The Brain Tissue Dilemma
Why Alzheimer's Research Stalls in the "Valley of Death"
Alzheimer's disease (AD) looms as one of modern medicine's most formidable challenges. By 2060, an estimated 13.8 million Americans could be living with Alzheimer's dementia—a near doubling from today's 7.2 million 1 . Despite decades of research, the failure rate for AD drug development remains a staggering 99% 6 . This crisis centers on the "Valley of Death": the perilous gap between laboratory discoveries and effective patient treatments.
13.8M
Projected AD cases in US by 2060
99%
AD drug failure rate
$5.6B
Average development cost
The Translational Gap: Why Alzheimer's Drugs Fail
The "Valley of Death" metaphor describes the collapse of promising therapies during the transition from preclinical studies to human trials. Key factors driving this include:
Prohibitive Costs
Developing a single AD drug takes ~13 years and costs $5.6 billion—far exceeding oncology ($793 million) or average drug development ($2.8 billion) 6 .
Imperfect Models
Mice engineered to develop amyloid plaques fail to replicate human AD complexity. Amyloid deposits also accumulate in bone marrow, disrupting bone-building cells 5 .
Late Diagnosis
By the time symptoms appear, irreversible neurodegeneration has occurred. Autopsy tissue reveals "battlefield damage" but obscures early triggers 7 .
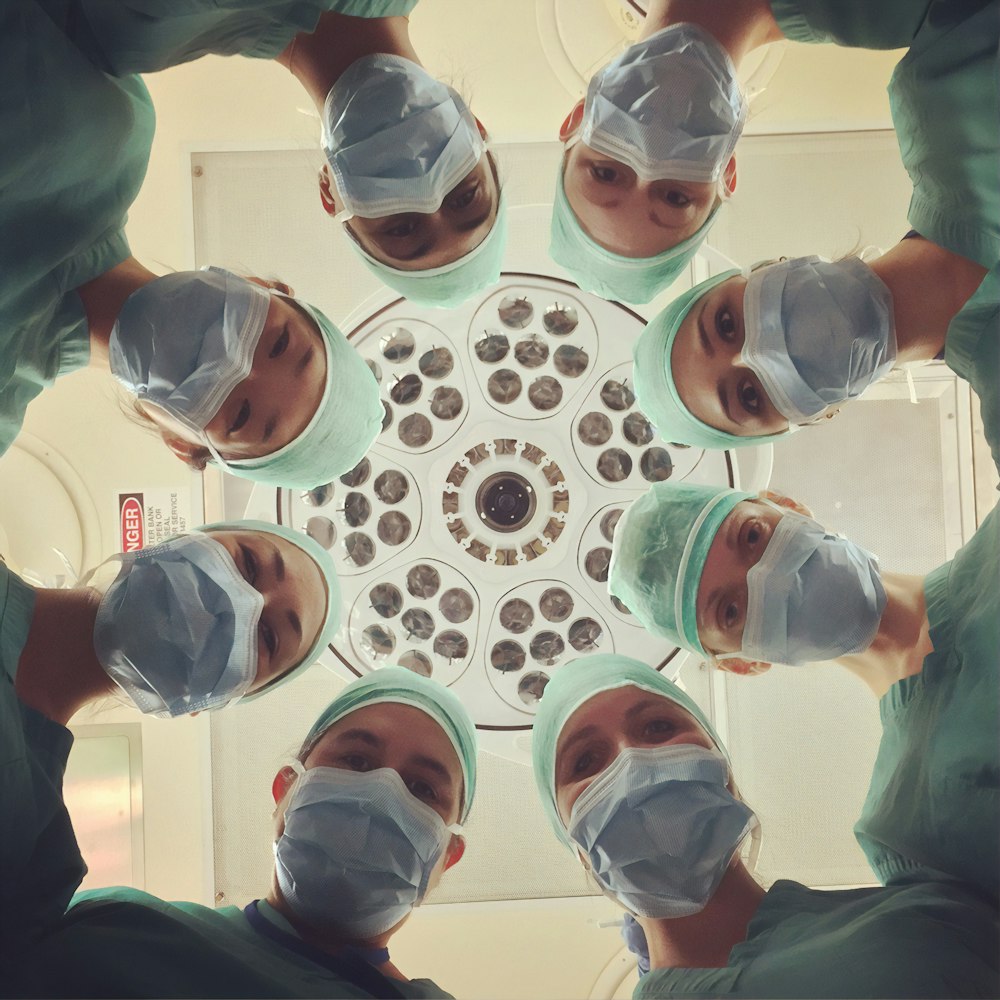
The Human Brain Tissue Shortage: A Fatal Bottleneck
Human brain tissue remains the gold standard for validating disease mechanisms, yet access is limited:
- Postmortem Samples Dominate: Initiatives provide invaluable donated brains, but these capture only end-stage pathology 7 .
- Dynamic Processes Go Unseen: Critical real-time interactions must be inferred from static tissue.
- Early-Stage Samples Are Rare: Only 1% of brain banks hold samples from mild cognitive impairment cases 7 .
