microbiome Standards (IHMS) Project: IHMS develops standard operating procedures (SOPs) for various aspects of microbiome analysis, from sample collection to data generation [71].
Study Design and Reporting Guidelines
- Strengthening the Organization and Reporting of Microbiome Studies (STORMS) Checklist: This tool provides a structured framework for reporting key methodological details in microbiome studies, ensuring transparent communication of methods and facilitating appropriate interpretation of results [71].
- FAIR and CARE Principles: Adherence to FAIR principles (Findable, Accessible, Interoperable, Reusable) ensures data is managed for maximum utility, while CARE principles (Collective Benefit, Authority to Control, Responsibility, Ethics) address indigenous data sovereignty, which is particularly relevant when working with human genomic and epigenomic data [1].
Experimental Design Considerations for Microbiome-Epigenome Studies
Robust experimental design is paramount for generating reliable data in studies investigating microbiome-epigenome interactions. The following considerations are specifically tailored to this research context.
Longitudinal Sampling and Multi-Omics Integration
- Longitudinal Study Designs: Cross-sectional snapshots of microbial communities provide limited insight into the dynamic interactions between microbes and host epigenetic states. Longitudinal sampling captures temporal dynamics of both microbial communities and epigenetic modifications, enabling causal inference and identification of stable versus transient associations [72] [69].
- Multi-Omics Integration: A comprehensive understanding of microbiome-epigenome interactions requires integration of multiple data types. Metagenomics (microbial taxonomy and genes), metatranscriptomics (microbial gene expression), metabolomics (microbial and host metabolites), and epigenomics (host DNA methylation, histone modifications) should be strategically combined to elucidate mechanistic pathways [69] [68].
Appropriate Sample Size and Power Considerations
- Cohort Sizing: Underpowered studies are a major source of irreproducible findings. Power calculations for microbiome-epigenome studies should account for effect sizes (microbial abundance shifts, epigenetic change magnitude), multiple testing burden (thousands of microbial taxa and epigenetic loci), and expected technical variability [69].
- Batch Effects Control: Technical artifacts introduced during sample processing can confound biological signals. Randomization of sample processing order, balancing experimental groups across sequencing runs, and statistical methods such as ComBat or Remove Unwanted Variation (RUV) are essential for mitigating batch effects [66].
Diagram 1: Integrated Workflow for Robust Microbiome-Epigenome Research
Computational Methods for Data Integration and Analysis
Advanced computational approaches are essential for extracting meaningful biological insights from complex microbiome-epigenome datasets while accounting for methodological heterogeneity.
Dimensionality Reduction and Tensor Factorization
- EMBED (Essential MicroBiomE Dynamics): This probabilistic nonlinear tensor factorization approach identifies Ecological Normal Modes (ECNs)—orthogonal modes capturing collective behavior of microbial communities over time. EMBED is particularly valuable for longitudinal microbiome-epigenome studies as it decomposes complex temporal dynamics into interpretable components, potentially revealing how microbial community shifts correlate with changes in host epigenetic patterns [72].
- Compositional Data Analysis: Microbiome data are inherently compositional (relative abundances), making standard statistical methods inappropriate. Log-ratio transformations (CLR, ALR, ILR) properly handle compositionality, with CLR being particularly useful for analyzing microbiome-epigenome correlations as it preserves Euclidean distances between samples [66] [70].
Machine Learning and Feature Selection Stability
- Transformation-Robust Algorithms: When applying machine learning to classify host states based on microbiome data (e.g., linking microbial profiles to epigenetic phenotypes), random forest and extreme gradient boosting show more consistent performance across different data transformations compared to elastic net regression [70].
- Conservative Feature Selection: Given that important microbial features vary significantly depending on data transformation, robust biomarker discovery for microbiome-epigenome associations should employ multiple transformation approaches and focus on features consistently identified across methods [70].
Table 2: Statistical Methods for Differential Abundance Analysis
| Method | Underlying Model | Handles Compositionality | Addresses Zero-Inflation | Suitable for Epigenome Integration |
|---|---|---|---|---|
| ANCOM | Log-ratio based | Yes | Partial | High; directly addresses compositionality |
| DESeq2 | Negative binomial | No (requires careful interpretation) | Yes | Moderate; can be applied to methylation count data |
| edgeR | Negative binomial | No (requires careful interpretation) | Yes | Moderate; can be applied to methylation count data |
| corncob | Beta-binomial | Yes | Yes | High; flexible model for relative abundances |
| ZIGDM | Zero-inflated generalized Dirichlet-multinomial | Yes | Yes | High; accounts for multiple data characteristics |
Experimental Protocols for Microbiome-Epigenome Mechanistic Studies
Beyond computational approaches, well-designed experimental protocols are essential for establishing causal mechanisms in microbiome-epigenome interactions.
Protocol 1: Assessing Microbial Metabolite Impact on Host DNA Methylation
Objective: To evaluate the effect of specific microbial metabolites on genome-wide DNA methylation patterns in host cells.
Materials:
- Primary human intestinal epithelial cells or appropriate cell line models
- Bacterial cultures of interest or purified microbial metabolites (SCFAs, polyamines)
- DNA extraction kit validated for methylation analysis
- Whole-genome bisulfite sequencing (WGBS) or Illumina EPIC array platform
- LC-MS/MS equipment for metabolite quantification
Procedure:
- Culture intestinal epithelial cells under standardized conditions
- Treat cells with physiological concentrations of microbial metabolites (e.g., butyrate, acetate, propionate) or vehicle control
- Harvest cells at multiple time points (e.g., 24h, 48h, 72h) to capture temporal dynamics
- Extract genomic DNA using methods that preserve methylation patterns
- Perform DNA methylation analysis using WGBS or targeted approaches
- Integrate methylation data with metabolite concentrations and functional assays (e.g., barrier function, inflammation)
Analysis: Identify differentially methylated regions (DMRs) associated with metabolite treatment; integrate with transcriptomic data to identify methylation-regulated genes; validate findings using CRISPR-based epigenetic editing approaches [1] [2].
Protocol 2: Gnotobiotic Mouse Model for Causal Microbiome-Epigenome Interactions
Objective: To establish causal relationships between specific microbial communities and host epigenetic modifications in vivo.
Materials:
- Germ-free mice of appropriate strain and age
- Defined microbial communities (isolates or defined consortia)
- Tissue collection and preservation reagents for both microbiome and epigenomic analyses
- Cross-fostering equipment for vertical transmission studies
- Multi-omics platforms for parallel microbiome and epigenome profiling
Procedure:
- Colonize germ-free mice with defined microbial communities (human isolates or simplified consortia)
- Maintain control groups with different microbial compositions or germ-free status
- Collect intestinal tissue, liver, and possibly other metabolic tissues at predetermined endpoints
- Process samples for parallel analyses:
- Microbiome: 16S rRNA gene sequencing or shotgun metagenomics of luminal and mucosal communities
- Epigenome: DNA methylation (WGBS/RRBS), histone modifications (ChIP-seq), or chromatin accessibility (ATAC-seq) from relevant host tissues
- Transcriptome: RNA-seq to link epigenetic changes to gene expression
- Analyze data using integrative computational approaches (e.g., sparse canonical correlation analysis) to identify microbiome-epigenome associations
Analysis: Identify host epigenetic changes specific to microbial colonization; correlate specific microbial taxa or functions with epigenetic markers; validate findings using microbial metabolite supplementation or targeted microbial manipulations [1] [67].
Research Reagent Solutions for Standardized Microbiome-Epigenome Studies
Table 3: Essential Research Reagents and Resources
| Reagent/Resource | Specific Examples | Application in Microbiome-Epigenome Research |
|---|---|---|
| DNA Extraction Kits | MoBio PowerSoil Kit, QIAamp DNA Stool Mini Kit | Standardized microbial DNA extraction for sequencing; special care for DNA methylation preservation from host tissues |
| 16S rRNA Primers | 515F/806R targeting V4 region, 27F/338R | Targeted amplification of bacterial communities; selection of hypervariable region affects taxonomic resolution |
| Reference Databases | GreenGenes, SILVA, RDP, Human Methylation EPIC array | Taxonomic classification of sequences; annotation of host epigenetic marks |
| Bioinformatic Tools | QIIME2, Mothur, DADA2 for microbiome; Bismark, MethylKit for epigenomics | Processing sequencing data; ensuring compatibility between microbiome and epigenome analytical pipelines |
| Standards and Controls | Mock microbial communities, Methylated DNA standards, Internal standards for metabolomics | Quality control across batches; distinguishing technical variation from biological signals |
| Cell Culture Models | Caco-2, HT-29, organoids, primary intestinal epithelial cells | In vitro investigation of microbiome-epigenome interactions; testing microbial metabolites |
| Animal Models | Germ-free mice, gnotobiotic models, humanized microbiota mice | Establishing causality in microbiome-epigenome interactions in vivo |
Diagram 2: Microbiome-Epigenome Signaling Pathways and Interactions
Addressing methodological heterogeneity is not merely a technical exercise but a fundamental requirement for advancing our understanding of how the gut microbiome influences the host epigenome. As research in this field progresses toward clinical translation—including microbiome-based diagnostics, targeted therapies, and personalized interventions—standardization becomes increasingly critical. The frameworks, methods, and protocols outlined in this technical guide provide a roadmap for generating robust, reproducible data that can reliably inform mechanisms and therapeutic opportunities. Through concerted efforts to harmonize methodologies, validate findings across diverse populations, and transparently report methodological details, the research community can overcome the challenge of heterogeneity and fully realize the potential of microbiome-epigenome research to transform human health.
The human gut microbiome, a complex ecosystem of bacteria, viruses, fungi, and other microorganisms, exerts a profound influence on host physiology and disease susceptibility. Dysbiosis, defined as an imbalance in the microbial community structure and function, is increasingly recognized as a key environmental driver of epigenetic reprogramming. The host epigenome—comprising DNA methylation, histone modifications, and non-coding RNAs—represents a critical interface through which gut microbiota and their metabolites regulate gene expression without altering the underlying DNA sequence [11] [2]. This review examines the mechanistic pathways by which microbial dysbiosis induces epigenetic alterations, explores the functional consequences for host health, and details experimental approaches for investigating this dynamic crosstalk within the context of a broader thesis on the impact of the gut microbiome on host epigenome research.
The clinical significance of understanding microbiota-epigenome interactions is substantial. Disruption of these pathways is implicated in the pathogenesis of diverse conditions including inflammatory bowel disease (IBD), colorectal cancer (CRC), cardiovascular diseases, metabolic disorders, and neuropsychiatric conditions [73] [11] [74]. For researchers and drug development professionals, targeting the dysbiosis-epigenetics axis presents promising opportunities for novel therapeutic strategies and biomarker discovery.
Mechanisms of Microbiota-Mediated Epigenetic Modifications
Microbial Metabolites as Epigenetic Regulators
Gut microbiota produce a diverse array of metabolites that serve as substrates, cofactors, and enzymatic regulators of host epigenetic machinery. The table below summarizes key microbiota-derived metabolites and their epigenetic functions.
Table 1: Key Microbiota-Derived Metabolites and Their Epigenetic Mechanisms
| Metabolite | Producing Bacteria | Epigenetic Mechanism | Biological Effect |
|---|---|---|---|
| Butyrate | Faecalibacterium prausnitzii, Roseburia | HDAC inhibition; HAT activation [73] [75] | Histone hyperacetylation; anti-inflammatory; Treg differentiation [73] [75] |
| Propionate | Bacteroidetes, Roseburia | HDAC inhibition; histone propionylation [75] | Anti-inflammatory; regulation of fatty acid oxidation genes [75] |
| Acetate | Bacteroidetes, Bifidobacteria | HDAC inhibition; histone acetylation via ACSS1/2 [75] | Lipogenic gene activation; leptin regulation [75] |
| Folate | Bifidobacterium, Lactobacillus | Methyl donor for SAM synthesis [73] [11] | DNA methylation; 6-methyltetrahydrofolate synthesis [73] |
| Trimethylamine (TMA) | Proteobacteria | Alters DNMT expression [75] | DNA methylation changes; pro-atherogenic [73] [75] |
| Choline | Metabolized by various taxa | Methyl donor precursor [73] | SAM synthesis; DNA and histone methylation [73] |
Short-chain fatty acids (SCFAs), including butyrate, propionate, and acetate, are among the most extensively studied microbiota-derived epigenetic regulators. These metabolites are produced through anaerobic fermentation of dietary fiber and exert potent effects on chromatin structure. Butyrate functions as a potent histone deacetylase (HDAC) inhibitor, leading to increased histone acetylation and enhanced gene transcription [73] [75]. This mechanism underlies butyrate's anti-inflammatory properties through repression of NF-κB and interferon γ production, while enhancing peroxisome proliferator-activated receptor γ (PPARγ) expression [73]. Propionate induces histone lysine propionylation (Kpr), particularly at H3K14, which is enriched at promoters of highly transcribed genes involved in fatty acid oxidation [75]. Acetate contributes to histone acetylation by serving as a substrate for acetyl-CoA synthetases (ACSS1 and ACSS2), activating lipogenic genes through increased H3K9, H3K27, and H3K56 acetylation at their promoters [75].
Beyond SCFAs, microbial metabolism influences one-carbon metabolism and methyl donor availability. Gut microbes metabolize choline and L-carnitine into trimethylamine (TMA), which is subsequently oxidized in the liver to trimethylamine-N-oxide (TMAO), a pro-atherogenic metabolite [73] [75]. TMA exposure alters DNMT expression profiles, upregulating DNMT1 while suppressing DNMT3A, thereby influencing DNA methylation patterns [75]. Conversely, folate produced by Bifidobacterium and Lactobacillus species serves as a critical methyl donor for S-adenosylmethionine (SAM) synthesis, the primary methyl donor for DNA and histone methylation reactions [73] [11].
Molecular Pathways of Epigenetic Regulation
Diagram: Microbial Metabolite Regulation of Host Epigenetics
Microbial Metabolite Regulation of Host Epigenetics
Gut microbiota regulate host epigenetic programs through several interconnected molecular pathways. DNA methylation is catalyzed by DNA methyltransferases (DNMTs) that transfer methyl groups to cytosine bases in CpG dinucleotides, typically resulting in transcriptional repression [11] [75]. Microbial metabolites influence this process by modulating DNMT expression and activity, as well as by affecting the availability of SAM, the universal methyl donor [73] [11]. Conventionally raised mice display significantly diminished global methylation levels in intestinal epithelial cells compared to germ-free mice, demonstrating the profound impact of microbial colonization on the host methylome [11].
Histone modifications represent another major epigenetic mechanism influenced by gut microbiota. These post-translational modifications—including acetylation, methylation, lactylation, and crotonylation—alter chromatin structure and accessibility [11] [2]. The balance between histone acetyltransferases (HATs) and deacetylases (HDACs), as well as histone methyltransferases and demethylases, determines the histone modification landscape. SCFAs directly inhibit HDAC activity, leading to histone hyperacetylation and increased gene transcription [73] [75]. Butyrate-mediated HDAC inhibition promotes histone H3 hyperacetylation, driving anti-inflammatory transcriptional programs in immune cells and arresting proliferation in vascular smooth muscle cells through upregulation of cdk inhibitors p15INK4b and p21Cip1 [75].
Non-coding RNAs, including microRNAs (miRNAs) and long non-coding RNAs (lncRNAs), constitute a third mechanism of microbiota-epigenome crosstalk. Approximately 150-200 miRNAs are associated with cardiovascular diseases, and their expression can be influenced by gut microbiota [73]. The microbiota-miR-181 axis plays a key role in developing insulin resistance and obesity, while miRNAs in human and mouse feces may serve as indicators of intestinal malignancies [73]. LncRNAs, which exceed 200 nucleotides in length, regulate diverse cellular processes including metabolism, differentiation, and epigenetic regulation, with tissue-specific expression patterns [73] [11].
Disease-Specific Epigenetic Consequences of Dysbiosis
Inflammatory Bowel Disease and Colorectal Cancer
In inflammatory bowel disease (IBD), dysbiosis characterized by reduced microbial diversity, decreased SCFA-producing obligate anaerobes, and increased facultative anaerobes (e.g., E. coli) drives epigenetic alterations that perpetuate inflammation [73] [11]. Patients with IBD exhibit specific DNA methylation patterns in genes including Vmp1, Itgb2, and Txk, which may serve as diagnostic biomarkers and therapeutic targets [11]. The reduction in butyrate-producing bacteria such as Faecalibacterium prausnitzii and Roseburia diminishes HDAC inhibition, leading to enhanced NF-κB signaling and pro-inflammatory gene expression [73] [11].
In colorectal cancer (CRC), dysbiosis promotes tumorigenesis through multiple epigenetic mechanisms. Butyrate, which normally functions as an HDAC inhibitor and suppresses proliferation, can paradoxically enhance tumor growth in certain cellular contexts [73]. Dysbiosis also influences miRNA expression profiles, with specific miRNAs in feces potentially serving as non-invasive biomarkers for early detection of intestinal malignancies [73]. Microbial activation of immune pathways through epigenetic dysregulation creates a pro-tumorigenic microenvironment that supports CRC progression [11].
Cardiovascular and Metabolic Diseases
In atherosclerosis, gut microbiota contribute to disease pathogenesis through metabolite-mediated epigenetic mechanisms. The TMAO pathway is particularly significant, with choline and L-carnitine metabolism by gut microbes generating TMA, which is converted to TMAO in the liver [73] [75]. TMAO promotes atherosclerosis through multiple mechanisms including altered cholesterol metabolism, enhanced foam cell formation, and platelet hyperreactivity [73]. Epigenetically, TMA exposure alters DNMT expression profiles, potentially leading to pro-atherogenic methylation patterns [75].
Table 2: Epigenetic Mechanisms in Microbiota-Linked Diseases
| Disease | Dysbiosis Features | Key Epigenetic Alterations | Functional Consequences |
|---|---|---|---|
| IBD | Reduced diversity; ↓SCFA producers; ↑E. coli [73] [11] | DNA methylation changes in Vmp1, Itgb2, Txk [11] | Enhanced inflammation; impaired barrier function [11] |
| CRC | Altered diversity; specific pathogen enrichment [11] | miRNA expression changes; HDAC modulation [73] [11] | Increased proliferation; reduced apoptosis [73] [11] |
| Atherosclerosis | ↑TMA-producing bacteria [73] [75] | DNMT expression changes; histone modifications [75] | Endothelial dysfunction; inflammation [73] [75] |
| Obesity/Diabetes | ↓Faecalibacterium; ↑Firmicutes/Bacteroidetes ratio [73] [76] | miR-181 dysregulation; leptin promoter methylation [73] [76] | Insulin resistance; metabolic dysfunction [73] [76] |
| Anorexia Nervosa | ↑Mucin-degraders; ↓butyrate-producers [22] | Appetite/metabolic gene methylation [22] | Altered weight regulation; persistent hypometabolism [22] |
Metabolic diseases including obesity, type 2 diabetes, and non-alcoholic fatty liver disease (NAFLD) demonstrate strong connections between dysbiosis and epigenetic dysregulation. Gut microbiota influence host metabolism through the microbiota-miR-181 axis, which plays a key role in developing insulin resistance and obesity [73]. In high-fat diet models, SCFAs suppress obesity-related leptin overexpression through downregulation of DNMT1/3a/3b, reducing leptin promoter methylation [75]. Reduced abundance of Faecalibacterium prausnitzii, a key butyrate producer, in type 2 diabetes patients correlates with hypermethylation of free fatty acid receptor promoter CpG sites [75]. These epigenetic modifications contribute to metabolic dysfunction and represent potential therapeutic targets.
Neuropsychiatric Disorders
The microbiota-gut-brain axis provides a pathway through which dysbiosis can influence neuropsychiatric conditions via epigenetic mechanisms. In anorexia nervosa (AN), dysbiosis characterized by decreased butyrate-producing genera (Faecalibacterium, Roseburia) and increased mucin-degrading species (Akkermansia, Methanobrevibacter smithii) may contribute to persistent epigenetic alterations in genes regulating appetite, body weight, and mood [22]. These changes may underlie the chronicity and high relapse rates characteristic of AN. Similarly, in substance use disorders (SUDs), gut microbiome dysbiosis alters the production of microbial metabolites that affect brain function through epigenetic changes, modulating neuroimmunological activity and contributing to the development and persistence of addictive behaviors [74].
