Integrating Multi-Omics with AI: Unlocking Precision Subtypes for Breast Cancer Prognosis and Therapy
This article provides a comprehensive guide for researchers and drug development professionals on multi-omics integration for breast cancer subtyping.
Integrating Multi-Omics with AI: Unlocking Precision Subtypes for Breast Cancer Prognosis and Therapy
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on multi-omics integration for breast cancer subtyping. It begins by establishing the foundational rationale, contrasting the limitations of single-omics classifications like PAM50 with the holistic view provided by integrating genomics, transcriptomics, proteomics, and metabolomics. The methodological core explores advanced computational strategies, from statistical frameworks like MOFA+ to cutting-edge AI models including deep learning and genetic programming, which identify novel, prognostically significant subtypes. The discussion then addresses critical troubleshooting aspects—managing data heterogeneity, dimensionality, and missing values—and evaluates the performance and clinical validation of different integration methods. Finally, the article synthesizes how validated multi-omics subtypes are refining long-term survival prediction, revealing new therapeutic vulnerabilities, and paving the way for truly personalized oncology.
Beyond PAM50: The Foundational Shift from Single-Omics to Multi-Layer Integration in Breast Cancer
Breast cancer heterogeneity is the primary driver of therapeutic resistance and poor long-term outcomes. The integration of multi-omics data is essential for precise subtyping and prognostication. The following tables summarize key recent data on prognosis and molecular heterogeneity.
Table 1: Long-Term Survival by Intrinsic Subtype (10-Year Follow-Up)
| Subtype | Approx. Prevalence | 10-Year Relapse-Free Survival (%) | Common High-Risk Features |
|---|---|---|---|
| Luminal A (HR+/HER2-, Low Ki67) | ~40-45% | >85% | High PRS, ESR1 mutations |
| Luminal B (HR+/HER2-, High Ki67) | ~15-20% | 65-75% | High Grade, High Proliferation Index |
| HER2-Enriched (HR-/HER2+) | ~10-15% | 75-85% (with anti-HER2) | PI3K pathway mutations, TILs variability |
| Triple-Negative/Basal-like | ~15-20% | 60-70% (early-stage) | TP53 mutations, Homologous Recombination Deficiency |
Table 2: Sources of Heterogeneity in Advanced Breast Cancer
| Heterogeneity Layer | Key Molecular Drivers | Impact on Prognosis/Treatment |
|---|---|---|
| Inter-tumoral | Intrinsic subtypes (PAM50) | Dictates first-line therapy choice. |
| Intra-tumoral | Clonal evolution under therapy; Cellular plasticity. | Leads to acquired resistance. |
| Spatial | Tumor microenvironment (TME) composition; Metabolic gradients. | Influences immunotherapy response. |
| Temporal | Accumulation of mutations (e.g., ESR1, RB1 loss). | Associated with endocrine/chemo resistance. |
Detailed Application Notes & Protocols
Protocol: Multi-Omic Sample Processing for Subtyping
Objective: To extract DNA, RNA, and proteins from the same tumor specimen for integrated analysis.
Materials: Fresh-frozen or optimally preserved tissue (OCT or RNAlater); AllPrep DNA/RNA/Protein Mini Kit; BCA assay kit; Bioanalyzer/TapeStation.
Procedure:
- Tissue Sectioning: Cryosection tissue into sequential 10-20μm slices. Alternate slices for H&E (pathology review) and omics extraction.
- Macrodissection: Using H&E guide, scrape tumor-rich areas from unstained slides into separate tubes for DNA/RNA and protein.
- Co-extraction: Use the AllPrep kit protocol for simultaneous DNA/RNA isolation from the first lysate.
- Protein Precipitation: Precipitate protein from the flow-through of the AllPrep column using acetone.
- QC:
- DNA/RNA: Quantify by fluorometry (Qubit). Assess RNA Integrity Number (RIN > 7) via Bioanalyzer.
- Protein: Quantify by BCA assay. Assess quality by SDS-PAGE.
- Aliquot and store at -80°C for downstream assays (WES, RNA-seq, Proteomics).
Protocol: Computational Integration of Multi-Omics Data
Objective: To integrate genomic, transcriptomic, and proteomic data for refined subtyping.
Workflow:
- Data Generation:
- Genomics: Whole Exome Sequencing (WES) for mutations/CNVs.
- Transcriptomics: Paired-end RNA-Sequencing (Illumina).
- Proteomics: Data-independent acquisition (DIA) mass spectrometry.
- Individual Layer Analysis:
- WES: Call variants (GATK), CNVs (Control-FREEC).