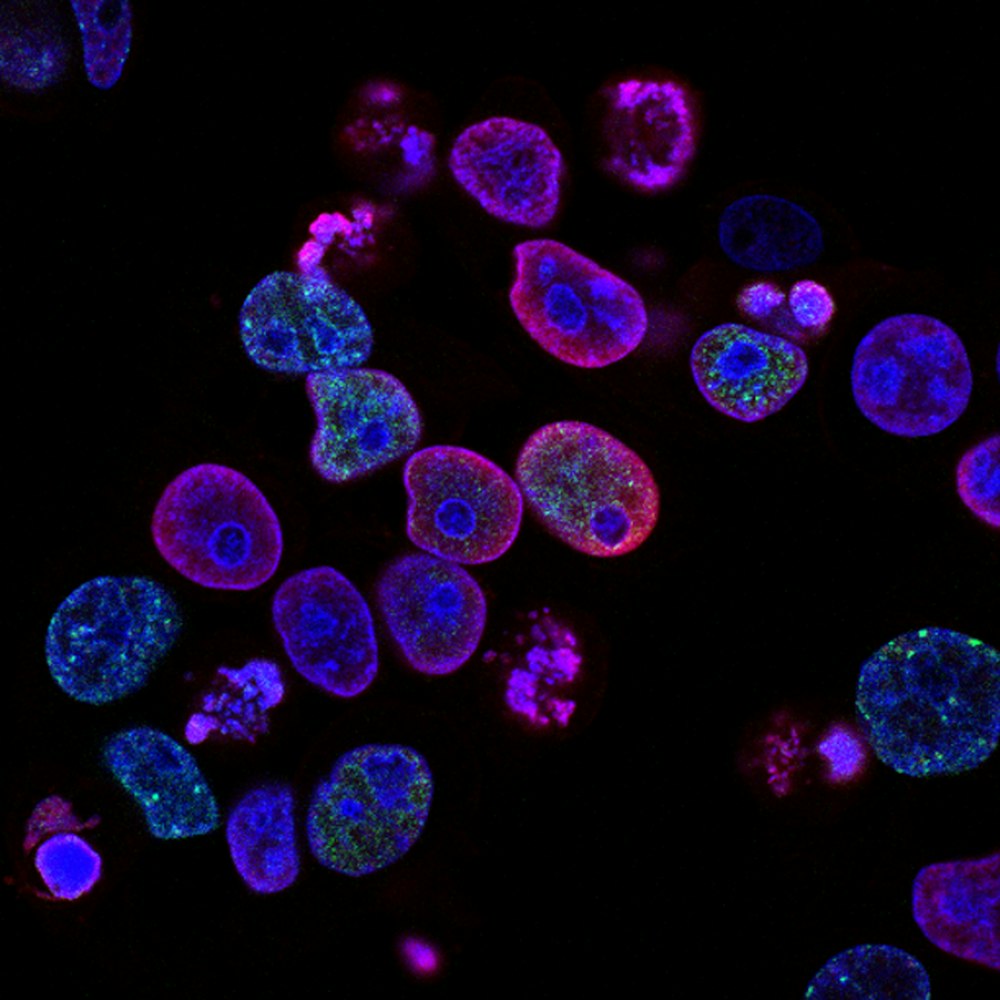
Featured Experiment: The Lithium Breakthrough
A landmark 2025 Nature study led by Harvard's Bruce Yankner revealed lithium's role in AD—and why past clinical trials failed 3 7 9 .
Methodology:
- Human Tissue Analysis: Using mass spectrometry to measure trace metals in brain samples from three cohorts
- Dietary Depletion in Mice: Healthy mice received lithium-restricted diets
- Therapeutic Intervention: Mice received lithium orotate via drinking water
Key Results:
| Group | Lithium Concentration (ppm) | Change vs. Healthy |
|---|---|---|
| Healthy | 0.42 ± 0.05 | Baseline |
| MCI | 0.29 ± 0.04 | ↓ 30% |
| Alzheimer's | 0.17 ± 0.03 | ↓ 60% |
The Scientist's Toolkit: Essential Reagents for Alzheimer's Research
| Reagent/Method | Function | Example |
|---|---|---|
| CRISPR-Cas9 | Gene editing to probe disease mechanisms | Boosting ACE in microglia to clear amyloid plaques 2 |
| 40Hz Gamma Stimulation | Non-invasive brain entrainment | MIT trials showing reduced amyloid 4 |
| Lithium Orotate | Amyloid-evading lithium compound | Reversing memory loss in AD mice 7 9 |
Beyond Amyloid: New Therapeutic Avenues
The lithium study exemplifies a paradigm shift: targeting systemic deficits rather than single proteins. Other promising approaches include:
Microglia Engineering
Cedars-Sinai researchers used gene editing to boost ACE in microglia, "supercharging" them to clear plaques 2 .

Gamma Wave Therapy
MIT's 40Hz sensory stimulation promotes anti-inflammatory signals and amyloid clearance 4 .
Bone-Brain Axis
Johns Hopkins found amyloid in bone marrow accelerates osteoporosis 5 .
Conclusion: A Path Forward
The Valley of Death persists, but human tissue insights are lighting exits. Initiatives now prioritize longitudinal tissue banks capturing early AD stages 6 . Meanwhile, the discovery of lithium's role—and its capture by amyloid—reveals why "failed" trials may reflect flawed delivery, not flawed biology.
"Lithium targets all the major pathologies of Alzheimer's. I have not seen anything quite like it."