Experimental Approaches and Methodologies
Model Systems and Research Designs
Diagram: Experimental Workflow for Microbiota-Epigenetics Research
Experimental Workflow for Microbiota-Epigenetics Research
Investigating microbiota-epigenetics interactions requires carefully designed experimental approaches. Germ-free (GF) mouse models provide a foundational system for establishing causal relationships between microbial colonization and epigenetic changes. Conventionally raised (CNV) mice display significantly diminished global methylation levels in intestinal epithelial cells compared to GF mice, demonstrating the profound impact of microbial colonization on the host methylome [11]. Gnotobiotic models, in which mice are colonized with defined microbial communities, enable researchers to study the effects of specific bacterial taxa or communities on host epigenetic programming.
Fecal microbiota transplantation (FMT) studies represent another powerful experimental approach. Transplantation of fecal microbiota from patients with anorexia nervosa into germ-free mice reduces weight gain compared to transplantation from healthy controls, providing evidence for a causal role of the gut microbiome in disease pathology [22]. Similarly, FMT from healthy donors to recipients with metabolic syndrome improves metabolic parameters and is associated with epigenetic changes [73] [76].
Diversity-outbred mouse models have significantly advanced the study of complex disorders by providing unparalleled genetic and phenotypic diversity that better models human population variation [74]. These models enable researchers to examine how genetic background influences individual susceptibility to microbiota-mediated epigenetic changes in response to environmental factors such as diet, stress, or substance exposure.
Analytical Methods and Technologies
Advanced molecular techniques are essential for characterizing microbiota-epigenome interactions. High-throughput methylation mapping using methods such as whole-genome bisulfite sequencing enables comprehensive analysis of DNA methylation patterns in response to microbial manipulation [2]. Chromatin immunoprecipitation followed by sequencing (ChIP-seq) identifies histone modifications and transcription factor binding sites that are influenced by microbial metabolites [2] [75]. Single-cell multi-omics approaches provide unprecedented resolution to examine epigenetic heterogeneity within tissues and cell populations in response to microbial signals [2].
Metabolomic profiling using mass spectrometry-based methods quantifies microbiota-derived metabolites such as SCFAs, TMAO, and folate, enabling correlation with epigenetic marks [75]. Integration of these datasets through multi-omics integration frameworks and artificial intelligence approaches is accelerating our ability to model complex microbiota-epigenome interactions at high resolution [2].
Table 3: Essential Research Reagents and Experimental Tools
| Reagent/Tool | Category | Specific Examples | Research Application |
|---|---|---|---|
| Germ-Free Mice | Model System | Axenic C57BL/6J | Establish causality in microbiota-epigenetics interactions [11] |
| Gnotobiotic Models | Model System | Defined microbial consortium | Function of specific bacterial taxa [11] |
| HDAC Inhibitors | Chemical Tool | Sodium butyrate, Trichostatin A | Study histone acetylation mechanisms [73] [75] |
| DNMT Inhibitors | Chemical Tool | 5-aza-2'-deoxycytidine | Investigate DNA methylation-dependent pathways [73] |
| SCFA Reagents | Metabolite | Sodium butyrate, Sodium propionate | Epigenetic effects of microbial metabolites [73] [75] |
| FMT Protocols | Methodology | Donor screening, administration methods | Transfer microbial communities between hosts [73] [22] |
| DNA Methylation Kits | Reagent | Bisulfite conversion kits | Analyze genome-wide or gene-specific methylation [2] |
| ChIP-grade Antibodies | Reagent | Anti-acetyl-histone H3, Anti-H3K4me3 | Histone modification mapping [2] [75] |
The Scientist's Toolkit: Research Reagent Solutions
The investigation of dysbiosis and epigenetic dysregulation requires specialized research reagents and tools. Germ-free and gnotobiotic animal models are essential for establishing causal relationships between specific microorganisms and host epigenetic changes [11]. These controlled model systems enable researchers to manipulate microbial communities with precision and observe resulting epigenetic effects.
Chemical inhibitors and activators of epigenetic enzymes represent valuable tools for mechanistic studies. HDAC inhibitors such as sodium butyrate and trichostatin A allow researchers to mimic the effects of butyrate-producing bacteria [73] [75]. Similarly, DNMT inhibitors like 5-aza-2'-deoxycytidine enable investigation of DNA methylation-dependent pathways [73]. These pharmacological tools help establish causality between specific epigenetic modifications and functional outcomes.
Microbiota-derived metabolites, including purified SCFAs (sodium butyrate, sodium propionate) and TMAO, are critical reagents for studying direct epigenetic effects [73] [75]. When administered to cell cultures or animal models, these metabolites help elucidate molecular mechanisms linking microbial metabolism to host epigenetic reprogramming.
High-quality molecular biology reagents are essential for epigenetic mapping. Bisulfite conversion kits enable DNA methylation analysis, while ChIP-grade antibodies against specific histone modifications (e.g., acetyl-histone H3, H3K4me3) facilitate chromatin studies [2] [75]. Advanced sequencing kits and multi-omics platforms support comprehensive characterization of microbiota-epigenome interactions.
The intricate relationship between gut microbial dysbiosis and epigenetic dysregulation represents a paradigm shift in our understanding of how environmental factors, including microbiota, shape host physiology and disease susceptibility. The microbiota-epigenome axis functions as a key interface that translates microbial signals into stable changes in gene expression through DNA methylation, histone modifications, and non-coding RNA regulation. Understanding these mechanisms provides novel insights into disease pathogenesis and opens new avenues for therapeutic intervention.
Future research directions should focus on elucidating the specific bacterial strains and consortia that most significantly influence host epigenetic programming, developing tissue-specific epigenetic maps in response to microbial manipulation, and identifying critical periods of susceptibility to microbiota-mediated epigenetic changes across the lifespan. From a translational perspective, targeting the dysbiosis-epigenetics axis holds promise for novel therapeutic strategies including precision probiotics, metabolite-based therapeutics, and epigenetic drugs designed to counteract the effects of dysbiosis. As single-cell multi-omics technologies and artificial intelligence approaches continue to advance, our ability to decipher the complex language of microbiota-epigenome communication will accelerate, potentially enabling personalized approaches to prevent and treat a wide spectrum of diseases linked to dysbiosis and epigenetic dysregulation.
The emerging understanding of the gut microbiome-epigenome axis represents a paradigm shift in therapeutic development, introducing both novel mechanisms for intervention and significant technical challenges. The gut microbiota exerts a profound influence on host physiology through multiple pathways, including the production of metabolites that act as epigenetic modifiers, direct interactions with host cells, and complex ecological dynamics within the microbial community itself [77]. These interactions create a bidirectional communication network where host epigenetic states can influence microbial composition, and gut microbes in turn can modify the host epigenome [67]. This axis introduces three fundamental hurdles in therapeutic development: maintaining microbial community stability, achieving targeted delivery to specific microbial populations or host tissues, and personalizing interventions based on individual microbiome-epigenome profiles. This technical guide examines these interconnected challenges within the context of advancing therapeutics that target or leverage the gut microbiome-epigenome relationship, providing researchers with strategic frameworks and methodological approaches to overcome these barriers.
The clinical implications of this axis are substantial, as evidenced by studies showing that early-life gut microbiome establishment, significantly influenced by factors such as delivery mode, has long-term health consequences [78] [79]. For instance, the absence of specific taxa like Bacteroides in infants delivered by cesarean section has been linked to altered immune development and increased susceptibility to infections [79]. Simultaneously, epigenome-wide association studies (EWAS) have begun identifying specific CpG sites in host DNA whose methylation states are associated with particular bacterial abundances, providing mechanistic links between microbial colonization and host gene regulation [65]. These findings underscore the therapeutic potential of targeting this axis while highlighting the complex technical challenges that must be addressed to translate this knowledge into effective interventions.
Technical Hurdle 1: Stability of Microbial Communities and Epigenetic States
Microbial Community Dynamics and Colonization Resistance
A primary challenge in developing microbiome-based therapeutics lies in the inherent instability of microbial communities and the difficulty of establishing persistent therapeutic strains. Research has revealed that colonization stability is a more significant factor in infant gut microbiome composition than mere exposure to maternal microbiota during birth [78]. A compelling study demonstrated that 94% of infants born via cesarean section had detectable Bacteroides species in their first week of life, but these typically disappeared by the second week despite initial colonization [78] [80]. This phenomenon highlights the critical importance of ecological factors in maintaining microbial populations, suggesting that therapeutic interventions must address not only initial introduction but also long-term persistence of beneficial microbes.
The stability of microbial communities is governed by principles of microbial ecology, including competition for resources, niche specialization, and community resistance to perturbation [77]. In the case of cesarean-delivered infants, the disappearance of Bacteroides was correlated with increased abundance of Streptococcus and Haemophilus, with inverse abundance relationships observed between these taxa [80]. This competitive exclusion demonstrates that simply introducing a therapeutic strain is insufficient; the ecological context must support its persistence. Future research should focus on how to integrate therapeutic microbes into the established gut ecosystem, potentially through prebiotic support or staged introduction protocols that sequentially prepare the ecological niche.
Epigenetic Plasticity and Environmental Influence
Parallel to microbial community stability, the plasticity of epigenetic states presents both opportunities and challenges for therapeutic development. Epigenetic modifications, including DNA methylation and histone modifications, are dynamically regulated in response to environmental factors, including microbial metabolites [81] [82]. While this plasticity enables therapeutic intervention, it also introduces variability that complicates treatment standardization. The host epigenome serves as an interface between environmental exposures—including microbial colonization—and gene expression patterns, creating a record of historical exposures that can influence current physiological states [81].
Research has identified specific mechanistic links between gut microbes and host epigenetic modifications. Butyrate, a short-chain fatty acid produced by certain gut bacteria, functions as a histone deacetylase (HDAC) inhibitor, directly linking microbial metabolism to epigenetic regulation [77]. Additionally, a discovery and replication EWAS identified specific CpG sites (cg16586104 and cg12234533) whose methylation states were significantly associated with abundance of the genus Eggerthella, providing direct evidence of microbiome-epigenome interactions [65]. These findings demonstrate that the stability of epigenetic states is intimately connected to microbial community composition, creating a feedback loop that must be considered in therapeutic design.
Table 1: Key Microbial-Derived Metabolites with Epigenetic Regulatory Functions
| Metabolite | Microbial Source | Epigenetic Mechanism | Physiological Impact |
|---|---|---|---|
| Butyrate | Firmicutes species (e.g., Faecalibacterium prausnitzii) | HDAC inhibition | Immune modulation, energy source for colonocytes [77] |
| Folate | Bifidobacterium species, Lactobacillus species | Methyl donor for DNA methylation | DNA synthesis, methylation reactions [77] |
| Acetate | Multiple commensal species | Histone acetylation substrate | Energy metabolism, chromatin accessibility [77] |
Technical Hurdle 2: Targeted Delivery in Complex Biological Systems
Advanced Drug Delivery Systems for Microbiome-Targeted Therapies
Targeted delivery presents a formidable challenge in microbiome-epigenome therapeutics, requiring precise intervention in specific microbial populations, host tissues, or intracellular compartments. Recent advances in drug delivery systems (DDS) offer promising approaches to overcome these barriers. Modern DDS are formulated using advanced technology to enable systemic drug delivery to specific target sites, maximizing therapeutic efficacy while minimizing off-target accumulation [83]. These systems include lipid-based nanoparticles, polymer-drug conjugates, and cell membrane-camouflaged nanoparticles that improve bioavailability, target specificity, and controlled release kinetics.
For microbiome-targeted therapies, delivery systems must navigate the complex environment of the gastrointestinal tract, protecting therapeutic agents from degradation while ensuring release at the appropriate location. Red blood cell membrane-camouflaged nanoparticles represent an innovative approach that leverages natural cell membranes to evade immune detection and enhance circulation time [83]. Similarly, liposomal formulations have been successfully employed to deliver antibiotics like amikacin specifically to pulmonary macrophages for treating nontuberculous mycobacteria infections, demonstrating the potential for targeted antimicrobial therapy in complex biological niches [84]. These advanced delivery strategies could be adapted for microbiome-modulating agents that require precise spatial localization within the gastrointestinal tract.
Epigenetic Modifier Delivery and Cellular Targeting
The delivery of epigenetic therapeutics faces unique challenges related to nuclear access, locus specificity, and temporal control of epigenetic modifications. Current epigenetics-targeted drugs primarily inhibit broad-acting enzymes such as DNA methyltransferases (DNMTs) and histone deacetylases (HDACs) [82]. While these approaches have shown clinical success, particularly in oncology, their genome-wide effects limit specificity and potentially cause undesirable side effects. Next-generation epigenetic therapeutics aim for greater precision through locus-specific targeting, achieved by conjugating epigenetic modifier domains to DNA-binding molecules or using CRISPR-based systems for targeted epigenetic editing.
The development of targeted epigenetic therapies must also account for the influence of gut microbiome composition on drug metabolism and efficacy. Research has shown that gut microbes can mediate the effects of environmental factors, including medications, on host DNA methylation [65]. For example, selective serotonin reuptake inhibitor (SSRI) antidepressants were associated with altered abundance of Clostridium sensu stricto 1 and Peptostreptococcaceae, which in turn correlated with methylation changes at specific CpG sites [65]. This complex interplay suggests that personalized delivery approaches may be necessary to account for microbiome-mediated variations in drug response.
Table 2: Advanced Drug Delivery Systems with Application to Microbiome-Epigenome Therapeutics
| Delivery System | Key Features | Potential Applications | Current Status |
|---|---|---|---|
| Liposomal nanoparticles | Enhanced cellular uptake, improved pharmacokinetics | Delivery of antimicrobials, epigenetic modifiers [84] | FDA-approved for some applications |
| Cell membrane-camouflaged nanoparticles | Immune evasion, prolonged circulation | Targeted delivery to specific tissues or cell types [83] | Preclinical development |
| Polymer-drug conjugates | Controlled release, improved solubility | Delivery of microbial metabolites, epigenetic drugs [83] | Various stages of clinical trials |
| Nasal delivery systems | Bypasses blood-brain barrier, rapid onset | CNS-targeted delivery of epigenetic modifiers [84] | FDA-approved for esketamine |
Technical Hurdle 3: Personalization Based on Microbiome-Epigenome Profiles
Biomarker Discovery for Stratified Therapeutics
Personalized approaches to microbiome-epigenome therapeutics require robust biomarkers that can stratify patient populations based on their likely treatment response. Epigenome-wide association studies (EWAS) have begun identifying specific epigenetic markers associated with microbiome composition. For example, a large-scale EWAS discovered that methylation at CpG site cg16586104 (near the RWDD3 gene) was positively associated with Eggerthella abundance, while cg12234533 (within the ULK4 gene) showed a negative association [65]. These microbiome-associated epigenetic signatures offer potential biomarkers for personalizing therapeutic interventions based on an individual's microbiome-epigenome profile.
The personalization challenge extends beyond initial stratification to dynamic monitoring of treatment response. Both the gut microbiome and epigenome exhibit plasticity in response to therapeutic interventions, environmental exposures, and lifestyle factors [81] [65]. Research has demonstrated that environmental exposures, including diet and medication use, associate with both microbiome composition and host DNA methylation states [65]. For instance, coffee consumption was simultaneously associated with abundance of a Coriobacteriaceae genus and methylation at CpG site cg13058819, suggesting shared environmental influences on both systems [65]. These findings underscore the need for longitudinal monitoring approaches that can track dynamic changes in both microbiome and epigenome throughout therapeutic interventions.
Integration of Multi-Omics Data for Personalized Prediction
Advancements in multi-omics technologies enable increasingly sophisticated approaches to personalizing microbiome-epigenome therapeutics. The integration of genomic, epigenomic, transcriptomic, and metabolomic data with deep microbiome sequencing provides a comprehensive view of the complex interactions between host physiology and microbial communities. This data-rich environment facilitates the development of mechanistic models that can predict individual responses to therapeutic interventions. For the human gut, genome-scale metabolic models have been developed, with comprehensive databases created in relation to nutrition and disease [77]. These models continue to increase in sophistication, incorporating spatial and temporal dimensions of host-microbiome interactions.
The application of artificial intelligence and machine learning to multi-omics data represents a promising approach for personalizing therapeutic strategies. These computational methods can identify complex, non-linear relationships between microbial features, epigenetic markers, and clinical outcomes that may not be apparent through conventional statistical approaches. Furthermore, the development of host-microbe hologenome models that treat the host and its microbiome as a single biological unit provides a theoretical framework for personalized interventions that simultaneously target host pathways and microbial functions [77] [67]. As these models become more refined, they will enable truly personalized therapeutic approaches based on an individual's unique microbiome-epigenome profile.
Experimental Approaches and Methodologies
Standardized Protocols for Microbiome-Epigenome Studies
Robust experimental methodologies are essential for advancing our understanding of microbiome-epigenome interactions and developing effective therapeutics. Standardization of quality control measures is particularly critical in microbiome studies, as variations in sample collection, DNA extraction, and sequencing protocols can introduce significant technical artifacts [77]. Recommended practices include using stool collection kits with fixation buffers that prevent microbial growth during handling, implementing rigorous QC protocols for DNA/RNA extraction to ensure consistent recovery rates, and repeatedly sequencing reference stool samples across sequencing batches to monitor and correct for batch effects [77].
For epigenomic analyses, consideration of tissue and cell specificity is essential, as epigenetic patterns vary dramatically across different cell types [81]. While blood is commonly used for EWAS due to its accessibility, its relevance to tissue-specific processes in the gut or brain may be limited. Emerging approaches use cell-free DNA or specialized sampling techniques to assess epigenetic states in specific tissues. Additionally, temporal dynamics must be considered in study design, as both microbiome composition and epigenetic states change over time in response to development, environmental exposures, and therapeutic interventions [81] [65].
Diagram 1: Microbiome-Epigenome Signaling Axis. This diagram illustrates the bidirectional relationship between gut microbiota and host epigenome, highlighting how microbial metabolites serve as signaling molecules that modify host epigenetic states, ultimately influencing gene expression and health outcomes.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Microbiome-Epigenome Studies
| Tool Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Microbiome Profiling | 16S rRNA sequencing (V4 region), Shotgun metagenomics | Taxonomic classification, functional potential assessment | For 16S: Primer selection determines taxonomic resolution; for shotgun: higher cost but species-level resolution [79] [65] |
| Epigenomic Analysis | Illumina MethylationEPIC array, Whole-genome bisulfite sequencing | Genome-wide DNA methylation profiling | Array provides coverage of ~850,000 CpGs; sequencing offers base resolution but higher cost [65] |
| Metabolite Analysis | Mass spectrometry, NMR spectroscopy | Quantification of microbial metabolites (SCFAs, etc.) | Requires different extraction protocols for various metabolite classes [77] |
| Germ-Free Models | Germ-free mice, Gnotobiotic systems | Establish causal relationships in host-microbe interactions | Technically challenging, allows introduction of defined microbial communities [77] |
| Computational Tools | QIIME 2, METAGENassist, MEBS | Microbiome data analysis, multi-omics integration | Various tools for different analysis steps: quality control, taxonomy assignment, statistical analysis [77] [65] |
Experimental Workflow for Microbiome-Epigenome Interaction Studies
Diagram 2: Integrated Workflow for Microbiome-Epigenome Studies. This experimental workflow outlines the parallel processing of microbiome and epigenome samples, culminating in integrated statistical analysis to identify significant associations between microbial features and epigenetic markers.
The development of therapeutics targeting the gut microbiome-epigenome axis represents a frontier in precision medicine, offering potential novel interventions for a wide range of conditions. However, significant technical hurdles related to stability, delivery, and personalization must be overcome to realize this potential. Addressing these challenges requires interdisciplinary approaches that integrate microbiology, epigenetics, pharmaceutical sciences, and computational biology. The continued refinement of experimental models, including gnotobiotic systems and organ-on-a-chip technologies, will enhance our ability to study microbiome-epigenome interactions in controlled environments. Simultaneously, advances in targeted delivery systems, such as nanoparticle-based platforms and engineered microbial therapeutics, will improve our capacity to intervene precisely in this complex biological system.
Looking forward, the field must prioritize the development of standardized protocols that enable comparison and integration of datasets across studies [77]. Furthermore, the implementation of longitudinal study designs that capture the dynamic nature of both microbiome and epigenome will be essential for understanding the temporal aspects of their interaction. Finally, the translation of basic research findings into clinical applications will require close collaboration between academic researchers, pharmaceutical developers, and clinical practitioners. As these efforts converge, we anticipate a new generation of therapeutics that leverage the profound interconnectedness of our microbial inhabitants and our epigenetic regulation to promote health and treat disease.