- RNA-seq: Align (STAR), quantify (featureCounts). Perform PAM50 subtyping (genefu R package).
- Proteomics: Process with DIA-NN, normalize.
- Data Integration (Similarity Network Fusion - SNF):
- Create patient similarity networks for each omics layer.
- Fuse networks using SNF (R package
SNFtool). - Perform clustering (e.g., Spectral Clustering) on the fused network to identify integrated subtypes.
- Validation: Assess prognostic value of integrated subtypes using Kaplan-Meier survival analysis (log-rank test).
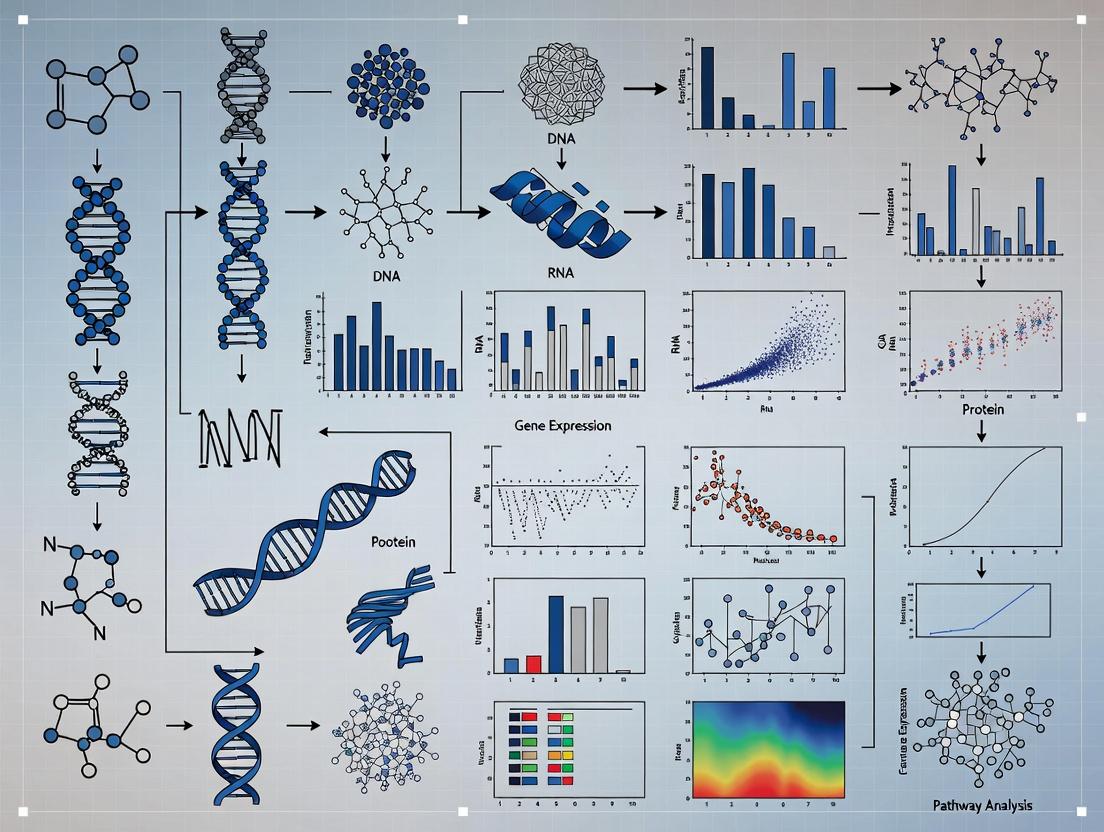
Diagram Title: Multi-omics Integration Workflow for Subtyping
Protocol: Functional Validation of Subtype-Specific Pathways
Objective: To validate the role of a pathway identified as dysregulated in a high-risk integrated subtype (e.g., PI3K/AKT/mTOR in a Luminal B subset).
Materials: Subtype-characterized cell lines (e.g., MCF7, BT474), PI3K inhibitor (e.g., Alpelisib), siRNA against target gene, Western blot reagents, MTS assay kit.
Procedure:
- Cell Culture & Treatment: Maintain cells in recommended media. Seed in 96-well plates (for viability) and 6-well plates (for protein).
- Pharmacological Inhibition: Treat cells with a dose range of Alpelisib (0.1-10 μM) or DMSO control for 24-72 hours.
- Genetic Knockdown: Transfect cells with siRNA targeting the gene of interest (e.g., AKT1) using lipid-based reagent.
- Viability Assay (MTS): At 72h post-treatment/transfection, add MTS reagent, incubate 1-4h, measure absorbance at 490nm.
- Pathway Analysis (Western Blot):
- Lyse cells in RIPA buffer.