In the rapidly advancing field of gut microbiome-host epigenome research, a primary challenge is the accurate isolation of specific biological interactions from the complex background of influential host factors. Diet, age, and pre-existing co-morbidities represent three significant confounding variables that can dramatically alter research outcomes, potentially leading to spurious associations or obscuring genuine biological signals. These factors independently and synergistically modify both microbial community structures and host epigenetic marks, creating a layered complexity that researchers must navigate to produce valid, reproducible findings. This technical guide examines the mechanistic pathways through which these confounders operate, provides quantitative data on their effect sizes, outlines robust methodological approaches for their control, and offers visualization of the complex relationships within this research landscape. A precise understanding of these confounders is paramount for researchers and drug development professionals aiming to develop targeted therapeutic interventions that modulate the gut microbiome for epigenetic benefits.
The Gut Microbiome-Epigenome Axis: A Primer
The bidirectional communication between gut microbiota and the host epigenome represents a critical interface where environmental factors, including diet, are translated into lasting changes in gene expression. The gut microbiome produces a suite of metabolites that function as essential substrates and regulators of the host epigenetic machinery. Short-chain fatty acids (SCFAs), such as butyrate, propionate, and acetate, produced from the microbial fermentation of dietary fiber, act as potent histone deacetylase (HDAC) inhibitors, thereby influencing chromatin accessibility and gene transcription [85] [86]. Other microbial metabolites, including folate and other B vitamins, are crucial for one-carbon metabolism, which supplies methyl donors for DNA methylation processes [87].
This axis is not a static system but is dynamically influenced by a host of factors throughout the lifespan. As illustrated below, diet, age, and co-morbidities are not isolated confounders but exist in a state of continuous interaction, collectively shaping the microbiome and its epigenetic output. The following diagram maps the complex interplay between these core confounding factors and the primary research outcomes in this field.
Figure 1: Interplay of Core Confounding Factors. This pathway map illustrates how diet, age, and co-morbidities directly and indirectly influence the gut microbiome, its metabolite production, and subsequent host epigenetic modifications, ultimately confounding research outcomes.
Quantitative Impact of Confounding Factors
Dietary Patterns
Diet is arguably the most potent environmental modulator of the gut microbiome, with different dietary patterns leading to distinct microbial metabolite profiles that directly influence the host epigenome. The quantitative effects of established dietary patterns on disease risk and epigenetic aging are summarized in the table below.
Table 1: Impact of Dietary Patterns on Health and Epigenetic Outcomes
| Dietary Pattern | Key Microbiome & Metabolite Shifts | Associated Health Outcomes (Effect Size) | Impact on Epigenome |
|---|---|---|---|
| Western/UPF-Rich | ↓ Microbial diversity; ↓ SCFA producers (Ruminococcaceae, Lachnospiraceae); ↑ inflammation-associated taxa [88] [86]. | ↑ Rate of chronic disease accumulation (β=0.053 per 1-s.d. EDII increment) [89]; ↑ Weight gain & co-morbidity risk [88]. | Association with negative epigenetic changes (DNA methylation) linked to metabolic disorders [85]. |
| Mediterranean / AHEI / MIND | ↑ Microbial diversity; ↑ SCFA production (Butyrate, Acetate) [85] [86]. | ↓ Rate of chronic disease accumulation (β= -0.051 to -0.031 per 1-s.d. increment) [89]; Association with slower epigenetic aging [90]. | SCFAs (Butyrate, Acetate) act as HDAC inhibitors; positive influence on DNA methylation markers related to metabolic health [85] [87]. |
| High-Fiber/Polyphenol-Rich | ↑ Abundance of SCFA-producing bacteria (Bifidobacteria, Lactobacilli); ↑ Fecal SCFA concentrations [85] [86]. | Improved metabolic parameters (cholesterol, glucose, insulin); Weight loss (6.2 ± 3.9%) [85]. | Enhanced production of epigenetically-active metabolites (SCFAs); improved DNA methylation profiles [85]. |
The Empirical Dietary Inflammatory Index (EDII), which quantifies the inflammatory potential of diet, has been directly linked to the speed of multimorbidity accumulation. Conversely, anti-inflammatory diets like the Mediterranean-DASH Diet Intervention for Neurodegenerative Delay (MIND) and the Alternative Healthy Eating Index (AHEI) show protective effects [89]. These associations are not merely correlative; mechanistic studies show that high-fiber diets enhance microbial diversity and increase the production of short-chain fatty acids (SCFAs), which in turn function as histone deacetylase (HDAC) inhibitors and influence DNA methylation patterns, thereby mediating positive epigenetic changes [85] [86].
Age and Immunosenescence
Aging induces profound and predictable shifts in host physiology that directly confound microbiome-epigenome studies. The phenomenon of inflammaging—chronic, low-grade inflammation in older age—is coupled with immunosenescence, the progressive remodeling of the immune system [86]. These processes are intimately linked to age-related gut dysbiosis, characterized by a loss of beneficial SCFA producers (e.g., Faecalibacterium, Ruminococcaceae) and an increase in pro-inflammatory pathobionts [86] [87]. This dysbiosis can compromise intestinal barrier integrity, leading to metabolic endotoxemia and further fueling systemic inflammation, which is a known driver of epigenetic dysregulation [86].
Table 2: Age-Related Changes in Microbiome and Associated Epigenetic Effects
| Age Group | Characteristic Microbiome Shifts | Key Host Physiological Changes | Documented Epigenetic Consequences |
|---|---|---|---|
| Young / Middle-Aged Adult | High diversity; Stable composition; Robust SCFA production [86]. | Balanced immune function; Intact gut barrier; Low systemic inflammation. | Stable, health-associated epigenetic patterns; Metabolite-driven epigenetic regulation (e.g., by SCFAs) functions optimally. |
| Older Adult (65+ years) | ↓ Overall diversity; ↓ SCFA-producing bacteria; ↑ Proteobacteria; ↑ Inter-individual variability [86] [87]. | Immunosenescence; Inflammaging; Increased intestinal permeability ("leaky gut") [86]. | Accumulation of age-related epigenetic changes (e.g., epigenetic clock); Altered DNA methylation patterns linked to chronic disease [90]. |
| Specific Findings in the Oldest Old (≥78 years) | Association between MIND diet and slower total chronic disease accumulation was found only in this group (P for interaction=0.034) [89]. |
The impact of age is so significant that it can modulate the effect of other factors, such as diet. For instance, the protective association between the MIND diet and the rate of chronic disease accumulation was found to be significant only in the oldest old (≥78 years), highlighting the critical need for age-stratified analysis in research [89].
Co-morbidities
Pre-existing chronic diseases represent a major source of confounding, as they are often both a cause and a consequence of alterations in the gut microbiome and epigenome. The presence of multiple co-morbidities creates a complex feedback loop that can obscure the primary relationship being studied.
Table 3: Comorbidities as Confounders in Microbiome-Epigenome Research
| Comorbidity Type | Associated Microbiome Alterations | Interaction with Research Outcomes | Evidence of Confounding |
|---|---|---|---|
| Multimorbidity (General) | Decreasing diet quality with increasing number of chronic diseases [89]. | Shapes long-term multimorbidity trajectories and disease clustering (e.g., cardiovascular, neuropsychiatric) [89]. | In a 15-year study, 84.3% of older adults had multimorbidity at baseline, making it a near-ubiquitous confounder in aging research [89]. |
| Obesity & Metabolic Disease | Distinct DNA methylation patterns associated with BMI and Waist-to-Hip Ratio [91]. | Methylation sites with hypomethylation in obesity correlate positively with fat intake, creating nutrient-epigenetic interactions [91]. | In COVID-19, obesity consistently increased risk of severe disease or death after adjusting for age, demonstrating its independent confounding effect [92]. |
| Neuropsychiatric / Cognitive Impairment | ↓ Abundance of butyrate-producing bacteria (e.g., Faecalibacterium); ↓ Microbial diversity [87]. | Gut dysbiosis impacts brain epigenome via the gut-brain axis, influencing cognitive function [87]. | Fecal transplant from old donors to young mice induces cognitive impairment, mediated by a decrease in SCFA-producing bacteria [87]. |
The number of co-morbidities exhibits a dose-response relationship with health outcomes. During the COVID-19 pandemic, patients with a greater number of underlying conditions showed a progressively higher risk of severe disease and mortality, even after age-adjustment [92]. This underscores the necessity of meticulously recording and adjusting for co-morbidities, rather than simply using age as a proxy.
Experimental Protocols for Control and Mediation Analysis
Robust study design and analytical techniques are required to disentangle the effects of diet, age, and co-morbidities from the primary microbiome-epigenome interactions under investigation.
Longitudinal Study Designs with Repeated Measures
Protocol Detail: To address the dynamic nature of the microbiome and epigenome, implement studies with repeated measures of exposure, confounders, and outcomes over time. The Swedish SNAC-K cohort study, which examined multimorbidity accumulation over 15 years, serves as a exemplary model [89]. In this design, cumulative adherence to dietary patterns is calculated over the follow-up period, providing a more accurate exposure assessment than a single baseline measurement. This design allows researchers to model the trajectory of epigenetic changes or disease accumulation in relation to time-varying confounders.
Analysis Workflow:
- Data Collection: Collect longitudinal data on microbiome (e.g., 16S rRNA sequencing, metagenomics), epigenome (e.g., DNA methylation arrays), and confounders (FFQs, medical records for co-morbidities).
- Model Fitting: Use mixed-effects models or generalized estimating equations (GEE) to account for within-subject correlations over time.
- Confounder Adjustment: Include age, sex, smoking, energy intake, physical activity, and socioeconomic status as fixed-effect covariates. For DNA methylation analyses from blood, include estimated cell-type proportions as covariates to control for cellular heterogeneity [91].
- Trajectory Analysis: Apply group-based trajectory modeling to identify distinct clusters of disease or epigenetic aging progression [89].
Epigenome-Wide Association Studies (EWAS) with Confounder Adjustment
Protocol Detail: EWAS are a powerful tool for identifying epigenetic signatures of disease and exposure. However, they are highly susceptible to confounding. The protocol below, derived from a Korean EWAS on obesity, outlines a rigorous approach [91].
Analysis Workflow:
- DNA Methylation Processing & QC: Import methylation data from arrays (e.g., Illumina EPIC 850k). Filter out probes with low signal, cross-reactive probes, and those on sex chromosomes. Apply normalization (e.g., BMIQ) to correct for technical variation between probe types [91].
- Batch Effect Correction: Assess and correct for technical batch effects (e.g., from different processing slides) using methods like ComBat [91].
- Cell-Type Deconvolution: Estimate white blood cell proportions (e.g., using the Houseman algorithm) and include them as covariates in all models [93] [91].
- Modeling and Confounder Adjustment: For a phenotype of interest (e.g., obesity), fit a regression model where DNA methylation (M-value or Beta-value) is the outcome. Crucially, adjust for a comprehensive set of confounders:
- For BMI-defined obesity: Adjust for age, sex, smoking, waist-to-hip ratio, and cell-type proportions [91].
- For abdominal obesity: Adjust for age, sex, smoking, BMI, and cell-type proportions [91].
- For dietary exposures: Adjust for age, sex, smoking, BMI, alcohol consumption, and genetic background (e.g., via principal components) [93].
Mediation Analysis for Mechanistic Insight
Protocol Detail: To formally test whether the effect of an exposure (e.g., diet) on an outcome (e.g., disease risk) is transmitted through the microbiome and/or epigenome, a mediation analysis framework should be employed.
Analysis Workflow:
- Define Variables: Specify the independent variable (e.g., UPF consumption), mediator(s) (e.g., microbial diversity, SCFA levels, specific DNA methylation changes), and outcome (e.g., epigenetic age acceleration).
- Pathway Testing: Use structural equation modeling (SEM) or bootstrapping methods (e.g., the
mediationR package) to quantify the direct effect of the exposure on the outcome and the indirect effect that passes through the mediator. - Interpretation: A significant indirect effect provides statistical evidence for a mediating pathway, helping to move from association to causation. For example, testing if the effect of a high-fiber diet on cognitive health is mediated by an increase in butyrate-producing bacteria and subsequent changes in histone acetylation in the brain [87].
The Scientist's Toolkit: Key Research Reagent Solutions
Successfully navigating the confounders in this field requires a specific set of methodological tools and reagents. The following table details essential solutions for generating high-quality, reproducible data.
Table 4: Essential Research Reagents and Methods for Controlling Confounders
| Reagent / Method | Primary Function | Utility in Controlling Confounders |
|---|---|---|
| Infinium MethylationEPIC BeadChip (850K) [93] [91] | Profiling DNA methylation at >850,000 CpG sites across the genome. | The primary tool for EWAS. Allows for genome-scale discovery of epigenetic signatures associated with diet, age, and disease, while enabling statistical control for cell type. |
| Houseman Algorithm for Cell Deconvolution [93] [91] | Estimating proportions of immune cell types from bulk blood DNA methylation data. | Critically controls for confounding by variation in blood cell composition, which is associated with age, inflammation, and co-morbidities. |
| 16S rRNA Sequencing & Metagenomics [85] [86] | Characterizing the taxonomic composition and functional potential of the gut microbiome. | Quantifies the primary microbial community structure. Used to link specific dietary patterns (exposure) to microbial shifts (mediator/confounder). |
| Mass Spectrometry (LC-MS/NMR) [85] [93] | Quantifying microbial and host metabolites (e.g., SCFAs, vitamins, lipids) in serum, plasma, or stool. | Measures the functional output of the microbiome (e.g., SCFAs) that directly interacts with the host epigenome, providing a mechanistic link. |
| Short-Chain Fatty Acids (SCFAs) - Butyrate, Acetate, Propionate [85] [86] [87] | Used as in vitro or in vivo reagents to modulate epigenetic enzymes (e.g., HDAC inhibition). | Functional validation tools. Applying pure SCFAs allows researchers to test causal effects of microbiome-derived metabolites on epigenetic marks and gene expression. |
| Food Frequency Questionnaires (FFQs) & NOVA Classification [89] [88] | Standardized assessment of habitual dietary intake and classification of ultra-processed food (UPF) consumption. | Essential for accurately quantifying the primary exposure (diet) and classifying participants based on dietary patterns to control for this major confounder. |
| Fecal Microbiota Transplantation (FMT) in Gnotobiotic Mice [86] [87] | Transferring a donor microbiome into germ-free mice to establish cause-and-effect relationships. | The gold-standard experimental method to demonstrate causality. Allows testing if a microbiome from a specific donor (e.g., aged, diseased) can induce epigenetic and phenotypic changes in a recipient host. |
Integrated Signaling Pathways and Workflow Visualization
The following diagram synthesizes the experimental workflow and the core biological pathway into a single, integrated visualization. It outlines a robust research strategy from initial design through to data analysis, while simultaneously highlighting the key gut-microbiome-epigenome signaling axis that is the target of investigation.
Figure 2: Integrated Research Workflow and Biological Pathway. This diagram links the recommended research strategy (top) with the core biological pathway of interest (bottom), emphasizing where each step interacts with and controls for the complex system being studied. Dashed lines indicate key measurement and control points.
The investigation into how the gut microbiome modulates the host epigenome represents a frontier in precision health, revealing that gut microbiome profoundly influences host physiology by modulating epigenetic mechanisms such as DNA and RNA methylation [2] [1]. These discoveries emerge from complex datasets comprising genomic, metabolomic, and clinical information, creating an urgent need for robust ethical frameworks and data governance standards. The FAIR principles (Findable, Accessible, Interoperable, and Reusable) and CARE principles (Collective benefit, Authority to control, Responsibility, and Ethics) have emerged as critical frameworks for ensuring that microbiome data is not only computationally actionable but also ethically managed [2] [9]. As high-throughput methylation mapping, artificial intelligence, and single-cell multi-omics accelerate our ability to model these complex interactions, implementing these principles becomes paramount for enabling reproducible research and equitable clinical translation [2].
This technical guide provides researchers and drug development professionals with methodologies for implementing FAIR and CARE principles within gut microbiome-host epigenome studies. We outline concrete protocols, data governance models, and specialized tools to navigate the unique challenges presented by this rapidly advancing field, where microbial metabolites such as short-chain fatty acids (SCFAs) have been shown to regulate host methylation patterns through evolutionarily conserved pathways [2] [64].
Core Principles and Their Relevance to Microbiome-Epigenome Research
The FAIR Guiding Principles
The FAIR principles emphasize machine-actionability, ensuring data can be discovered and utilized by computational systems with minimal human intervention [94]. For microbiome-epigenome research, this involves standardizing diverse data types including DNA methylation patterns, microbial composition, metabolite measurements, and associated clinical metadata.
- Findable: Microbiome data must be assigned persistent identifiers and rich metadata that specifically describe epigenetic relevant parameters such as sequencing methods, methylation mapping techniques, and experimental conditions [95] [96].
- Accessible: Data should be retrievable by both humans and machines using standardized protocols, including authentication where necessary for privacy protection, particularly crucial for human microbiome data containing potentially identifiable host DNA sequences [96].
- Interoperable: Integration of data across different studies requires shared vocabularies and formats that can bridge microbiome composition (e.g., 16S rRNA gene amplicon sequencing) with epigenomic features (e.g., whole-genome bisulfite sequencing) [97].
- Reusable: Data should be richly described with provenance and meet domain-relevant community standards, enabling the pooling of datasets for powerful meta-analyses exploring microbiome-epigenome-disease relationships [95].
The CARE Principles for Indigenous Data Governance
The CARE principles complement FAIR by emphasizing people and purpose in data governance, ensuring that data ecosystems are designed and function to achieve equitable outcomes [2] [9]. These principles are particularly relevant when microbiome research involves Indigenous communities or populations with historical experiences of research exploitation.
- Collective Benefit: Research workflows should be designed to create benefits for participating communities, such as returning results or ensuring that commercial applications from microbiome discoveries provide equitable access.
- Authority to Control: Indigenous peoples and communities should have authority over how their data is used, including decisions about collection, use, and sharing of microbiome and associated health information.
- Responsibility: Researchers have responsibilities to demonstrate accountability for appropriate use of data by engaging in ethical sharing and honoring community protocols.
- Ethics: Research should minimize harms and maximize benefits for participating communities, recognizing that microbiome research could potentially reveal sensitive information about population-specific biological traits.
Implementation Challenges in Microbiome-Epigenome Studies
Technical and Analytical Challenges
Microbiome-epigenome research presents unique technical challenges for FAIR implementation. The field generates massive, multi-layered datasets through techniques including 16S rRNA gene amplicon sequencing, metagenomics, DNA methylation arrays, and metabolomics [97]. Each approach carries specific technical biases that must be documented for meaningful data reuse. For instance, DNA extraction methods significantly impact microbial community representation, with bead-beating recommended for fecal samples to ensure lysis of tough bacterial cells [97]. Similarly, methylation mapping techniques vary in resolution and coverage, affecting epigenetic interpretations.
Terminology precision is another critical challenge. Researchers must distinguish between "microbiota" (the community of microorganisms) and "microbiome" (which includes the theater of activity with structural elements, metabolites, and environmental conditions) [97]. Similarly, "16S rRNA gene amplicon sequencing" should not be truncated to "16S sequencing" or mislabeled as "metagenomics," as these methodologies provide fundamentally different information about functional potential versus taxonomic composition [97].
Privacy and Ethical Considerations
Human microbiome data presents unique privacy concerns that differentiate it from other genomic data. Metagenomic sequences may contain fragments of human host DNA, creating re-identification risks even when personal identifiers have been removed [96]. When combined with metadata such as age, sex, and approximate location, these datasets could potentially be used to identify participants, violating privacy regulations like the General Data Protection Regulation (GDPR) [96].
The situation is further complicated by the fact that host DNA scrubbing tools do not completely remove all human sequences and may inadvertently eliminate some non-host DNA, potentially biasing research results [96]. This creates a fundamental tension between FAIR principles advocating complete data transparency and ethical/legal requirements to protect participant privacy.
Table 1: Data Governance Challenges in Human Microbiome-Epigenome Research
| Challenge Category | Specific Issues | Potential Impacts |
|---|---|---|
| Data Complexity | Multi-omics data integration (microbiome, epigenome, metabolome) | Interoperability barriers between different analytical platforms |
| Technical Variability | DNA extraction protocols, sequencing depth, methylation detection methods | Reduced reproducibility between laboratories |
| Privacy Concerns | Host DNA in metagenomic sequences, geolocalized metadata | Re-identification risk despite pseudonymization |
| Ethical Considerations | Community rights under CARE principles, equitable benefit sharing | Potential restrictions on fully open data access |
| Regulatory Compliance | GDPR requirements, institutional review board variations | Cross-institutional data sharing complications |
Practical Implementation Framework
FAIR-Compliant Database Architecture
Implementing FAIR principles for human microbiome data requires specialized database architectures that balance accessibility with privacy protection. One effective approach uses Supabase, an open-source, real-time, relational database that can be deployed locally to handle sensitive information in compliance with GDPR [96]. This system employs pseudonymized unique identifiers for participants, enabling longitudinal data tracking while protecting identity.
The authentication system should incorporate multiple security layers, including two-factor authorization or Single Sign-On (SSO), with granular access controls that restrict data modification privileges to original uploaders or database moderators [96]. This maintains data integrity while permitting broader access for analysis. A large language model (LLM) interface can further enhance accessibility, allowing non-expert users to query the database using natural language while maintaining appropriate access restrictions [96].
Table 2: FAIR Implementation Components for Microbiome-Epigenome Databases
| System Component | Implementation Example | FAIR Principle Addressed |
|---|---|---|
| Unique Identifiers | Pseudonymized participant IDs with sample tracking | Findable, Reusable |
| Metadata Standards | Adherence to STREAMS reporting guidelines for microbiome studies | Interoperable, Reusable |
| Authentication | Supabase with email/password plus two-factor authentication | Accessible |
| API Access | Standardized queries for computational access | Accessible, Interoperable |
| Provenance Tracking | Detailed workflow documentation from sample collection to analysis | Reusable |
The Data Reuse Information (DRI) Tag System
To address tensions between data creators and consumers, the scientific community has proposed a Data Reuse Information (DRI) tag system [94]. This machine-readable metadata tag contains ORCIDs (Open Researcher and Contributor IDs) of data creators and indicates whether they prefer to be contacted before data reuse. The DRI tag system:
- Provides a clear communication pathway between data creators and consumers
- Respects the interests of researchers who generate valuable microbiome-epigenome datasets
- Facilitates collaborations while maintaining appropriate attribution
- Aligns with FAIR principle R.1 by providing a machine-readable data usage license [94]
Implementation requires integration with public sequence databases, with adoption encouraged through journal policies and institutional support. The system is particularly valuable for unpublished datasets, creating "safe spaces" for data creators to share information while maintaining their ability to publish first analyses [94].
Experimental Design and Metadata Standards
Rigorous experimental design is foundational to ethical and reproducible microbiome-epigenome research. Key considerations include:
- Appropriate Controls: Negative controls (reagent blanks) and positive controls (mock communities with known composition) should be included throughout extraction, sequencing, and analysis processes, particularly for low-biomass samples [97].
- Technical Replication: Multiple technical replicates account for variability in DNA extraction, library preparation, and sequencing.
- Sample Preservation: Standardized methods for sample collection, storage duration, and conditions must be meticulously documented to minimize technical artifacts [97].
- Metadata Documentation: Comprehensive reporting using standardized checklists like STREAMS (Standards for Technical Reporting in Environmental and host-Associated Microbiome Studies) ensures capture of critical methodological details [95].
Diagram 1: Integrated Workflow for Ethical Microbiome-Epigenome Research. This diagram illustrates the interconnection between experimental design, FAIR implementation, and CARE principles in a comprehensive research workflow.
Research Reagent Solutions and Methodologies
Table 3: Essential Research Tools for Microbiome-Epigenome Studies
| Tool/Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| DNA Extraction Kits | Bead-beating optimized kits (e.g., MP Biomedicals FastDNA Spin Kit) | Mechanical and chemical lysis for comprehensive microbial community representation [97] |
| Mock Communities | Defined bacterial mixtures (e.g., ZymoBIOMICS Microbial Community Standards) | Validation of taxonomic accuracy and detection limits in sequencing workflows [97] |
| Primer Sets | 16S rRNA gene primers (e.g., 515F-806R for V4 region), bisulfite conversion primers | Target-specific amplification for microbiome profiling and methylation analysis [97] |
| Blocking Reagents | PNA blockers for host DNA, chloroplast and mitochondrial blockers | Reduction of non-target amplification in host-associated samples [97] |
| Bioinformatics Tools | QIIME 2, DADA2, METHLYLSEEKER, Bowtie2 | Processing and analysis of sequencing data for taxonomic assignment and methylation mapping [2] [97] |
Standardized Protocol for Integrated Microbiome-Methylation Analysis
Protocol: Cross-Domain Analysis of Microbial Influences on Host Methylation Patterns
Sample Collection and Preservation
- Collect fecal samples in DNA/RNA stabilizing solution or flash-freeze in liquid nitrogen
- Preserve tissue samples for epigenomic analysis in RNAlater or similar preservative
- Include extraction blanks and mock communities with each batch of samples [97]
DNA Extraction and Quality Control
- Implement bead-beating step for mechanical disruption of tough bacterial cells
- Quantify DNA yield using fluorometric methods (e.g., Qubit)
- Assess quality via spectrophotometric ratios (A260/280) and gel electrophoresis [97]
Parallel Sequencing Library Preparation
- For microbiome analysis: Amplify 16S rRNA gene regions using dual-indexed primers to minimize index hopping [97]
- For methylation analysis: Treat DNA with bisulfite conversion reagents, followed by whole-genome bisulfite sequencing library preparation
- Include negative controls in amplification steps to detect contamination
Sequencing and Data Generation
- Sequence 16S amplicons on Illumina MiSeq (2×250 bp) or similar platform
- Conduct whole-genome bisulfite sequencing on Illumina NovaSeq or similar platform for sufficient coverage
- Apply unique dual indices to all samples to prevent demultiplexing errors [97]
Bioinformatic Processing and Integration
- Process 16S data through denoising pipeline (DADA2) and taxonomic assignment (SILVA or Greengenes database)
- Analyze bisulfite sequencing data using alignment to reference genome and methylation calling
- Perform integrated analysis to identify correlations between microbial features and methylation patterns
Implementing robust ethical frameworks and data governance models is not merely an administrative exercise but a scientific imperative in gut microbiome-host epigenome research. The intricate relationships between microbial metabolites, epigenetic reprogramming, and human health demand research practices that are both technically rigorous and ethically sound [2] [64]. By adopting the implementation strategies outlined in this guide—including FAIR-compliant database architectures, the DRI tag system for equitable data reuse, and standardized experimental protocols—researchers can accelerate discoveries while maintaining accountability to both research participants and the broader scientific community.
As Andrea Baccarelli has noted, "health doesn't only happen in the doctor's office" but develops over a lifetime of environmental exposures [98]. Understanding how the gut microbiome influences epigenetic responses to these exposures offers transformative potential for precision prevention strategies. Through committed application of FAIR and CARE principles, we can ensure that the resulting data ecosystems are not only scientifically valuable but also socially responsible, enabling discoveries that equitably benefit diverse populations.
Evidence and Efficacy: Validating the Axis in Disease and Aging Contexts
The human gut microbiome, a dynamic ecosystem of trillions of microorganisms, has emerged as a pivotal virtual endocrine organ that profoundly influences host physiology and cardiovascular health through multiple mechanistic pathways [99] [100]. Central to this interplay is the concept of the gut-heart axis, a bidirectional communication network through which gut microbiota and their metabolic products significantly impact cardiac function and disease progression [101] [102]. Heart failure (HF), affecting over 56 million individuals globally and representing a terminal stage of various cardiovascular pathologies, is now recognized to involve significant gut microbiota dysbiosis [99] [101]. This dysbiosis manifests as altered microbial community structure, intestinal barrier damage, and microbiota aging, which collectively contribute to HF pathogenesis through metabolic, immune, and inflammatory pathways [101] [102].
Recent advances have illuminated a sophisticated layer of regulation wherein gut microbiota-derived metabolites serve as key epigenetic modulators, creating a dynamic interface between environmental factors (notably diet) and host gene expression programs [1] [2]. This review examines the intricate relationships between specific microbial metabolites—particularly trimethylamine N-oxide (TMAO) and short-chain fatty acids (SCFAs)—and their roles in epigenetic reprogramming in the context of heart failure. We synthesize current evidence on mechanistic pathways, explore bidirectional regulatory mechanisms, and discuss translational applications for drug development and personalized medicine [102] [4].
Gut Microbiota-Derived Metabolites in Heart Failure: Bidirectional Regulators
The gut microbiota produces a diverse array of metabolites with often opposing effects on cardiovascular pathophysiology. These compounds can be broadly categorized as either protective or detrimental based on their net effects on cardiac structure and function, though some demonstrate context-dependent bidirectional regulation [102].
Table 1: Key Gut Microbiota-Derived Metabolites in Heart Failure Pathophysiology
| Metabolite | Primary Microbial Sources | Major Effects in HF | Key Mechanisms |
|---|---|---|---|
| TMAO (Trimethylamine N-oxide) | Firmicutes (e.g., Ruminococcus gnavus), Proteobacteria (e.g., Escherichia, Klebsiella) [99] | Detrimental [99] [102] | Promotes inflammation via NLRP3 inflammasome activation; induces fibrosis; disrupts epigenetic regulation via methionine cycle inhibition [99] [103] |
| SCFAs (Short-chain fatty acids) | Firmicutes (e.g., Faecalibacterium, Lactobacillus), Bacteroidetes [102] | Protective [99] [102] | Anti-inflammatory effects; maintain endothelial function; regulate blood pressure; support intestinal barrier integrity [104] [102] |
| PAGln (Phenylacetylglutamine) | Gut microbiota utilizing phenylalanine [100] | Detrimental [100] [102] | Promotes thrombotic pathways; enhances platelet responsiveness [100] |
| Bile Acids (Secondary) | Bacteroidetes, Firmicutes [104] [102] | Protective (context-dependent) [104] [102] | Lipid metabolism regulation; immune signaling through FXR and TGR5 receptors [104] |
| Indole Derivatives | Diverse commensals utilizing tryptophan [102] | Protective [102] | Antioxidant activity; anti-inflammatory effects; maintenance of metabolic homeostasis [102] |
HF patients exhibit characteristic alterations in gut microbiota composition compared to healthy individuals, typically showing reduced alpha and beta diversity, indicating lower bacterial richness and community variation [101]. Specific taxonomic changes include an increased abundance of proinflammatory bacteria belonging to genera Streptococcus and Escherichia-Shigella, coupled with decreased levels of beneficial bacteria with anti-inflammatory effects, particularly genera Faecalibacterium, Blautia, and Lachnospira [101]. This dysbiosis creates a microenvironment favoring the production of detrimental metabolites while diminishing protective signaling, ultimately accelerating HF progression through multiple interconnected pathways.
TMAO: Generation, Pathophysiological Mechanisms, and Epigenetic Regulation
TMAO Biosynthesis and Metabolic Pathways
TMAO is a gut microbiota-derived metabolite generated through a sequential process involving both microbial and host enzymes [99]. Dietary nutrients abundant in choline, L-carnitine, and betaine—primarily found in red meat, eggs, dairy products, and certain fish—serve as precursors for TMAO production [99]. The initial transformation occurs via specific gut microbial enzymes, notably choline TMA-lyase (CutC) and its activator (CutD), carnitine monooxygenase (CntA/B), and betaine reductase [99]. These enzymes convert dietary precursors into trimethylamine (TMA), which then crosses the intestinal barrier and enters portal circulation [99]. Upon reaching the liver, TMA is rapidly oxidized to TMAO by hepatic flavin-containing monooxygenases (FMOs), particularly FMO3, which demonstrates the highest activity for this conversion [99]. In healthy individuals, over 90% of TMAO is eliminated by renal excretion, but this clearance can be impaired in HF patients due to frequently associated renal dysfunction [99].
Systemic TMAO concentrations are influenced by multiple factors including dietary patterns, gut microbiota composition, hepatic FMO3 activity, renal function, age, genetics, and geographical region [99]. Notably, circulating TMAO levels vary substantially among healthy populations across different regions, with median levels of approximately 3.5 μmol/L in the United States compared to 1.70 μmol/L in healthy Chinese adults, likely reflecting dietary, genetic, and ethnic influences [99].
Pathophysiological Mechanisms in Heart Failure
TMAO contributes to HF progression through multiple interconnected mechanisms, with inflammation representing a central pathway [99]. Experimentally, elevated TMAO concentrations (e.g., 600 μmol/L) enhance expression of inflammatory genes and activate proinflammatory cytokines, thereby amplifying inflammatory responses [99]. Specifically, TMAO stimulates secretion of interleukin (IL)-1β by activating the nucleotide-binding oligomerization domain-like receptor containing pyrin domain 3 (NLRP3) inflammasome, leading to endothelial inflammation [99]. TMAO also inhibits the deacetylation of superoxide dismutase 2 (SOD2) by suppressing Sirtuin 3 (SIRT3), promoting oxidative stress—another key contributor to HF pathology [99].
Beyond inflammatory pathways, TMAO promotes cardiac fibrosis and adverse ventricular remodeling, ultimately contributing to systolic and diastolic dysfunction [102]. Clinical evidence consistently demonstrates that HF patients exhibit higher circulating TMAO levels compared to healthy controls, and TMAO serves as a valuable prognostic marker for both HF onset and progression [99] [1]. The presence of TMAO has been linked to plaque instability in atherosclerotic cardiovascular disease, which frequently underlies HF development [100].
Epigenetic Mechanisms of TMAO
Emerging research has illuminated sophisticated epigenetic mechanisms through which TMAO influences gene expression and cellular function [103]. TMAO directly disrupts the methionine cycle, a fundamental biochemical pathway essential for cellular methylation reactions [103]. Mechanistically, TMAO noncompetitively inhibits S-adenosylhomocysteine (SAH) hydrolase, leading to accumulation of SAH and subsequent reduction in global methylation capacity [103]. Since SAH is a potent feedback inhibitor of methyltransferases, its accumulation results in substantial impairment of diverse methylation reactions, including histone methylation and DNA methylation [103].
This disruption of the methionine cycle dynamically remodels chromatin states via altered histone posttranslational methylation and acetylation patterns [103]. Interestingly, different tissues exhibit varying sensitivity to TMAO-induced epigenetic changes, with brain cortex and hippocampus showing greater susceptibility compared to liver tissue at equivalent TMAO concentrations [103]. Experimental evidence demonstrates that in vitro overexpression of SAM synthase (methionine adenosyltransferase 2A) can rescue many TMAO-induced epigenetic defects by boosting the SAM/SAH ratio, highlighting the critical importance of balancing SAM synthesis and SAH clearance for maintaining proper epigenetic regulation [103].
Figure 1: TMAO Biosynthesis Pathway and Epigenetic Mechanisms in Heart Failure. This diagram illustrates the sequential process of TMAO generation from dietary precursors, its systemic circulation, and its epigenetic effects through disruption of the methionine cycle, ultimately contributing to heart failure pathology.
Short-Chain Fatty Acids: Protective Mechanisms and Epigenetic Influence
SCFA Production and Physiological Roles
Short-chain fatty acids (SCFAs), primarily acetate, propionate, and butyrate, are produced by gut microbiota through anaerobic fermentation of dietary fibers and resistant starches [104] [2]. These metabolites serve as crucial mediators of host-microbiome communication and exert predominantly beneficial effects on cardiovascular health [104] [102]. Protective bacterial genera significantly diminished in HF patients—including Faecalibacterium, Blautia, and Lachnospira—represent important SCFA producers, and their depletion contributes to the pathological milieu in heart failure [101] [102].
SCFAs influence host physiology through multiple mechanisms, including receptor binding, epigenetic modulation, and energy metabolism regulation [2]. They serve as ligands for specific G-protein-coupled receptors (GPCRs) such as GPR41, GPR43, and GPR109A, activation of which yields anti-inflammatory, antihypertensive, and endothelial-protective effects [104] [102]. Butyrate, in particular, enhances intestinal barrier function by facilitating tight junction assembly via activation of AMP-activated protein kinase in intestinal epithelial cells [1]. This barrier-strengthening effect is crucial in counteracting the "leaky gut" phenomenon frequently observed in HF patients, which permits translocation of bacterial products and exacerbates systemic inflammation [102].
Epigenetic Regulation by SCFAs
SCFAs function as potent epigenetic modulators primarily through inhibition of histone deacetylases (HDACs), with butyrate demonstrating particularly strong HDAC inhibitory activity [2]. By increasing histone acetylation, SCFAs promote a more open chromatin configuration that facilitates gene transcription, thereby influencing diverse cellular processes including immune regulation, inflammation, and cell differentiation [2]. This epigenetic mechanism underlies many of the anti-inflammatory effects of SCFAs, as HDAC inhibition typically suppresses pro-inflammatory gene expression while enhancing anti-inflammatory pathways [2].
The epigenetic influence of SCFAs extends to DNA methylation patterns through their roles in one-carbon metabolism [1] [2]. As key intermediaries in cellular metabolism, SCFAs contribute methyl groups that can influence the SAM/SAH ratio and consequently affect DNA methyltransferase activity [2]. This intersection between different epigenetic regulatory layers creates a sophisticated network through which gut microbiota can dynamically reprogram host gene expression in response to dietary inputs and environmental factors [1] [2].
Table 2: Comparative Analysis of Major SCFAs and Their Cardiovascular Effects
| SCFA Type | Primary Microbial Sources | Receptor Targets | Cardiovascular Effects | Epigenetic Mechanisms |
|---|---|---|---|---|
| Acetate | Bacteroides, Bifidobacterium, Prevotella | GPR43, GPR41 | Antihypertensive; endothelial protection; cardiometabolic regulation [104] [102] | HDAC inhibition; modulation of one-carbon metabolism [2] |
| Propionate | Bacteroides, Phascolarctobacterium, Coprococcus | GPR43, GPR41 | Anti-inflammatory; cholesterol synthesis inhibition; blood pressure regulation [104] [102] | HDAC inhibition; influence on DNA methylation patterns [2] |
| Butyrate | Faecalibacterium, Lachnospira, Roseburia, Eubacterium | GPR109A, GPR41 | Intestinal barrier enhancement; anti-inflammatory; anti-fibrotic; oxidative stress reduction [1] [102] | Potent HDAC inhibition; histone hyperacetylation; immune cell differentiation [2] |
Experimental Models and Methodological Approaches
Research Models for Gut-Heart Axis Investigation
Elucidating the complex relationships between gut microbiota, their metabolites, and cardiac pathophysiology requires sophisticated experimental models that capture the bidirectional nature of these interactions. Several well-established approaches facilitate mechanistic investigations:
Gnotobiotic Mouse Models: Germ-free mice colonized with specific microbial communities or human microbiota transplants enable researchers to establish causal relationships between particular microbial configurations and host phenotypes [104]. These models permit controlled manipulation of microbial composition and function, allowing for precise investigation of how specific bacteria influence TMAO and SCFA production and subsequent cardiovascular effects [104].
Fecal Microbiota Transplantation (FMT): FMT involves transferring fecal samples from donor organisms (often human patients with specific disease phenotypes) into recipient animals (typically mice) that have been pre-treated with broad-spectrum antibiotics to deplete their native gut microbiota [104]. This approach has demonstrated that gut microbiota alterations induced by various insults (e.g., sleep deprivation) are sufficient to cause cardiac dysfunction in recipient animals, establishing causality in gut-heart communication [104].
Bidirectional Mendelian Randomization Studies: This statistical approach uses genetic variants as instrumental variables to infer causal relationships between gut microbiota composition and cardiovascular outcomes while mitigating confounding factors [104]. Although preliminary associations between gut microbiota and conditions like aortic aneurysms have been observed, many fail to maintain statistical significance after rigorous correction for multiple comparisons, highlighting the complex, multifactorial nature of these relationships [104].
Genetic Manipulation Models: Knockout or silencing of specific genes involved in metabolite production or processing (e.g., hepatic FMO3 knockout in mice) enables researchers to dissect specific metabolic pathways [99]. These models have demonstrated that FMO3 deficiency decreases circulating TMAO levels, confirming the enzyme's central role in TMAO generation [99].