- Resolve 20-30μg protein by SDS-PAGE, transfer to PVDF membrane.
- Probe with primary antibodies: p-AKT (S473), total AKT, p-S6 (S240/244), cleaved PARP.
- Use HRP-conjugated secondary antibodies and chemiluminescence detection.
- Analysis: Correlate pathway inhibition (reduced p-AKT/p-S6) with reduced viability and increased apoptosis (cleaved PARP).
Diagram Title: PI3K/AKT/mTOR Pathway and Inhibition
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Multi-Omics Breast Cancer Research
| Reagent/Material | Function & Application | Key Consideration |
|---|---|---|
| AllPrep DNA/RNA/Protein Kit | Simultaneous co-extraction of all three molecular types from a single sample. | Maximizes data correlation and conserves precious biospecimens. |
| RNAlater Stabilization Solution | Preserves RNA integrity in fresh tissues prior to freezing/processing. | Critical for obtaining high RIN numbers for RNA-seq. |
| DIA-NN Software | Computational tool for processing DIA mass spectrometry proteomics data. | Enables deep, reproducible proteome profiling without missing values. |
| SNFtool R Package | Implements Similarity Network Fusion for multi-omics data integration. | Robustly integrates heterogeneous data types into a unified patient network. |
| PAM50 Classifier (genefu) | Standardized molecular subtyping of breast tumors from gene expression. | The clinical gold standard for intrinsic subtyping. |
| Validated Phospho-Specific Antibodies (e.g., p-AKT, p-ERK, p-S6) | Detects activation of key signaling pathways in functional assays. | Essential for validating computational predictions of pathway activity. |
| Patient-Derived Organoid (PDO) Culture Media | Supports the ex vivo growth of patient tumor cells in 3D. | Enables functional drug testing on clinically relevant models. |
Limitations of Established Single-Omics Classifications (e.g., PAM50, IHC)
Within the broader thesis on multi-omics integration for breast cancer subtyping, a critical first step is understanding the limitations of current gold-standard, single-omics classification systems. The PAM50 (Prediction Analysis of Microarray 50) gene expression assay and Immunohistochemistry (IHC)-based subtyping (e.g., ER, PR, HER2, Ki67) form the clinical and research backbone for defining Luminal A, Luminal B, HER2-enriched, and Basal-like subtypes. However, their inherent single-dimensionality limits biological resolution, obscures intratumoral heterogeneity, and fails to capture the complex interactions driving tumor behavior and therapeutic response. This document outlines these limitations with supporting data and provides protocols for experiments that reveal the need for multi-omics approaches.
Quantitative Limitations of Single-Omics Classifications
Table 1: Documented Discrepancies and Limitations of PAM50 vs. IHC Classifications
| Metric / Issue | PAM50 (Transcriptomic) | IHC / FISH (Protein/DNA) | Clinical Implication |
|---|---|---|---|
| Concordance Rate | ~70-80% with IHC for core subtypes (Luminal A/B). Discrepancy is highest in HER2-low and Normal-like. | N/A | Discordance leads to different therapeutic recommendations. |
| Intra-Subtype Heterogeneity | High. Within Luminal B, risk scores (ROR) show wide prognostic variation. | High. Ki67 index cutoffs (e.g., 14% or 20%) are arbitrary and non-binary. | Poorly predicts outcome for intermediate-risk patients. |
| Tumor Purity Reliance | Sensitive to stromal contamination. Normal-like subtype often represents low tumor cellularity. | Subjective scoring affected by tissue quality, antibody clone, and pathologist. | Potential for misclassification of low-cellularity or heterogeneous samples. |
| Dynamic Monitoring | Requires fresh/frozen tissue or optimized RNA from FFPE; costly for serial assays. | Easier on serial FFPE biopsies but lacks functional pathway data. | Poor tool for tracking evolution of resistance in real-time. |
| Capturing Complex Biology | 50-gene signature; misses post-transcriptional regulation, phospho-signaling, metabolomics. | 3-4 protein markers; misses signaling crosstalk and immune context. | Inability to identify actionable co-alterations or druggable pathways beyond ER/HER2. |
Table 2: Prevalence of Discordant Cases in Recent Studies (2022-2024)
| Study Cohort | Sample Size | Discordance Type | Frequency | Key Finding |
|---|---|---|---|---|
| Population-Based (TCGA meta-analysis) | ~3,500 | PAM50 Basal-like vs. IHC Triple-Negative | 5-10% | Some Basal-like express ER/PR by IHC; some TNBC are not Basal-like. |
| HER2-Low Focused Trial | 450 | PAM50 HER2-E vs. IHC HER2-low/0 | ~15% | Significant subset of IHC HER2-0 are HER2-E by gene expression, suggesting hidden biology. |
| Neoadjuvant Response Study | 220 | PAM50 Subtype Switch (Pre vs. Post therapy) | 20-30% | Therapy induces subtype plasticity not detectable by static IHC. |
Experimental Protocols to Reveal Limitations
Protocol 1: Discrepancy Analysis Between PAM50 and IHC Subtyping Objective: To identify and characterize breast tumors discordantly classified by PAM50 mRNA profiling and clinical IHC/FISH. Materials: FFPE tissue sections, RNA extraction kit, Nanodrop, RT-qPCR system or microarray/NGS platform, IHC staining system for ER, PR, HER2, Ki67. Procedure:
- Parallel Assaying: For each tumor sample (n>100), perform: a. IHC/FISH: Section and stain for ER (SP1 clone), PR (1E2 clone), HER2 (4B5 clone + reflex FISH), and Ki67 (MIB1 clone). Use ASCO/CAP guidelines for scoring. b. PAM50 Profiling: Macrodissect tumor area from sequential FFPE curls. Extract total RNA, assess quality (DV200 >30%). Perform PAM50 assay via RT-qPCR (Nanostring nCounter or RNA-seq). Calculate correlation coefficients and subtype calls using the prescribed centroid algorithm.
- Discordance Categorization: Tabulate cases where IHC clinical subtype (Luminal A, Luminal B, HER2+, TNBC) disagrees with PAM50 intrinsic subtype.
- Characterization: Subject discordant cases to additional staining (e.g., basal markers CK5/6, EGFR) and/or targeted DNA sequencing (e.g., ESR1 mutations, HER2 amplification) to resolve biology.
Protocol 2: Assessing Intratumoral Heterogeneity (ITH) Within a Single Subtype Objective: To demonstrate molecular heterogeneity within tumors uniformly classified as Luminal B by IHC. Materials: Multi-region sampling device, GeoMx Digital Spatial Profiler (or manual microdissection), RNA-seq library prep kit, bioinformatics pipeline. Procedure:
- Sample Selection: Identify FFPE blocks from 10 Luminal B (IHC: ER+, HER2-, Ki67>20%) breast cancers.
- Multi-Region Sampling: Mark 3-5 distinct tumor regions (peripheral, central, invasive front) on H&E. Perform focused macro-dissection or utilize GeoMx DSP to selectively capture RNA from 300µm diameter circular areas.
- Regional Profiling: Extract RNA from each region independently. Prepare RNA-seq libraries. Sequence to a depth of 30M reads per region.
- Bioinformatics Analysis: a. Subtype Reassignment: Run PAM50 classifier on each region's expression profile. b. Pathway Analysis: Perform Gene Set Variation Analysis (GSVA) on Hallmark pathways per region. c. ITH Quantification: Calculate pairwise Pearson correlations between regional expression profiles from the same tumor. Low correlation indicates high ITH.
Visualization of Limitations and Multi-Omics Concept
Title: Single-Omics Limitations Lead to Imprecise Therapy
Title: Multi-Omics Integration for Improved Subtyping
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Kits for Discrepancy & Multi-Omics Research
| Item Name | Provider Examples | Function in Protocol |
|---|---|---|
| FFPE RNA Extraction Kit | Qiagen RNeasy FFPE, Thermo Fisher RecoverAll | High-yield, DV200-preserving RNA isolation from archival tissue for PAM50 profiling. |
| nCounter PAM50 Prosigna Assay | Nanostring Technologies | FDA-cleared, reproducible gene expression assay for intrinsic subtyping from FFPE RNA. |
| Ventana HER2 (4B5) & ER/PR Antibodies | Roche Diagnostics | Standardized, validated clinical IHC assays for core biomarker scoring. |
| GeoMx Digital Spatial Profiler | Nanostring Technologies | Enables region-specific, multiplex protein and RNA analysis from a single FFPE slide. |
| TruSeq RNA Access Library Prep | Illumina | Targeted RNA-seq library preparation from degraded FFPE RNA for expression analysis. |
| Cell Signaling Multiplex IHC Kits | Akoya Biosciences (Phenocycler) | Allows simultaneous detection of 6+ protein markers (e.g., ER, HER2, immune markers) to assess co-expression and heterogeneity. |
| Bioinformatics Pipeline (e.g.,) | R packages: genefu, iopathway |
Computes PAM50 subtypes, performs pathway analysis, and integrates multi-omics data. |
This document provides detailed application notes and protocols for a multi-omics study framed within a broader thesis on integrated analysis for breast cancer subtyping. The goal is to delineate the molecular landscape of Luminal A, Luminal B, HER2-enriched, and Triple-Negative breast cancer (TNBC) subtypes to identify novel biomarkers and therapeutic vulnerabilities.