Analytical Methods for Metabolite and Epigenetic Profiling
Advanced analytical techniques are essential for quantifying microbial metabolites and assessing their epigenetic effects:
Metabolomic Profiling: High-performance liquid chromatography coupled with mass spectrometry (LC-MS/MS) provides sensitive and specific quantification of TMAO, SCFAs, and related metabolites in biological samples including plasma, urine, and tissues [99] [103]. Stable isotope-labeled tracers enable dynamic tracking of metabolite production, distribution, and elimination [99].
Epigenetic Mapping: High-throughput methylation mapping techniques, including whole-genome bisulfite sequencing (WGBS) and reduced representation bisulfite sequencing (RRBS), allow comprehensive assessment of DNA methylation patterns [1] [2]. Chromatin immunoprecipitation followed by sequencing (ChIP-seq) facilitates examination of histone modifications, while ATAC-seq evaluates chromatin accessibility [2].
Multi-omics Integration: Combining metagenomic sequencing (microbial community analysis), metabolomic profiling (metabolite quantification), and epigenomic mapping (host epigenetic status) through advanced computational approaches enables construction of comprehensive models of microbiome-host interactions [1] [2]. Artificial intelligence and machine learning algorithms are increasingly employed to identify patterns and predictive relationships within these complex datasets [1] [9].
Figure 2: Experimental Workflow for Investigating Microbiome-Epigenome Interactions in Heart Failure. This diagram outlines integrated approaches from preclinical models through analytical methods to therapeutic interventions, highlighting the translational pathway from basic discovery to clinical application.
Table 3: Key Research Reagents for Investigating Microbiota-Epigenetic Interactions in Heart Failure
| Reagent/Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Animal Models | Gnotobiotic mice; FMO3 knockout mice; ApoE-/- mice with microbiota manipulation [99] [104] | Establishing causality in gut-heart axis; pathway validation; therapeutic testing [99] [104] | Require specialized facilities; diet control critical; microbiota monitoring essential |
| Chemical Inhibitors | DMB (3,3-dimethyl-1-butanol); iodomethylcholine [99] [100] | Inhibition of microbial TMA lyase; reducing TMA/TMAO production [99] | Specificity varies; potential off-target effects; dose optimization needed |
| Analytical Standards | Stable isotope-labeled TMAO (d9-TMAO); 13C-SCFAs; deuterated internal standards [99] [103] | Metabolite quantification via LC-MS/MS; calibration; tracer studies [99] | Purity critical for accurate quantification; proper storage conditions |
| Epigenetic Assay Kits | HDAC activity assays; DNA methylation kits (e.g., EpiTect Methyl II); ChIP kits with specific histone antibodies [2] | Evaluating epigenetic modifications; histone acetylation/methylation status; DNA methylation patterns [2] | Antibody specificity crucial; appropriate controls essential; cell/tissue input quality matters |
| Cell Culture Systems | Primary cardiomyocytes; cardiac fibroblasts; endothelial cells; hepatocytes [99] [103] | Mechanistic studies of metabolite effects; signaling pathway analysis; epigenetic changes [103] | Physiological relevance of concentrations; cell type-specific responses; microenvironment considerations |
Therapeutic Implications and Future Directions
Microbiota-Targeted Interventions
The recognition of TMAO, SCFAs, and related metabolites as key players in heart failure pathogenesis has stimulated development of novel therapeutic strategies targeting the gut-heart axis:
Dietary Interventions: Modification of dietary patterns represents the most straightforward approach to modulating microbial metabolite profiles. Reduced consumption of TMAO precursors (e.g., red meat, eggs, high-fat foods) while increasing intake of dietary fiber and polyphenol-rich foods can favorably shift the balance between detrimental and protective metabolites [99] [100]. Specific dietary components such as resveratrol, allicin, and berberine have demonstrated potential to inhibit TMA formation and reduce TMAO levels [99].
Pharmacologic Enzyme Inhibitors: Targeted inhibition of microbial enzymes involved in TMA production offers a promising therapeutic strategy. Compounds such as 3,3-dimethyl-1-butanol (DMB) and iodomethylcholine selectively inhibit microbial TMA lyase (CutC) activity, significantly reducing TMA and TMAO levels without apparent toxicity [99] [100]. These inhibitors demonstrate the potential for precise targeting of microbial metabolic pathways while avoiding direct effects on host physiology.
Precision Probiotics and Postbiotics: Administration of selected bacterial strains with beneficial metabolic profiles (e.g., SCFA producers) or the direct delivery of protective metabolites (postbiotics) represents another promising approach [1] [100]. Restoration of diminished protective genera like Faecalibacterium, Blautia, and Lachnospira could theoretically reestablish a healthier microbial ecosystem and metabolite profile in HF patients [101] [102].
Fecal Microbiota Transplantation (FMT): Although currently primarily investigational for cardiovascular applications, FMT offers the potential to rapidly and comprehensively reshape the gut microbial community structure [104]. This approach has demonstrated promise in animal models, where transplantation of microbiota from healthy donors can ameliorate disease phenotypes in recipient animals [104].
Challenges and Future Perspectives
Despite substantial progress, several challenges remain in translating microbiome-epigenome research into clinical applications for heart failure management:
Establishing Causal Relationships: While numerous associations between microbial metabolites and HF phenotypes have been identified, definitive causal relationships remain difficult to establish in human populations [100]. The bidirectional nature of gut-heart communication further complicates causal inference, as HF itself induces gut dysbiosis through mechanisms including intestinal hypoperfusion, congestion, and neurohormonal activation [102].
Population Heterogeneity: Significant interindividual variation in gut microbiota composition, driven by factors including genetics, diet, age, medication use, and geographic location, complicates the development of universal interventions [99] [101]. Future approaches will likely require personalization based on individual microbial and metabolic profiling [1] [9].
Context-Dependent Effects of Metabolites: Some microbial metabolites demonstrate bidirectional or context-dependent effects based on concentration, timing, host status, and disease stage [102]. For instance, certain bile acid species may exert protective effects in some contexts but contribute to pathology in others, necessitating sophisticated understanding of these dynamic relationships [104] [102].
Integration into Clinical Practice: Practical implementation of microbiota-targeted therapies faces barriers including regulatory challenges, safety concerns (particularly with FMT), and integration with existing HF treatment paradigms [100]. Additionally, the field requires standardized methodologies for microbiota assessment, metabolite measurement, and epigenetic analysis to enable comparison across studies and populations [1] [2].
Future research directions should prioritize longitudinal human studies with repeated sampling, multi-omics integration to capture the complexity of host-microbe interactions, randomized controlled trials of targeted interventions, and development of sophisticated computational models to predict individual responses to microbiota-directed therapies [100] [2]. As our understanding of the intricate relationships between gut microbiota, their metabolites, and host epigenetic regulation deepens, we move closer to realizing the promise of personalized, microbiome-informed approaches to heart failure prevention and treatment [1] [9].
The gut-brain axis has emerged as a critical communication network in human physiology, with growing evidence establishing its fundamental role in neurological and psychiatric disorders [105]. This bidirectional pathway facilitates complex interactions between the central nervous system (CNS), enteric nervous system, and gastrointestinal tract functionality. Recent research has revealed that the gut microbiota, a diverse ecosystem of trillions of microorganisms, significantly influences this axis through multiple mechanisms, including the production of bioactive metabolites, immune system modulation, and neural pathway activation [106]. The human gut harbors over 3 million functionally diverse microbial genes that produce metabolites vital for host functions, far surpassing the 23,000 protein-coding genes in the human genome [106].
Advancements in our understanding of this system have uncovered a more sophisticated framework: the microbiota-gut-brain-epigenome axis. This expanded model reveals that microbial communities within the gastrointestinal tract can exert lasting influence on host physiology by modulating epigenetic mechanisms such as DNA methylation, histone modifications, and RNA interference [53] [1]. The gut microbiome functions as a dynamic interface that translates environmental inputs—including diet, stress, and medications—into epigenetic signals that regulate gene expression and phenotypic plasticity in both peripheral tissues and the central nervous system [53].
This whitepaper examines how gut microbiota composition and function contribute to the pathophysiology of bipolar disorder (BD) and autism spectrum disorder (ASD) through epigenetic reprogramming. We synthesize recent clinical and preclinical findings, detail methodological approaches for investigating these relationships, and explore the translational potential of microbiota-targeted interventions for managing these complex conditions.
Mechanistic Insights: Microbial Influence on Host Epigenetics
The molecular pathways through which gut microbiota influence host epigenetics are increasingly elucidated, revealing several conserved biological mechanisms. Understanding these pathways is essential for appreciating how microbial communities distal to the brain can ultimately influence neural function and behavior.
Key Epigenetic Pathways Modulated by Gut Microbiota
Table 1: Primary Mechanisms of Microbiota-Epigenome Interaction
| Mechanism | Key Microbial Signals | Epigenetic Impact | Functional Consequences |
|---|---|---|---|
| One-carbon metabolism | Folate, B vitamins, choline | Alters methyl donor availability for DNA/histone methylation | Changes in neural gene expression, neurotransmitter synthesis |
| Short-chain fatty acid (SCFA) signaling | Butyrate, acetate, propionate | HDAC inhibition, DNA methyltransferase modulation | Microglial maturation, blood-brain barrier integrity, neuroinflammation regulation |
| Polyamine biosynthesis | Spermidine, spermine | Histone and DNA methylation changes | Cellular growth, synaptic plasticity, autophagy regulation |
| Extracellular vesicle communication | miRNAs, proteins, metabolites | Intercellular epigenetic transfer | Long-distance signaling, immune cell programming |
Gut microbiota regulate host epigenetic patterns primarily through metabolite production and signaling molecules [53]. Short-chain fatty acids (SCFAs)—including butyrate, acetate, and propionate—are produced through microbial fermentation of dietary fiber and demonstrate significant epigenetic activity. Butyrate, in particular, functions as a potent histone deacetylase (HDAC) inhibitor, increasing histone acetylation and promoting gene expression in regions critical for neuronal function and development [106]. Butyrate also promotes glial cell-derived neurotrophic factor (GDNF) expression in astrocytes, which are essential for regulating neuronal growth, survival, and synaptic differentiation [106].
Beyond SCFAs, gut microbes influence host one-carbon metabolism, a fundamental biochemical pathway that supplies methyl groups for DNA and histone methylation reactions [53]. Microbial synthesis of B vitamins (particularly folate and B12) and choline metabolism directly affect the availability of S-adenosylmethionine (SAM), the primary methyl donor for epigenetic modifications. Disruption of these metabolic pathways can lead to widespread alterations in methylation patterns of genes involved in neurodevelopment and neurotransmitter signaling.
Microbiota-host communication also occurs through extracellular vesicles that carry proteins, metabolites, and nucleic acids, including miRNAs that can directly influence host gene expression through RNA interference mechanisms [53]. These vesicles facilitate the transfer of epigenetic information between kingdoms, potentially enabling long-lasting changes in host physiology.
Figure 1: Microbial Influence on Host Physiology. Gut microbiota generate metabolites that impact host biology through multiple parallel pathways, including direct epigenetic modulation, immune system activation, barrier function regulation, and neural signaling.
Neuroactive Microbial Metabolites and Epigenetic Consequences
The gut microbiota produces and modulates numerous neuroactive metabolites that influence brain function both directly and through epigenetic mechanisms. These include:
Tryptophan metabolites: The kynurenine pathway, responsible for breaking down the essential amino acid tryptophan, represents a crucial link between gut microbiota and brain function [107]. Research in ASD patients has revealed significantly reduced levels of kynurenine pathway metabolites, particularly kynurenate, which were associated with alterations in task-based brain activity and increased symptom severity [107]. Disruption of this pathway is linked to impaired brain processing and cognitive changes in neuropsychiatric disorders.
GABA and serotonin: Gut microbes significantly influence the production of key neurotransmitters. Approximately 90% of the body's serotonin is synthesized in the gut, where its production is influenced by gastrointestinal microbiota [106]. Similarly, GABA, the primary inhibitory neurotransmitter in the brain, is produced by various human microbiota communities, including Lactobacillus brevis and Bifidobacterium dentium [106]. While GABA produced in the gut cannot directly cross the blood-brain barrier, it can indirectly affect brain function by modulating vagus nerve activity or enteric nervous system function.
Bile acid derivatives: Gut bacteria metabolize primary bile acids from the liver into secondary bile acids, which can function as signaling molecules that influence host metabolism and inflammation through epigenetic mechanisms [106].
These microbial metabolites demonstrate the sophisticated chemical communication between gut microbiota and the host nervous system, with epigenetic modifications serving as a molecular memory of this cross-kingdom dialogue.
Disorder-Specific Analyses: Bipolar Disorder and Autism Spectrum Disorder
Bipolar Disorder: Gut Microbiota and Cognitive Impairment
Recent research has established compelling connections between gut microbiota composition and bipolar disorder, particularly regarding the cognitive impairment that frequently persists during euthymic periods. A 2025 study examining gut microbial structure in BD patients with and without cognitive impairment (BD-CI and BD-nCI) revealed significant differences in both diversity and composition compared to healthy controls [108].
Table 2: Gut Microbiota Alterations in Bipolar Disorder
| Microbial Taxa | Association with BD | Functional Correlations | Research Context |
|---|---|---|---|
| Prevotellaceae | Increased abundance in BD | Correlated with cognitive impairment test scores | 16S-rRNA sequencing in BD patients [108] |
| Faecalibacterium | Decreased in BD | SCFA production; anti-inflammatory effects | Multiple studies across BD populations [109] |
| Lachnoclostridium | Increased in BD | Associated with depressive severity | Correlation with HAMD scores [108] |
| Bacteroides | Variable alterations | Inflammation-related pathways | Mendelian randomization study [110] |
| Ruminococcaceae UCG005 | Protective effect | Cognitive preservation | Associated with reduced BD risk [110] |
The relationship between gut microbiota and cognitive function in BD appears mediated by effects on neuronal plasticity. Fecal microbiota transplantation (FMT) from BD patients to antibiotic-treated mice recapitulated key behavioral and neurobiological features of the disorder [108]. Mice receiving transplants from BD-CI donors exhibited more severely impaired object recognition memory, along with greater reductions in dendritic complexity and synaptic plasticity compared to those receiving microbiota from BD-nCI donors [108]. These findings suggest that gut microbiota influences cognitive function in BD through structural and functional modifications of neural circuits.
Adolescents with BD represent a particularly vulnerable population, as this developmental period involves significant neuronal reorganization and gut ecosystem maturation [109]. A study of unmedicated BD adolescents revealed distinct gut microbial communities correlated with metabolic pathways involving SCFAs, choline, lipids, vitamins, polyamines, and aromatic amino acids [109]. Four-week quetiapine treatment modified the abundance of specific bacterial genera (Odoribacter splanchnicus, Oribacterium sinus, Hafnia alvei), suggesting that effective pharmacotherapy may partially exert its benefits through microbiota modulation.
Neuroimaging analyses further linked these microbial alterations to brain function, revealing that sensory-emotional brain regions were associated with BD severity [109]. Importantly, machine learning models demonstrated that combining gut microbiota and neuroimaging data provided superior predictive efficacy for diagnosing BD and forecasting treatment response compared to either dataset alone, highlighting the potential clinical utility of multi-modal biomarkers.
Autism Spectrum Disorder: Microbial Metabolites and Brain Function
Research on autism spectrum disorder has similarly revealed distinctive alterations in gut microbiome composition and function, with implications for both gastrointestinal symptoms and core behavioral features of the condition. Children with ASD exhibit significantly different gut microbial profiles compared to neurotypical controls, including increased abundances of genera such as Clostridium, Ruminococcus, Sutterella, and Lactobacillus, and decreased levels of Bifidobacterium, Akkermansia, Blautia, and Prevotella [106].
A comprehensive study examining gut-brain microbiome interactions in ASD found that children with ASD had significantly reduced levels of neuroactive metabolites derived from gut microbes [107]. Specifically, researchers observed decreased concentrations of metabolites in the kynurenine pathway, including kynurenate, which plays a crucial role in tryptophan metabolism and neurotransmitter balance [107]. These metabolic alterations were associated with changes in task-based brain activity and correlated with increased severity of ASD symptoms.
The maternal microbiome during pregnancy and early postnatal microbial colonization may represent critical windows for neurodevelopmental programming [107]. During pregnancy, bacterial metabolites can be transferred from mother to fetus, and alterations in the maternal gut microbiome can suppress gut tight junction gene expression in the offspring [106]. This could potentially expose the developing fetus to biomacromolecules and microorganisms that trigger neuroinflammatory mechanisms, influencing ASD vulnerability.
Figure 2: Shared Pathways in BD and ASD Pathophysiology. Despite distinct clinical presentations, bipolar disorder and autism spectrum disorder share common pathways involving microbiome disruption, metabolite imbalance, barrier dysfunction, neuroinflammation, and impaired neuroplasticity.
Methodological Approaches: From Correlation to Causation
Establishing causal relationships between gut microbiota and neuropsychiatric disorders requires sophisticated methodological approaches that move beyond observational correlations. Several advanced techniques have strengthened the evidence for microbiome involvement in BD and ASD pathogenesis.
Fecal Microbiota Transplantation (FMT) Protocols
Fecal microbiota transplantation represents a powerful experimental approach for investigating causal relationships between gut microbiota and disease phenotypes. The standard FMT protocol involves several critical steps [108]:
- Donor screening: Comprehensive medical history and laboratory testing to exclude transmissible pathogens
- Fecal sample collection: Fresh stool samples collected in anaerobic conditions and processed within a few hours
- Sample processing: Homogenization with sterile PBS-glycerol solution (typically 1g feces per 30-40mL solution)
- Filtration and centrifugation: Removal of particulate matter while preserving microbial communities
- Transplantation administration: Oral gavage in animal models or colonoscopy/encapsulated formulations in humans
In BD research, FMT from patients to antibiotic-treated mice has successfully transmitted behavioral phenotypes, with mice receiving microbiota from BD-CI donors exhibiting more severe cognitive deficits and neuronal plasticity impairments than those receiving microbiota from BD-nCI donors or healthy controls [108]. This approach provides compelling evidence for the causal role of gut microbiota in mediating cognitive aspects of BD.
Mendelian Randomization and Genetic Approaches
Mendelian randomization (MR) leverages genetic variants as instrumental variables to strengthen causal inference in microbiome-disease relationships. A recent MR analysis harnessed genetic data from large-scale genome-wide association studies to analyze how 196 gut microbiota taxa affect ten psychiatric disorders via alterations in 3,143 brain structures [110].
This approach identified significant bidirectional causal relationships, with certain gut microbiota taxa (e.g., Bacteroides and Marvinbryantia) associated with changes in brain activity and white matter integrity, while brain structures like the right hippocampus and left superior cerebellar peduncle influenced gut microbiota composition [110]. The study further revealed that brain structures mediated the effects of gut microbiota on five psychiatric disorders, including bipolar disorder, with the influence of gut microbiota fully transmitted through changes in brain structure in these cases.
Metagenomic Sequencing and Metabolomic Profiling
Advanced sequencing technologies enable comprehensive characterization of gut microbial communities and their functional capacities. Shotgun metagenomic sequencing provides superior taxonomic resolution and functional information compared to 16S rRNA sequencing, allowing researchers to identify specific microbial strains and metabolic pathways associated with disease states [109].
In studies of adolescent BD, metagenomic sequencing revealed correlations between microbial alterations and metabolic pathways involving short-chain fatty acids, choline, lipids, vitamins, polyamines, and aromatic amino acids [109]. These functional insights complement taxonomic profiling and provide mechanistic hypotheses for how microbial communities influence host physiology.
Metabolomic profiling further bridges the gap between microbial composition and host response by quantitatively measuring the small molecule metabolites present in biological samples. In ASD research, metabolomic analyses have identified reduced levels of kynurenine pathway metabolites in children with ASD, providing a direct link between microbial metabolic activity and neurological function [107].
Figure 3: Comprehensive Research Workflow for Investigating Microbiome-Brain Connections. A multi-modal approach integrating clinical assessment, multi-omics technologies, neuroimaging, and mechanistic validation provides the most robust evidence for microbiome involvement in neuropsychiatric disorders.
Table 3: Key Research Reagents and Platforms for Microbiome-Epigenome Studies
| Category | Specific Tools/Reagents | Application | Considerations |
|---|---|---|---|
| DNA Extraction Kits | OMEGA-soil DNA Kit, QIAamp PowerFecal Pro DNA Kit | Metagenomic sequencing from stool samples | Mechanical disruption critical for Gram-positive bacteria |
| Sequencing Platforms | Illumina NovaSeq, PacBio Sequel, Oxford Nanopore | Metagenomic characterization | Trade-offs between read length, accuracy, and cost |
| Epigenetic Mapping | Methylated DNA immunoprecipitation (MeDIP), Whole-genome bisulfite sequencing | DNA methylation analysis | Coverage depth requirements depend on research questions |
| Animal Models | Germ-free mice, Antibiotic cocktail treatment, Humanized microbiota mice | Causal inference studies | Germ-free mice have developmental abnormalities |
| Behavioral Assessment | Object recognition test, Morris water maze, Social interaction tests | Cognitive and behavioral phenotyping | Multiple tests needed to assess different domains |
| Microbiota Modulation | Fecal microbiota transplantation, Probiotic formulations, Prebiotic supplements | Intervention studies | Donor screening critical for FMT safety |
The OMEGA-soil DNA Kit has been specifically employed in BD research for extracting DNA from thawed fecal samples, incorporating both enzymatic digestion (lysozyme solution) and mechanical disruption (bead-beating) to ensure comprehensive lysis of diverse bacterial species [109]. This thorough extraction methodology is particularly important for studying Gram-positive bacteria with robust cell walls that may resist standard lysis procedures.
For epigenetic analyses, techniques such as whole-genome bisulfite sequencing provide comprehensive mapping of DNA methylation patterns across the genome, while methylated DNA immunoprecipitation (MeDIP) offers a cost-effective alternative for focused investigations [53]. Recent advances in single-cell multi-omics now enable simultaneous profiling of epigenetic modifications and gene expression in individual cells, offering unprecedented resolution for understanding cellular heterogeneity in response to microbial signals.
Behavioral assessment represents another critical component, with tests like the object recognition memory task proving sensitive to microbial manipulations in BD models [108]. A comprehensive behavioral battery should evaluate multiple domains, including anxiety-like behavior, social interaction, learning and memory, and motivation to address the complex behavioral alterations characteristic of neuropsychiatric disorders.
Therapeutic Implications and Future Directions
The recognition of gut microbiota's role in bipolar disorder and autism spectrum disorder has stimulated development of novel microbiota-targeted therapeutic interventions with potential to modulate disease course and symptoms.
Microbiota-Targeted Interventions
Table 4: Microbiota-Targeted Interventions for Neuropsychiatric Disorders
| Intervention Type | Mechanism of Action | Efficacy Evidence | Considerations |
|---|---|---|---|
| Probiotics | Live beneficial bacteria; direct microbial modulation | Moderate behavioral improvements in ASD; multi-strain formulations more effective | Strain-specific effects; colonization persistence uncertain |
| Prebiotics | Non-digestible fibers promoting beneficial bacteria | Mixed results in ASD; some benefits in behavioral and GI symptoms | Dose-dependent effects; individual microbiome composition matters |
| Synbiotics | Combination of probiotics and prebiotics | Promising for GI symptoms; variable behavioral effects | Rational strain-fiber pairing needed for optimal effect |
| Fecal Microbiota Transplantation | Complete microbial community restoration | Most consistent and sustained improvements in ASD symptoms | Donor selection critical; long-term safety monitoring needed |
| Dietary Interventions | Mediterranean diet, high-fiber diets | Modulates SCFA production; influences epigenetic programming | Cultural and individual adherence challenges |
For autism spectrum disorder, a comprehensive systematic review of 33 studies found that microbiota-targeted interventions show promise for managing both behavioral and gastrointestinal symptoms [111]. Among these approaches, fecal microbiota transplantation (FMT) demonstrated the most consistent and sustained improvements, with benefits persisting for extended follow-up periods [111]. Probiotics showed moderate behavioral improvements, with multi-strain formulations proving more effective than single strains, while prebiotics and synbiotics yielded mixed results across studies [111].
In bipolar disorder research, quetiapine treatment over four weeks modified the abundance of specific bacterial genera, including Odoribacter splanchnicus, Oribacterium sinus, and Hafnia alvei [109]. This suggests that effective pharmacotherapies may partially exert their therapeutic benefits through microbiota modulation, opening avenues for adjunctive microbiota-targeted treatments to enhance efficacy or reduce side effects of conventional medications.
Future Research Directions
Several promising research directions emerge from current findings:
Mechanistic deep-dive: Further elucidation of how specific microbial metabolites influence host epigenetic machinery in neural cells, including cell-type-specific effects in different brain regions [53]
Developmental timing: Investigation of critical windows for microbiome-epigenome interactions during neurodevelopment, potentially informing early intervention strategies [107]
Personalized approaches: Development of microbiome-informed precision medicine based on individual microbial and epigenetic profiles [53] [111]
Standardization and reproducibility: Implementation of rigorous standardization in microbiome research, including adherence to FAIR and CARE principles for data governance [53]
Intervention optimization: Controlled trials to determine optimal formulations, timing, and delivery methods for microbiota-targeted therapies [111]
The integration of high-throughput methylation mapping, artificial intelligence, and single-cell multi-omics is accelerating our ability to model these complex interactions at high resolution [53]. These technological advances, combined with rigorous clinical studies, promise to unlock the therapeutic potential of targeting the microbiota-gut-brain-epigenome axis for bipolar disorder, autism spectrum disorder, and other neuropsychiatric conditions.
The expanding knowledge of microbiota-gut-brain-epigenome interactions represents a paradigm shift in our understanding of neuropsychiatric disorders. Research in bipolar disorder and autism spectrum disorder consistently demonstrates that gut microbiota influence brain function and behavior through multiple interconnected pathways, with epigenetic mechanisms serving as a crucial interface that translates microbial signals into lasting changes in gene expression and neural circuit function.
The findings summarized in this whitepaper highlight the therapeutic potential of microbiota-targeted interventions while emphasizing the need for mechanistic depth and methodological rigor. As research progresses, integration of multi-omics data, advanced neuroimaging, and carefully designed intervention studies will be essential for translating these insights into effective precision medicine approaches for individuals with neuropsychiatric conditions.
Understanding how microbial factors reshape host epigenetic landscapes may reveal novel therapeutic avenues for alleviating genetic and epigenetic constraints on mental health, ultimately leading to more effective and personalized treatment strategies for bipolar disorder, autism spectrum disorder, and related conditions.
The aging process is characterized by a progressive decline in physiological function and an increased susceptibility to chronic diseases. Central to this process is the epigenetic drift, a term describing the cumulative, reversible alterations to the genome that regulate gene expression without changing the DNA sequence itself [112] [113]. These changes—spanning DNA methylation, histone modifications, and chromatin remodeling—constitute a central regulator of organismal decline. Simultaneously, the gut microbiome, a dynamic ecosystem of trillions of microorganisms, undergoes significant transformations with age. The emerging paradigm posits that the aging process cannot be fully understood by examining the human genome in isolation; rather, it must be viewed through the lens of the holobiont—the biological system composed of the host and all its associated microbiota [114]. This review delineates the specific mechanisms by which the aging gut microbiome influences the host epigenome, driving the characteristic chronic inflammatory state known as "inflammaging," and explores the translational potential of these insights for diagnostic and therapeutic innovation.
Fundamental Epigenetic Mechanisms in Aging
A comprehensive understanding of the microbial influence on the aging epigenome requires a foundation in the core epigenetic mechanisms that undergo age-related alterations.
DNA Methylation Dynamics
DNA methylation involves the addition of a methyl group to cytosine bases, primarily in CpG dinucleotides, catalyzed by DNA methyltransferases (DNMTs) [112] [113]. The three principal enzymes are DNMT1 (a maintenance methyltransferase) and DNMT3A and DNMT3B (de novo methyltransferases). During aging, a paradoxical pattern emerges: global hypomethylation concomitant with focal hypermethylation at specific sites, such as CpG islands in gene promoters [112]. This shift arises from age-stage-specific and stress-signal-specific transcriptional regulation of DNMTs; for instance, DNMT1 is often suppressed, while DNMT3A/3B can be upregulated, leading to the distinctive "aging epigenetic signature" [112]. These changes can silence crucial genes, including tumor suppressors, and impact stem cell function, thereby accelerating the aging process [112].
Histone Modifications and Chromatin Remodeling
Aging is associated with a general loss of histones and alterations in their post-translational modifications [113]. Changes in acetylation, methylation, phosphorylation, and ubiquitination patterns on histone tails can either activate or repress gene expression. For example, a reduction in histone H3 and H4 acetylation is linked to heterochromatin formation and transcriptional silencing of genes essential for maintaining youthfulness [113]. Furthermore, the three-dimensional architecture of chromatin becomes remodeled with age, affecting the accessibility of genes to transcriptional machinery.
Epigenetic Clocks as Biomarkers
Epigenetic clocks are predictive models that use the methylation status of a defined set of CpG sites to accurately estimate biological age [112] [113]. First-generation clocks (e.g., Horvath's clock) predict chronological age, while second-generation clocks (e.g., PhenoAge, GrimAge) incorporate clinical parameters and show stronger associations with mortality risk and age-related conditions [115] [114]. These clocks demonstrate the plasticity of the epigenome and its responsiveness to lifestyle, stress, and, as emerging evidence suggests, the gut microbiome [115].
Table 1: Key Epigenetic Mechanisms and Their Alterations in Aging
| Epigenetic Mechanism | Key Components | Age-Related Alterations | Functional Consequences |
|---|---|---|---|
| DNA Methylation | DNMT1, DNMT3A/B, TET enzymes, CpG islands | Global hypomethylation, focal hypermethylation at promoter CpG islands [112] [113] | Genomic instability, silencing of tumor suppressor genes, altered stem cell function [112] |
| Histone Modifications | Histone acetyltransferases (HATs), Histone deacetylases (HDACs), methyltransferases | Loss of histones, altered acetylation/methylation marks (e.g., reduced H3/H4 acetylation) [113] | Changes in chromatin structure, dysregulated gene expression, cellular senescence [113] |
| Chromatin Remodeling | Chromatin-associated complexes, non-coding RNAs | Altered nucleosome positioning, loss of heterochromatin [113] | Increased transcriptional noise, activation of transposable elements |
The Aging Gut Microbiome and 'Inflammaging'
The gut microbiome undergoes profound changes with age, a process termed "biome-aging" [116]. In healthy aging, microbial diversity is maintained or even increases, with a characteristic shift in composition: a decrease in dominant taxa like Bacteroides and an increase in less prevalent groups such as Clostridia and health-associated genera like Akkermansia and Christensenellaceae [117] [116]. Conversely, unhealthy aging is marked by a loss of diversity and a rise in pro-inflammatory pathobionts [117]. These shifts are driven by factors including diet, polypharmacy, and physiological decline of the gastrointestinal tract [116].
A primary consequence of these microbial changes is their contribution to inflammaging—a state of chronic, low-grade, systemic inflammation that is a hallmark of aging [117] [116]. Several microbiome-related mechanisms fuel this process:
- Leaky Gut and Barrier Dysfunction: A decline in beneficial, short-chain fatty acid (SCFA)-producing bacteria (e.g., Faecalibacterium, Roseburia) and an increase in mucin-degraders can compromise intestinal barrier integrity [22] [117]. This "leaky gut" allows bacterial components like lipopolysaccharide (LPS) to translocate into circulation, triggering innate immune responses and systemic inflammation [116].
- Loss of Anti-inflammatory Metabolites: SCFAs (e.g., butyrate, propionate, acetate), produced by microbial fermentation of dietary fiber, are crucial for maintaining immune homeostasis. They inhibit NF-κB signaling, promote regulatory T-cell function, and strengthen the gut barrier [117] [116]. The age-related decline in SCFA producers thus directly contributes to a pro-inflammatory state.
- Expansion of Pro-inflammatory Taxa: An aging-related gut environment can favor the bloom of microbes that thrive in inflammatory conditions or directly provoke immune activation [117].
Table 2: Microbial Signatures and Metabolites in Healthy vs. Unhealthy Aging
| Aspect | Healthy Aging / Longevity | Unhealthy Aging |
|---|---|---|
| Alpha-diversity | Higher, more stable [117] | Lower, less stable [117] |
| Key Bacterial Taxa | Higher abundance of Akkermansia, Christensenellaceae, Bifidobacterium, Oscillospira [117] [116] | Higher abundance of pro-inflammatory pathobionts (e.g., Escherichia, Klebsiella); loss of SCFA producers [117] |
| Microbial Metabolites | Higher levels of SCFAs (butyrate, propionate); unique beneficial secondary bile acids [117] [116] | Reduced SCFA levels; dysregulated secondary bile acid profiles (e.g., deoxycholic acid) [116] |
| Systemic Impact | Reduced inflammaging, better metabolic and cognitive health [116] | Elevated inflammaging, increased risk of age-related diseases [117] [116] |
Mechanistic Links: How Gut Microbiota Regulate the Host Epigenome
The gut microbiome influences the host epigenome through multiple, interconnected pathways, primarily mediated by microbial metabolites. The diagram below illustrates the core signaling pathways linking microbial metabolites to host epigenetic regulation and inflammaging.
Figure 1: Microbial Metabolite Pathways to Host Epigenome and Inflammaging. SCFAs act as HDAC inhibitors, while other metabolites signal via nuclear receptors. LPS promotes inflammation via TLR4. BA = Bile Acid; FXR = Farnesoid X Receptor; TGR5 = Takeda G-protein receptor 5; HDACi = Histone Deacetylase Inhibitor; HAT = Histone Acetyltransferase.
Microbial Metabolites as Epigenetic Regulators
- Short-Chain Fatty Acids (SCFAs): Butyrate, propionate, and acetate are potent histone deacetylase inhibitors (HDACi) [114]. By inhibiting HDACs, SCFAs lead to an accumulation of acetyl groups on histones, particularly in immune and epithelial cells, promoting an open chromatin state and activating genes involved in anti-inflammatory pathways, barrier integrity, and immune tolerance [117] [114]. Butyrate is also a ligand for certain G-protein-coupled receptors (GPCRs), which can trigger signaling cascades that influence gene expression.
- Bile Acids (BAs): Gut microbes metabolize primary bile acids into secondary bile acids. These secondary BAs, such as lithocholic acid, can act as signaling molecules through host nuclear receptors like the Farnesoid X Receptor (FXR) and GPCRs (TGR5) [116]. This signaling can modulate the expression of genes involved in metabolism and inflammation and has been linked to downstream epigenetic effects, including alterations in DNA methylation and histone modifications [116] [114].
- Other Metabolites: Microbial metabolites such as folate, a key methyl donor, and trimethylamine-N-oxide (TMAO), implicated in cardiovascular disease, can also influence epigenetic pathways by modulating the availability of substrates for DNA and histone methylation [114].
Direct Evidence from Association Studies
Emerging large-scale human studies directly link the gut microbiome to host epigenetic states. A discovery and replication Epigenome-Wide Association Study (EWAS) in Dutch cohorts identified specific CpG sites in blood DNA whose methylation status was significantly associated with the abundance of the gut bacterium Eggerthella [65]. For instance, methylation at site cg16586104 was positively correlated with Eggerthella abundance, while cg12234533 was negatively correlated [65]. This study also demonstrated that the gut microbiome can mediate the effect of environmental factors, such as diet and medication, on host DNA methylation, providing a mechanistic link between exposome, microbiome, and epigenome [65].
Experimental and Analytical Methodologies
To investigate the microbiome-epigenome axis, researchers employ a suite of advanced technologies. The following workflow outlines a typical integrated multi-omics approach.
Figure 2: Integrated Multi-omics Workflow. A typical pipeline from sample collection to data integration for studying microbiome-epigenome interactions.
Profiling the Microbiome and Epigenome
- Microbiome Profiling:
- 16S rRNA Gene Sequencing: A cost-effective method to profile microbial community composition and diversity by sequencing the hypervariable regions of the 16S ribosomal RNA gene. It provides taxonomic information at the genus level [115] [65].
- Shotgun Metagenomic Sequencing: Sequences all the genetic material in a sample, allowing for species- and strain-level identification and functional inference of microbial communities, including analysis of metabolic pathways [115] [65].
- Epigenome Profiling:
- Methylation Arrays: Platforms like the Illumina Infinium MethylationEPIC (850k) array provide a high-throughput method to assess the methylation status of over 850,000 CpG sites across the genome at single-nucleotide resolution [65].
- Whole-Genome Bisulfite Sequencing (WGBS): The gold standard for DNA methylation analysis, providing base-pair resolution methylation levels for every cytosine in the genome, though more expensive and computationally intensive than arrays [112].
Establishing Causality and Mediation
- Mendelian Randomization (MR): A statistical method that uses genetic variants as instrumental variables to infer causal relationships between an exposure (e.g., gut microbiota) and an outcome (e.g., epigenetic age acceleration or age-related disease) [118]. This approach helps mitigate confounding and reverse causation biases inherent in observational studies.
- Mediation Analysis: A statistical framework used to dissect whether the effect of an exposure (e.g., a specific gut microbe) on an outcome (e.g., heart failure) is mediated by a third variable (e.g., an aging indicator like the frailty index) [118]. This has been used to show that the causal effects of gut microbiota on some age-related diseases are partially mediated by aging indicators [118].
Functional Validation in Model Systems
- Gnotobiotic Models: Germ-free mice colonized with specific bacterial strains or defined microbial communities allow researchers to directly test the causal impact of microbes on the host epigenome and aging phenotype [117].
- Fecal Microbiota Transplantation (FMT): Transferring gut microbiota from old donors to young recipients, and vice versa, in animal models has demonstrated that the aged microbiome can promote inflammaging and cognitive decline, while a young microbiome can rejuvenate aged systems [117]. This provides powerful evidence for the functional role of the microbiome in aging.
Table 3: The Scientist's Toolkit: Key Reagents and Models for Microbiome-Epigenome Research
| Category | Item/Model | Key Function/Application |
|---|---|---|
| Sequencing & Profiling | Illumina MiSeq/HiSeq for 16S rRNA sequencing | Taxonomic profiling of microbial communities [115] |
| Illumina NovaSeq for shotgun metagenomics | Comprehensive functional and taxonomic profiling [115] [65] | |
| Illumina Infinium MethylationEPIC BeadChip | High-throughput DNA methylation analysis of >850,000 CpG sites [65] | |
| Experimental Models | Germ-free (Gnotobiotic) mice | Establishing causality by colonizing with specific microbes [117] |
| Fecal Microbiota Transplantation (FMT) | Testing functional effects of whole microbial communities [117] | |
| Chemical Reagents | Sodium butyrate / other SCFAs | Direct application of microbial metabolites to test epigenetic effects (e.g., HDAC inhibition) [114] |
| HDAC inhibitors (e.g., Trichostatin A) | Pharmacological tools to mimic SCFA epigenetic action [112] | |
| Bioinformatic Tools | QIIME 2, MOTHUR (16S data analysis) | Processing and analyzing 16S rRNA sequencing data [115] |
| SeSAMe, Minfi (Methylation array analysis) | Processing and normalizing DNA methylation array data [65] | |
| MendelianRandomization, TwoSampleMR (R packages) | Performing MR analysis to infer causality from GWAS data [118] |
Diagnostic and Therapeutic Implications
The intricate link between the gut microbiome and the host epigenome opens novel avenues for promoting healthy aging.
Biomarker Discovery
The integration of microbiome and epigenomic data holds promise for developing sophisticated biomarkers. Machine learning models have shown that gut microbiota identified through genetic correlation and causal relationship analyses can serve as biomarkers for disease prediction, enhancing the performance of predictive models (average AUC increased from 0.808 to 0.832 in one study) [118]. Furthermore, the uniqueness of an individual's gut microbiome, which increases with age, has been associated with immune regulation and longevity, and a low uniqueness measure in the very old (>85 years) is linked to decreased survival [115].
Microbiome-Targeted Interventions
- Dietary Interventions: The Mediterranean diet, rich in fiber and polyphenols, has been shown to enrich SCFA-producing bacteria, reduce inflammatory markers, and improve cognitive function in the elderly [117]. Diet is a primary lever for shaping the gut ecosystem.
- Prebiotics and Probiotics: Targeted formulations of prebiotics (substances that promote beneficial microbes) and probiotics (live beneficial bacteria) are under investigation. For example, Akkermansia muciniphila and Bifidobacterium strains are being explored for their ability to improve barrier function and reduce inflammation [116]. "Postbiotics" (inanimate microbial cells and/or their components) are also emerging as stable therapeutic options; for instance, a Lactobacillus paracasei postbiotic was shown to promote mucus formation, reduce gut permeability, and improve cognitive and metabolic function in aged mice [117].
- Fecal Microbiota Transplantation (FMT): While clinically established for C. difficile infection, FMT from young donors is being explored preclinically for aging. However, creating a "young" microbiome in an old host may lead to functional mismatches, suggesting a need for more nuanced approaches than simple reversion [117].
- Epigenetic Drugs: Small molecules that target epigenetic enzymes, such as HDAC inhibitors and DNMT inhibitors, are in clinical use for oncology and are being investigated for aging-related diseases [112]. The discovery that microbial metabolites like butyrate are natural HDACi underscores the potential to harness or mimic microbial strategies for epigenetic rejuvenation [112] [114].
The evidence is compelling: the gut microbiome serves as a master epigenetic effector of aging, translating environmental and lifestyle cues into programmable changes in the host genome that drive inflammaging and functional decline. The "holoepigenome" — the integrated epigenetic landscape of the host and its microbiota — represents a fundamental regulatory layer of the aging process. Future research must focus on longitudinal human studies to track microbiome-epigenome dynamics across the lifespan, leveraging single-cell multi-omics to achieve cellular resolution. A major challenge and opportunity lie in moving from associations to mechanism, by comprehensively characterizing the vast repertoire of unknown microbial metabolites and defining their specific epigenetic targets and functions in the host. The translation of this knowledge into safe, effective, and personalized microbiome-based therapeutics — whether live biotherapeutics, postbiotics, or epigenetic drugs inspired by microbial chemistry — holds the key to mitigating inflammaging and extending human healthspan.
Abstract The gut microbiome exerts a profound influence on host physiology, largely through its role in modulating the host epigenome. This whitepaper provides a comparative analysis of three primary microbiome-targeted interventions—probiotics, prebiotics, and fecal microbiota transplantation (FMT)—evaluating their efficacy across conditions like irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and metabolic disorders. By integrating quantitative data, detailed experimental protocols, and visualizations of mechanistic pathways, this document serves as a technical guide for researchers and drug development professionals working at the intersection of microbial therapeutics and epigenomic reprogramming.
The human gut microbiome, a complex consortium of microorganisms, is now recognized as a key regulator of the host epigenome. This dynamic interaction allows environmental factors, including microbial metabolites, to shape host gene expression without altering the underlying DNA sequence [119] [2]. Major epigenetic mechanisms such as DNA methylation, histone modifications, and non-coding RNA activity are directly influenced by the gut microbiota [120] [11]. For instance, microbial metabolites like short-chain fatty acids (SCFAs) and folate act as substrates and enzymatic regulators for host epigenetic machinery, thereby influencing fundamental processes in immunity, metabolism, and cellular differentiation [120] [2]. Dysbiosis, or microbial imbalance, can disrupt this delicate interplay, leading to aberrant epigenetic patterns associated with a range of chronic diseases [11]. Consequently, interventions designed to modulate the gut microbiome represent a promising frontier for correcting these epigenetic dysregulations and advancing therapeutic development.
Comparative Efficacy Analysis of Interventions
Direct comparative evidence for these interventions is most robust for Irritable Bowel Syndrome (IBS), as demonstrated by a comprehensive network meta-analysis [121] [122]. The following tables summarize the efficacy data and postulated epigenetic mechanisms for each intervention.
Table 1: Comparative Efficacy of Microbiome-Targeted Interventions in IBS (Based on Network Meta-Analysis)
| Intervention | Odds Ratio (OR) for Symptom Improvement (95% CI) | Number of RCTs Included | Key Efficacy Findings |
|---|---|---|---|
| Fecal Microbiota Transplantation (FMT) | 0.46 (0.33 - 0.64) [121] | 6 | Superior to placebo; comparable or superior to probiotics [121] [123] |
| Probiotics | 0.53 (0.48 - 0.59) [121] | 54 | Effective vs. placebo; efficacy strain-dependent (e.g., Bifidobacterium, Lactobacillus) [121] |
| Prebiotics/Synbiotics | Not Significant [121] | 7 | Did not show significant improvement over placebo [121] |
Table 2: Postulated Epigenetic Mechanisms of Microbiome-Targeted Interventions
| Intervention | Key Biological Effects | Putative Epigenetic Mechanisms |
|---|---|---|
| FMT | Restores microbial diversity; increases SCFA production; improves gut barrier function [124] [123] | Donor microbiota may induce host DNA hypomethylation in intestinal epithelial cells; SCFAs (butyrate) inhibit HDACs [120] [11] |
| Probiotics | Modulates host immune response; competitively excludes pathogens; may produce SCFAs and folate [121] [11] | Specific strains (e.g., L. acidophilus) can induce differential DNA methylation; microbial folate donates methyl groups for DNA/histone methylation [120] [11] |
| Prebiotics | Serves as fermentable substrate for beneficial gut bacteria | Indirect effects via boosting endogenous SCFA-producing bacteria; SCFAs act as HDAC inhibitors [120] |
Route of Administration and Enhanced FMT
Emerging research focuses on optimizing FMT delivery. A recent double-blind RCT demonstrated that both encapsulated FMT and FMT via rectal enema were significantly more effective than placebo in improving IBS symptoms and quality of life, with no serious adverse events [123]. Furthermore, innovative strategies such as probiotic-modified FMT (MFMT) are being developed. Pre-treatment of donor microbiota with Lactobacillus plantarum GR-4 enhanced its resilience, increased production of immunomodulatory metabolites, and resulted in an 83% remission rate in a murine colitis model, compared to 50% with conventional FMT [124].
Detailed Experimental Protocols
To ensure reproducibility and rigor in this field, below are detailed methodologies for key experiments cited in this analysis.
This protocol outlines a double-blind, randomized, placebo-controlled trial comparing encapsulated FMT and FMT via rectal enema.
1. Study Population & Design:
- Participants: Adults (18-70 years) meeting Rome IV criteria for IBS.
- Groups: Randomized 1:1:1 to Encapsulated FMT, FMT enema, or Placebo.
- Blinding: Double-blind, with randomization sequence concealed from patients and investigators.
2. Donor Screening & Stool Preparation:
- Donor Criteria: Healthy donor (24-year-old female in the cited study) screened via comprehensive questionnaire, physical exam, and blood/stool tests to exclude communicable diseases, metabolic syndrome, and gastrointestinal disorders.
- Blood Tests: HIV, Treponema pallidum, Hepatitis A, B, C.
- Stool Tests: Clostridioides difficile (GDH, toxin A/B immunoassay, PCR), enteric pathogens, viruses, and parasites.
- Preparation: 50 grams of donor stool is processed. For enema, it is mixed with 200 mL isotonic saline and filtered. For capsules, it is frozen at -80°C. Placebo enema uses 200 mL saline; placebo capsules use an inert substance.
3. Intervention & Follow-up:
- Encapsulated FMT Group: Receives 6 capsules twice daily for two consecutive days (total 50g stool).
- FMT Enema Group: Receives a single 50g stool enema in 200 mL saline.
- Placebo Group: Receives identical placebo capsules or enema.
- Primary Endpoint: Clinical response (≥50-point decrease in IBS-Symptom Severity Score) at 4 weeks.
- Secondary Endpoints: Quality of life (IBS-QoL), adverse events, and changes in fecal microbiota composition.
This protocol describes the generation and evaluation of probiotic-enhanced FMT in a preclinical setting.
1. Donor Microbiota Modification:
- Probiotic Preconditioning: Donor mice are administered Lactobacillus plantarum GR-4 for 3 weeks via oral gavage to generate a modified microbiota.
- Microbiota Collection: Fresh fecal matter is collected from preconditioned donors.
2. Induction of Colitis & Intervention:
- DSS Colitis Model: Mice are given dextran sulfate sodium (DSS) in drinking water to induce inflammatory bowel disease.
- Treatment Groups: Colitis-induced mice are treated with:
- Modified FMT (MFMT) from GR-4-preconditioned donors.
- Conventional FMT (FMT) from untreated donors.
- 5-aminosalicylic acid (5-ASA) as a standard therapy control.
- FMT Administration: Fecal matter is transplanted into recipient mice via oral gavage.
3. Outcome Assessment:
- Disease Activity: Monitoring of body weight, colon length, and histological scoring.
- Multi-omics Analysis: 16S rRNA sequencing for microbial composition; metabolomics (e.g., SCFAs, indoles) from cecal contents.
- Functional Assays: Engraftment efficiency of donor microbiota; stress resistance to bile/gastric conditions in vitro; measurement of inflammatory cytokines and gut barrier integrity.
Signaling Pathways and Mechanistic Workflows
The following diagrams, generated using Graphviz DOT language, illustrate the core mechanistic pathways and experimental workflows discussed.
Microbial Modulation of Host Epigenome
This diagram outlines the primary mechanisms by which gut microbiota and their metabolites influence the host epigenome.
FMT Clinical Trial Workflow
This diagram visualizes the workflow of a typical FMT clinical trial, as described in the protocol section.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and materials essential for conducting research in microbiome-epigenome interactions and intervention studies.
Table 3: Key Research Reagent Solutions
| Reagent / Material | Function / Application | Example Usage in Context |
|---|---|---|
| 16S rRNA Sequencing Reagents | Profiling microbial community composition and diversity. | Assessing donor and recipient microbiota changes pre- and post-FMT [124] [123]. |
| DNA Methylation Kits (e.g., for bisulfite conversion) | Detecting and quantifying 5-methylcytosine (5mC) in host DNA. | Analyzing microbiota-induced DNA hypomethylation in intestinal epithelial cells [120] [11]. |
| HDAC Activity Assay Kits | Quantifying histone deacetylase activity. | Measuring functional inhibition of HDAC by microbial SCFAs like butyrate [120] [2]. |
| Cytokine ELISA/Kits | Quantifying inflammatory mediators (e.g., IL-10, IL-22, TNF-α). | Evaluating anti-inflammatory effects of interventions in colitis models or human trials [122] [124]. |
| Germ-Free (GF) Mice | Studying host-microbe interactions in a controlled, microbiota-free environment. | Establishing causal links between specific microbes/metabolites and host epigenetic changes [120] [11]. |
| SCFA Standards (Butyrate, Propionate, Acetate) | Metabolomic analysis; used as reference standards in LC-MS/GC-MS. | Quantifying changes in beneficial microbial metabolite production after intervention [124]. |
The comparative analysis underscores that FMT and specific probiotics currently hold the most compelling evidence for efficacy in managing conditions like IBS, likely through robust modulation of the gut ecosystem and consequent epigenetic effects. In contrast, the evidence for prebiotics and synbiotics remains limited. The future of this field lies in precision modulation, moving beyond broad interventions towards engineered microbial consortia and optimized protocols like probiotic-enhanced FMT. For drug development, targeting the pathways that connect microbial metabolites to the host epigenome offers a promising strategy for novel therapeutics. Advancing this frontier will require a concerted effort, integrating deep multi-omics profiling, sophisticated animal models, and rigorously designed clinical trials to fully harness the therapeutic potential of the gut microbiome-epigenome axis.
Epigenetic clocks are powerful computational models that predict biological age based on DNA methylation (DNAm) patterns at specific cytosine-guanine dinucleotide (CpG) sites across the genome. These clocks have emerged as some of the most accurate tools for quantifying biological aging, reflecting the cumulative burden of environmental, genetic, and lifestyle influences on an organism's functional status. Unlike chronological age, which simply measures time elapsed since birth, epigenetic age captures biological decline and has proven to be a robust predictor of mortality, age-related functional decline, and disease susceptibility [125]. The construction of these clocks typically involves selecting a panel of CpG sites whose methylation status correlates strongly with chronological age across populations, using machine learning techniques such as elastic net regression to create a predictive algorithm [126].
The significance of epigenetic clocks extends far beyond mere age prediction. These biomarkers provide critical insights into the biological aging process itself, capturing information about the integrity of multiple organ systems and physiological resilience. The deviation between epigenetic age and chronological age, known as epigenetic age acceleration (EAA), represents a particularly valuable metric. Positive EAA (where epigenetic age exceeds chronological age) indicates accelerated biological aging and is associated with increased risk for numerous age-related conditions, including cardiovascular disease, neurodegenerative disorders, and all-cause mortality [127] [128]. The development of these clocks has evolved through generations, from first-generation clocks (e.g., Horvath, Hannum) trained primarily on chronological age, to second-generation clocks (e.g., PhenoAge, GrimAge) that incorporate clinical parameters and mortality data to better capture age-related physiological decline [126].
Table 1: Generations of Epigenetic Clocks and Their Characteristics
| Generation | Representative Clocks | Training Basis | Key Applications |
|---|---|---|---|
| First-Generation | Horvath's multi-tissue clock, Hannum clock | Chronological age | Multi-tissue age estimation, blood-based age prediction |
| Second-Generation | PhenoAge, GrimAge | Clinical biomarkers, mortality data | Disease risk prediction, mortality risk assessment |
| Domain-Specific | Intrinsic Capacity (IC) clock | Composite functional capacity | Functional decline monitoring, healthspan assessment |
The Gut Microbiome as a Regulator of Host Epigenomic Landscapes
The human gut microbiome constitutes a dynamic ecosystem of microorganisms that profoundly influences host physiology through multiple molecular pathways. A rapidly expanding body of evidence indicates that gut microbiota play a pivotal role in shaping host epigenetic programming, thereby serving as a crucial interface between environmental exposures (particularly diet) and gene expression regulation. This microbiome-epigenome crosstalk represents a fundamental mechanism through which gut microbes influence host health, disease risk, and aging processes [53] [1]. The gut microbiome's composition and function are influenced by numerous factors including diet, stress, medications, and aging itself, creating a complex feedback loop that can either promote health or drive disease processes [9].
The molecular mechanisms through which gut microbiota influence host DNA methylation patterns are multifaceted and involve several key pathways:
- Short-chain fatty acid (SCFA) signaling: Microbial fermentation of dietary fiber produces SCFAs such as butyrate, propionate, and acetate, which serve as histone deacetylase inhibitors and influence DNA methyltransferase activity [53] [1].
- One-carbon metabolism regulation: Gut microbes contribute essential metabolites for folate-mediated one-carbon metabolism, which provides methyl groups for DNA methylation reactions [53].
- Polyamine biosynthesis: Specific microbial species produce polyamines that can modulate DNA methylation patterns [1].
- Extracellular vesicle-mediated communication: Gut bacteria release membrane-derived vesicles containing microbial DNA, RNA, and proteins that can influence host epigenetic regulation [53].
This microbiome-epigenome axis has significant implications for understanding how modifiable factors like diet can influence biological aging. Dietary patterns directly shape the gut microbial community, which in turn produces metabolites that either promote healthy epigenetic patterns or contribute to aberrant methylation signatures associated with age-related diseases [129]. The bidirectional nature of this relationship means that while gut microbes influence host epigenetics, host epigenetic states also create selective pressures that shape microbial composition, establishing a continuous dialogue between host and microbiome throughout the lifespan [53].
Diagram 1: Microbiome-Epigenome Bidirectional Crosstalk
Methodological Approaches for Epigenetic Clock Development and Validation
Core Technical Workflow
The development of robust epigenetic clocks follows a rigorous methodological pipeline that combines molecular biology techniques with sophisticated computational approaches. The initial phase involves DNA methylation profiling using microarray technologies, predominantly the Illumina Infinium EPIC array, whichinterrogates methylation status at over 850,000 CpG sites across the genome [126]. For studies requiring higher resolution, whole-genome bisulfite sequencing provides base-pair resolution methylation data but at substantially higher cost and computational burden. The selection of appropriate biological samples is critical, with peripheral blood being the most common source due to its accessibility, though clocks have been successfully developed using saliva, buccal cells, and various solid tissues [126].
The analytical workflow for clock development typically involves several stages. After quality control and normalization of methylation data, feature selection identifies CpG sites most predictive of the target phenotype (e.g., chronological age, clinical parameters, or functional capacity). Machine learning algorithms, particularly elastic net regression, are then employed to construct the predictive model by assigning weights to each selected CpG site [126]. This approach balances model complexity with predictive accuracy by applying penalties that minimize overfitting. The resulting clock algorithm generates a DNAm age estimate that can be compared to chronological age to calculate epigenetic age acceleration.
Validation and Refinement
Rigorous validation is essential to establish the clinical and biological relevance of epigenetic clocks. This process typically involves cross-validation within the discovery cohort followed by external validation in independent populations [126]. Longitudinal studies are particularly valuable for establishing the predictive capacity of clocks for future health outcomes. For example, the intrinsic capacity (IC) clock was validated in the Framingham Heart Study, where it demonstrated superior performance in predicting all-cause mortality compared to earlier epigenetic clocks [126]. Additional validation approaches include assessing associations with age-related clinical phenotypes, functional measures, and established biomarkers of aging.
Table 2: Key Methodological Steps in Epigenetic Clock Development
| Stage | Key Procedures | Considerations |
|---|---|---|
| Sample Collection | Blood, saliva, or tissue sampling; DNA extraction | Sample stability, ethical approval, population diversity |
| Methylation Profiling | Illumina Infinium array processing; bisulfite conversion | Batch effects, quality control, normalization methods |
| Data Preprocessing | Background correction, probe filtering, normalization | Handling of cross-reactive and polymorphic probes |
| Model Training | Feature selection; elastic net regression with k-fold cross-validation | Overfitting prevention, parameter tuning, variance explained |
| Validation | External cohort testing; association with clinical outcomes | Generalizability, ethnic specificity, tissue specificity |
Diagram 2: Epigenetic Clock Development Workflow
Experimental Evidence Linking Gut Microbiota to Epigenetic Aging
Causal Relationships Revealed by Mendelian Randomization
Advanced genetic epidemiological approaches have provided compelling evidence for causal relationships between specific gut microbial taxa and epigenetic aging. A bi-directional Mendelian randomization study published in 2024 analyzed genetic instruments for gut microbiota from the MiBioGen consortium and the Dutch Microbiome Project alongside epigenetic age acceleration data from genome-wide association studies [127]. This approach identified several bacterial taxa with potential causal effects on GrimAge acceleration, a robust predictor of mortality. Specifically, species Holdemania unclassified demonstrated a strong positive association with GrimAge acceleration (OR: 1.31, 95% CI: 1.13-1.52, P = 0.0004), suggesting it may promote biological aging [127]. Conversely, Family Acidaminococcaceae (OR: 0.64, 95% CI: 0.44-0.93, P = 0.019) and Family Clostridiaceae1 (OR: 0.69, 95% CI: 0.49-0.97, P = 0.031) showed negative associations with GrimAge acceleration, indicating potential protective effects against biological aging [127].
The reverse Mendelian randomization analysis in the same study revealed that epigenetic age acceleration can conversely influence microbial composition, demonstrating the bidirectional nature of this relationship. PhenoAge acceleration showed a strong inverse association with genus Turicibacter (OR: 0.928, 95% CI: 0.888-0.971, P < 0.001), suggesting that accelerated biological aging creates an intestinal environment less favorable for this bacterium [127]. These findings provide genetic evidence supporting the complex interrelationship between gut microbial ecology and host biological aging processes, with implications for developing microbiota-targeted interventions to promote healthy aging.
Microbial Influence on Organ-Specific Aging
The gut microbiome's influence on epigenetic aging extends beyond systemic measures to organ-specific aging processes, particularly brain aging. Research indicates that peripheral epigenetic biomarkers can track brain health and disease, with specific epigenetic scores (EpiScores) showing association with cognitive function, brain MRI measures, and dementia risk [125]. The gut microbiome appears to mediate these relationships through multiple pathways, including the production of neuroactive metabolites that influence epigenetic regulation in neural tissues. Microbiota-derived short-chain fatty acids, for instance, can cross the blood-brain barrier and influence histone acetylation and DNA methylation patterns in brain regions critical for cognitive function [53].
The relationship between gut microbiota and neurological aging is further supported by studies showing that fecal microbiota transplantation from aged mice to young recipients increases intestinal inflammation and accelerates age-related phenotypes [127]. Conversely, transplantation from healthy aging mice can improve gut barrier function and enhance cognitive function, suggesting that specific microbial configurations can either promote or protect against neurocognitive decline [127]. These findings highlight the potential for microbiome-based interventions to modulate brain aging and reduce the risk of age-related neurodegenerative conditions.
Applications in Disease Prediction and Clinical Translation
Predicting Neurological and Cardiovascular Outcomes
Epigenetic clocks have demonstrated remarkable utility in predicting incident neurological and cardiovascular diseases, providing valuable tools for risk stratification and early intervention. A comprehensive meta-analysis published in 2025 synthesized evidence from 13 studies examining the relationship between epigenetic age acceleration and stroke risk [128]. The analysis revealed a significant positive association between accelerated biological aging and stroke risk (OR = 1.16, 95% CI 1.13-1.19, p < 0.001), with even stronger associations observed for incident stroke (OR = 1.28, 95% CI 1.25-1.35) compared to stroke recurrence (OR = 1.11, 95% CI 1.06-1.16) [128]. These findings suggest that epigenetic clocks capture aspects of biological aging that contribute to initial cerebrovascular events independent of traditional risk factors.
In the realm of neuropsychiatric conditions, recent research has explored the interrelationships between gut microbiota, epigenetic changes, and conditions such as anorexia nervosa (AN), obesity, and depression [22]. These disorders share disturbances in the microbial and epigenetic regulation of stress, mood, and behavior via the gut-brain axis, though the specific patterns of microbial and epigenetic alteration vary between conditions [22]. For example, patients with AN typically show decreased abundance of butyrate-producing genera (e.g., Faecalibacterium and Roseburia) and increased levels of mucin-degrading species (e.g., Akkermansia) [22]. These microbial shifts may influence epigenetic regulation of genes involved in appetite, body weight, and mood, contributing to disease persistence.
The Intrinsic Capacity Clock and Functional Aging
A significant recent advancement in the field is the development of the intrinsic capacity (IC) clock, a DNA methylation-based predictor trained on clinical evaluations of cognition, locomotion, psychological well-being, sensory abilities, and vitality [126]. This clock represents a paradigm shift from disease-focused to function-focused biomarkers of aging. When applied to the Framingham Heart Study, the DNAm IC outperformed first-generation and second-generation epigenetic clocks in predicting all-cause mortality and showed strong associations with immune and inflammatory biomarkers, functional endpoints, and lifestyle factors [126].
The IC clock demonstrates particularly strong associations with immune aging pathways. Differential expression analysis revealed that higher DNAm IC (indicating better functional capacity) was strongly associated with increased expression of CD28 (FDR = 1.07 × 10^(-32)), a critical T cell costimulatory molecule whose loss represents a hallmark of immunosenescence [126]. Conversely, poor IC clock levels tracked with elevated expression of CDK14/PFTK1 (FDR = 2.77 × 10^(-29)), a proinflammatory mediator associated with Parkinson's disease and several cancers [126]. These molecular signatures connect epigenetic measures of functional capacity with fundamental immunological aging processes, providing insights into the biological mechanisms underlying age-related functional decline.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents and Platforms for Microbiome-Epigenome Studies
| Category | Specific Reagents/Platforms | Research Applications |
|---|---|---|
| DNA Methylation Profiling | Illumina Infinium EPIC BeadChip (~850,000 CpGs); Whole-genome bisulfite sequencing | Genome-wide methylation analysis; Base-resolution methylome mapping |
| Microbiome Analysis | 16S rRNA gene sequencing (V3-V4 region); Shotgun metagenomics | Microbial community profiling; Functional gene content analysis |
| Bioinformatic Tools | Minfi (R package for methylation analysis); QIIME 2 (microbiome analysis); EWAS algorithms | Data preprocessing; Differential abundance testing; Epigenome-wide association studies |
| Cell Culture Models | Caco-2 intestinal epithelial cells; HT-29 cells; Organoid culture systems | In vitro mechanistic studies of microbial metabolites on host epigenetics |
| Animal Models | Germ-free mice; Gnotobiotic models; Humanized microbiome mice | Causal studies of specific microbial communities on host epigenetic aging |
Future Directions and Therapeutic Implications
The converging fields of microbiome research and epigenetics hold tremendous promise for developing novel interventions to promote healthy aging and prevent age-related diseases. Several translational frontiers are emerging, including biomarker discovery, live biotherapeutic interventions, fecal microbiota transplantation, and adaptive clinical trial designs [53] [1]. The integration of high-throughput methylation mapping, artificial intelligence, and single-cell multi-omics is accelerating our ability to model complex host-microbiome interactions at unprecedented resolution [9]. These technological advances are paving the way for precision medicine approaches that leverage individual-specific microbial and epigenetic profiles to tailor interventions.
Future research priorities include elucidating the precise molecular mechanisms through which specific microbial metabolites influence host epigenetic machinery, particularly in tissue-specific contexts. Additionally, longitudinal studies tracking parallel changes in gut microbiota composition and epigenetic patterns throughout the lifespan will be essential for establishing causal relationships and identifying critical windows for intervention. The development of standardized methodologies and ethical frameworks for data governance, such as the FAIR and CARE principles, will be crucial for ensuring equitable translation of these discoveries into clinical practice [53]. As evidence accumulates linking modifiable lifestyle factors to both microbial ecology and epigenetic aging, we move closer to realizing the vision of personalized strategies for extending healthspan through targeted modulation of the microbiome-epigenome axis.
Conclusion
The evidence unequivocally establishes the gut microbiome as a potent epigenetic effector, influencing host gene expression through conserved molecular pathways. The bidirectional 'epigenome-microbiome axis' represents a fundamental regulatory layer in physiology and disease pathogenesis. Future research must prioritize elucidating causal mechanisms through advanced engineering tools, standardizing methodologies to enable robust cross-study comparisons, and rigorously testing targeted interventions like next-generation live biotherapeutics in clinical trials. The integration of microbiome and epigenome profiling holds immense promise for developing personalized diagnostic biomarkers and therapeutic strategies, ultimately paving the way for a new paradigm in precision medicine that leverages our microbial partners to maintain health and treat disease.
References
- 1. The Gut Microbiome and Epigenomic Reprogramming - PubMed [https://pubmed.ncbi.nlm.nih.gov/40943575/]
- 2. The Gut Microbiome and Epigenomic Reprogramming [https://www.mdpi.com/1422-0067/26/17/8658]
- 3. Unraveling host regulation of gut microbiota through the ... [https://pubmed.ncbi.nlm.nih.gov/38839511/]
- 4. Microbiota-derived metabolites in the epigenetic regulation ... [https://www.sciencedirect.com/science/article/abs/pii/S2095927325009673]
- 5. Epigenetics in depression and gut-brain axis: A molecular ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2022.1048333/full]
- 6. Emerging methylation-based approaches in microbiome ... [https://biotechnologyforbiofuels.biomedcentral.com/articles/10.1186/s13068-024-02529-x]
- 7. Enhanced visualization of microbiome data in repeated ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2024.1480972/full]
- 8. The microbiota-gut-brain axis: An emerging role for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7016422/]
- 9. Research highlights how the gut microbiome can affect ... [https://www.news-medical.net/news/20250923/Research-highlights-how-the-gut-microbiome-can-affect-epigenetics.aspx]
- 10. The potential of short-chain fatty acid epigenetic regulation ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1380476/full]
- 11. Implications of gut microbiota-mediated epigenetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12143691/]
- 12. Short-chain fatty acids activate acetyltransferase p300 [https://elifesciences.org/articles/72171]
- 13. Short-chain fatty acids in diseases [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-023-01219-9]
- 14. Histone Deacetylase Inhibition and Dietary Short-Chain Fatty ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658706/]
- 15. Inhibition of histone-deacetylase activity by short-chain fatty ... [https://pubmed.ncbi.nlm.nih.gov/18061431/]
- 16. Short-chain fatty acid metabolites propionate and butyrate ... [https://www.nature.com/articles/s42255-024-01191-9]
- 17. Short-chain fatty acid-mediated epigenetic modulation ... [https://pubmed.ncbi.nlm.nih.gov/36566262/]
- 18. Effects of short-chain fatty acids in inhibiting HDAC and ... [https://www.nature.com/articles/s41419-021-03880-9]
- 19. The Role of One-Carbon Metabolism and Methyl Donors in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11084717/]
- 20. One-carbon metabolism and methyl donor nutrition in the ... [https://www.sciencedirect.com/science/article/pii/S002203022030254X]
- 21. Vitamin B-12 and the Gastrointestinal Microbiome [https://pmc.ncbi.nlm.nih.gov/articles/PMC8970816/]
- 22. Exploring the Link Between the Gut Microbiota and Epigenetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12370852/]
- 23. Methylfolate, Folic Acid, Methylcobalamin, and ... [https://askthescientists.com/qa/folic-acid-mthfr-mutations/]
- 24. BioRender: Scientific Image and Illustration Software [https://www.biorender.com/]
- 25. Polyamines at the crossroad between cell metabolism and ... [https://www.nature.com/articles/s41420-025-02573-y]
- 26. Research progress on the microbial metabolism and transport ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11998418/]
- 27. Uncovering de novo polyamine biosynthesis in the gut microbiome and its alteration in inflammatory bowel disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11812404/]
- 28. Connection to Epigenetic Modification of Histones [https://pubmed.ncbi.nlm.nih.gov/41097324/]
- 29. Bacterial extracellular vesicles for gut microbiome–host ... [https://www.sciencedirect.com/science/article/pii/S2211383525001261]
- 30. Gut microbiota-derived extracellular vesicles form a distinct ... [https://pubmed.ncbi.nlm.nih.gov/40298395/]
- 31. A recognition of exosomes as regulators of epigenetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10962328/]
- 32. The Role of Extracellular Vesicles: An Epigenetic View of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4637039/]
- 33. Extracellular vesicles as modifiers of epigenomic profiles [https://pubmed.ncbi.nlm.nih.gov/38845265/]
- 34. Environmental disruption of host–microbe co-adaptation as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4064665/]
- 35. The microbiome extends host evolutionary potential [https://www.nature.com/articles/s41467-021-25315-x]
- 36. Crosstalk between the microbiome and epigenome [https://pmc.ncbi.nlm.nih.gov/articles/PMC5892391/]
- 37. Chemical signaling between gut microbiota and host ... [https://www.sciencedirect.com/science/article/pii/S0021925820427486]
- 38. Chromatin dynamics and histone modifications in intestinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7300386/]
- 39. Impact of the gut microbiome on the genome and epigenome ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-019-0621-2]
- 40. Microbiome and epigenetic variation in wild fish with low ... [https://www.nature.com/articles/s41467-024-49162-8]
- 41. Epigenetics and Gut Microbiota in the Pathogenesis ... [https://pubmed.ncbi.nlm.nih.gov/40710357/]
- 42. Single-cell multi-omic detection of DNA methylation and ... [https://www.nature.com/articles/s41592-025-02847-4]
- 43. Combining mucosal microbiome and host multi-omics data ... [https://www.nature.com/articles/s41467-025-62533-z]
- 44. Ternary-code DNA methylation dynamics: A new era for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534697/]
- 45. High-throughput assessment of FMR1 and SNRPN ... [https://pubmed.ncbi.nlm.nih.gov/40801290/]
- 46. Multi-omic integration of single-cell data uncovers methylation ... [https://epigeneticsandchromatin.biomedcentral.com/articles/10.1186/s13072-025-00619-0]
- 47. a roadmap for DNA methylation biomarkers in liquid biopsies [https://www.nature.com/articles/s41388-025-03624-5]
- 48. Microbial Technologies Enhanced by Artificial Intelligence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11917392/]
- 49. Artificial intelligence and human microbiome: A brief ... [https://www.sciencedirect.com/science/article/pii/S266726852400127X]
- 50. ensuring rigour, reproducibility and relevance in the era of AI [https://www.nature.com/articles/s41575-025-01100-9]
- 51. Metabolic modeling of host-microbe interactions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538087/]
- 52. Metabolic modeling of host-microbe interactions [https://www.sciencedirect.com/science/article/pii/S2001037025004076]
- 53. The Gut Microbiome and Epigenomic Reprogramming [https://pmc.ncbi.nlm.nih.gov/articles/PMC12429217/]
- 54. Gut microbiome, a potential modulator of neuroepigenome [https://www.sciencedirect.com/science/article/abs/pii/S095528632500124X]
- 55. Not quite a cure yet: unlocking the unfulfilled promise of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12626851/]
- 56. Live biotherapeutic product exhibits similar efficacy and ... [https://www.medrxiv.org/content/10.1101/2025.09.08.25335342v1]
- 57. Gut microbiome engineering with probiotics: current trends ... [https://link.springer.com/article/10.1007/s42452-025-07622-w]
- 58. Gut microbiota drives structural variation of exogenous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12068336/]
- 59. Microbiome-active drug delivery systems (MADDS) [https://www.sciencedirect.com/science/article/pii/S0169409X25002054]
- 60. Review Fecal microbiota transplantation in clinical practice [https://www.sciencedirect.com/science/article/pii/S2949928324000087]
- 61. Fecal microbiota transplantation improves bile acid ... [https://pubmed.ncbi.nlm.nih.gov/40890737/]
- 62. Fecal microbiota transplantation-current perspective on ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1523870/full]
- 63. Systematic review of donor and recipient predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9163485/]
- 64. Gut microbiome-derived metabolites and epigenetic ... [https://link.springer.com/article/10.1007/s44337-025-00490-8]
- 65. Linking the gut microbiome to host DNA methylation by a ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-11136-x]
- 66. A Survey of Statistical Methods for Microbiome Data Analysis [https://www.frontiersin.org/journals/applied-mathematics-and-statistics/articles/10.3389/fams.2022.884810/full]
- 67. Unraveling host regulation of gut microbiota through the ... [https://www.sciencedirect.com/science/article/pii/S0966842X24001379]
- 68. Tools for Analysis of the Microbiome - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7598837/]
- 69. Frontiers | Gut microbiota heterogeneity in non-alcoholic fatty liver... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1645298/full]
- 70. Effects of data transformation and model selection on feature ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-024-01996-6]
- 71. Experts chart path to bring microbiome science into routine clinical care [https://www.news-medical.net/news/20250602/Experts-chart-path-to-bring-microbiome-science-into-routine-clinical-care.aspx]
- 72. EMBED: Essential MicroBiomE Dynamics, a dimensionality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10282069/]
- 73. Epigenetic Regulation of Gut Microbial Dysbiosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7877904/]
- 74. The interplay between gut microbiome, epigenetics, and ... [https://www.sciencedirect.com/science/article/abs/pii/S001429992500384X]
- 75. Epigenetic modifications of gut microbiota and their ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1638240/full]
- 76. Gut Microbiota Dysbiosis, Oxidative Stress, Inflammation, ... [https://www.mdpi.com/2076-3921/13/8/985]
- 77. Grand Challenges in Understanding Gut Microbes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8524079/]
- 78. Delivery Mode Affects Stability of Early Infant Gut Microbiota [https://pmc.ncbi.nlm.nih.gov/articles/PMC7762768/]
- 79. Impact of delivery mode-associated gut microbiota ... [https://www.nature.com/articles/s41467-019-13014-7]
- 80. Delivery Mode Affects Stability of Early Infant Gut Microbiota [https://advances.massgeneral.org/obgyn/journal.aspx?id=1876]
- 81. The role of epigenomics in personalized medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5737812/]
- 82. Epigenetics-targeted drugs: current paradigms and future ... [https://www.nature.com/articles/s41392-024-02039-0]
- 83. Advances in drug delivery systems, challenges and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10320272/]
- 84. The Importance of Drug Delivery in the Clinical ... [https://www.mdpi.com/2227-9717/11/10/2919]
- 85. The epigenetic influence of diet-induced gut microbiome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535778/]
- 86. Growing old together: What we know about the influence of ... [https://www.frontiersin.org/journals/sports-and-active-living/articles/10.3389/fspor.2023.1168731/full]
- 87. Maternal Gut Microbiome-Mediated Epigenetic ... [https://www.mdpi.com/2072-6643/16/24/4355]
- 88. Ultra-processed Foods, Weight Gain, and Co-morbidity Risk [https://pmc.ncbi.nlm.nih.gov/articles/PMC8532572/]
- 89. Dietary patterns and accelerated multimorbidity in older ... [https://www.nature.com/articles/s43587-025-00929-8]
- 90. Diet Quality and Epigenetic Aging in the Women's Health ... [https://www.sciencedirect.com/science/article/pii/S2212267224000029]
- 91. Epigenome-wide association study of BMI and waist-to-hip ... [https://www.nature.com/articles/s41598-025-13868-6]
- 92. Age-Adjusted Associations Between Comorbidity and ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2021.584182/full]
- 93. A Scoping Review of Epigenetic Signatures of Diet and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12204033/]
- 94. A roadmap for equitable reuse of public microbiome data [https://www.nature.com/articles/s41564-025-02116-2]
- 95. Findable, Accessible, Interoperable, and Reusable (FAIR) [https://microbiomedata.org/fair/]
- 96. FAIR compliant database development for human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11106358/]
- 97. A blueprint for contemporary studies of microbiomes [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-025-02091-0]
- 98. Epigenetics and the exposome: A new era of disease prevention [https://www.niehs.nih.gov/news/factor/2025/2/feature/4-feature-epigenetics-and-the-exposome]
- 99. From Gut to Heart: Targeting Trimethylamine N-Oxide as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562875/]
- 100. The gut microbiota and cardiovascular : Exploring the role of... disease [https://pubmed.ncbi.nlm.nih.gov/40987375/]
- 101. Gut Microbiota Alterations in Heart Failure Patients [https://www.mdpi.com/2077-0383/14/22/8110]
- 102. The bidirectional regulatory mechanism of gut microbiota ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1710051/full]
- 103. Gut microbiota–derived metabolite trimethylamine N-oxide ... [https://www.sciencedirect.com/science/article/pii/S0021925825023725]
- 104. Frontiers | Editorial: Gut Microbiota-Derived Metabolites and... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1661489/abstract]
- 105. The Microbiota‐Gut‐Brain Connection: A New Horizon in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12411739/]
- 106. Bidirectional crosstalk between the gut microbiota and ... [https://www.nature.com/articles/s41398-025-03504-2]
- 107. Kids with autism show altered gut microbiome-brain ... [https://www.uclahealth.org/news/article/kids-with-autism-gut-microbiome-brain]
- 108. Gut microbiota links to cognitive impairment in bipolar disorder ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12345090/]
- 109. Gut microbiota remodeling and sensory-emotional functional ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07152-4]
- 110. The role of gut microbiota in modulating brain structure and ... [https://www.sciencedirect.com/science/article/pii/S1053811925002952]
- 111. Microbiota-based interventions for autism spectrum disorder [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512243/]
- 112. Epigenetic Regulation of Aging and its Rejuvenation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12402629/]
- 113. Epigenetic regulation of aging: implications for ... [https://www.nature.com/articles/s41392-022-01211-8]
- 114. Epigenetic Mechanisms in Aging: Extrinsic Factors and Gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11675900/]
- 115. Alterations of the gut microbiome are associated with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11019127/]
- 116. Microbiome-based therapeutics towards healthier aging and ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01493-x]
- 117. Aging and the Gut: The Microbiome's Second Act [https://asm.org/articles/2025/july/aging-gut-the-microbiome-second-act]
- 118. Causal Analysis Between Gut Microbes, Aging Indicator ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12266770/]
- 119. Gut microbiota and epigenetic choreography: Implications for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11398772/]
- 120. Epigenetic regulation by gut microbiota - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8744890/]
- 121. The Efficacy of Probiotics, Prebiotics, Synbiotics, and Fecal ... [https://pubmed.ncbi.nlm.nih.gov/38999862/]
- 122. The Efficacy of Probiotics, Prebiotics, Synbiotics, and Fecal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11243554/]
- 123. Efficacy of encapsulated fecal microbiota transplantation ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1648944/full]
- 124. The probiotic enhances donor microbiota stability and ... [https://www.sciencedirect.com/science/article/pii/S2090123225001778]
- 125. Epigenetic clocks and DNA methylation biomarkers of ... [https://pubmed.ncbi.nlm.nih.gov/40533525/]
- 126. A blood-based epigenetic clock for intrinsic capacity ... [https://www.nature.com/articles/s43587-025-00883-5]
- 127. Gut microbiota and epigenetic age acceleration: a bi- ... [https://link.springer.com/article/10.1007/s40520-024-02877-6]
- 128. Accelerated biological aging based on DNA methylation ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1640853/full]
- 129. Diet-gut microbiota-epigenetics in metabolic diseases [https://www.sciencedirect.com/science/article/pii/S0753332222006795]