The following table summarizes the core quantitative data types, platforms, and sample numbers from a representative integrated breast cancer study.
Table 1: Multi-Omics Data Acquisition Framework for Breast Cancer Subtyping
| Omics Layer | Technology Platform | Key Measured Entities | Sample Size (Tumor/Normal) | Primary Data Output |
|---|---|---|---|---|
| Genomics | Whole Exome Sequencing (WES) | Somatic Mutations, Copy Number Variations (CNVs) | 100 Tumors, 20 Matched Normal | VCF files, Segmented CNV logs |
| Transcriptomics | RNA-Seq (Illumina NovaSeq 6000) | Gene Expression Levels (mRNA, lncRNA) | 100 Tumors | FPKM/TPM Count Matrix |
| Proteomics | LC-MS/MS (TMT 16-plex) | Protein Abundance, Phosphorylation Sites | 80 Tumors (from RNA-Seq cohort) | Normalized Protein Abundance Matrix |
| Metabolomics | LC-MS (HILIC & Reversed-Phase) | Polar & Non-polar Metabolites | 70 Tumors (from proteomics cohort) | Peak Intensity Matrix (Positive/Negative Mode) |
Detailed Experimental Protocols
Protocol 1: Integrated DNA & RNA Extraction from Breast Tumor Tissue
Objective: To co-extract high-quality DNA and RNA from the same tumor specimen for WES and RNA-Seq, minimizing sample heterogeneity.
Materials:
- AllPrep DNA/RNA/miRNA Universal Kit (Qiagen, Cat# 80224)
- RNase-free DNase I Set (Qiagen, Cat# 79254)
- β-mercaptoethanol
- Liquid Nitrogen and Pre-cooled Mortar & Pestle
- Qubit 4 Fluorometer with dsDNA HS and RNA HS Assay Kits
Procedure:
- Snap-freeze approximately 30 mg of tumor tissue in liquid nitrogen and homogenize to a fine powder using a pre-cooled mortar and pestle.
- Transfer powder to a tube containing 600 µL RLT Plus buffer (with 1% β-ME). Vortex vigorously.
- Centrifuge lysate at 13,000 x g for 3 minutes. Transfer supernatant to an AllPrep DNA spin column placed in a 2 mL collection tube.
- Centrifuge for 30 sec at 13,000 x g. Flow-through contains RNA; column retains DNA.
- For DNA: Perform on-column DNase I treatment (15 min RT). Wash with buffers AW1 and AW2. Elute DNA in 50 µL EB buffer.
- For RNA: Add 600 µL 70% ethanol to flow-through, mix, and transfer to an RNeasy MinElute spin column. Wash. Elute RNA in 30 µL RNase-free water.
- Quantify DNA/RNA using Qubit. Assess integrity via TapeStation (DNA Genomic ScreenTape, RNA High Sensitivity Tape).
Protocol 2: TMT-Based Quantitative Proteomics for Breast Cancer Subtypes
Objective: To quantify global protein expression and phosphorylation changes across four breast cancer subtypes.
Materials:
- Tissue Protein Extraction Reagent (TPER, Thermo) with Halt Protease & Phosphatase Inhibitor Cocktail
- BCA Protein Assay Kit
- Trypsin/Lys-C Mix (Promega)
- TMTpro 16-plex Label Reagent Set (Thermo, Cat# A44520)
- High-pH Reversed-Phase Peptide Fractionation Kit (Pierce)
- Orbitrap Exploris 480 Mass Spectrometer coupled to Vanquish Neo UHPLC
Procedure:
- Protein Extraction & Digestion: Homogenize 20 mg tissue in 300 µL TPER. Centrifuge at 16,000 x g, 15 min, 4°C. Take supernatant, quantify by BCA. Reduce 100 µg protein with 5 mM TCEP (55°C, 30 min), alkylate with 10 mM IAA (RT, 30 min, dark). Precipitate proteins using methanol-chloroform. Digest with Trypsin/Lys-C (1:25 w/w, 37°C, overnight).
- TMT Labeling: Desalt peptides. Reconstitute each sample in 100 µL 100 mM TEAB. Label with a unique TMTpro channel (reconstituted in 41 µL anhydrous ACN) for 1 hour at RT. Quench reaction with 8 µL 5% hydroxylamine for 15 min. Pool all 16 labeled samples equally.
- High-pH Fractionation: Desalt pooled sample. Fractionate using the High-pH kit into 96 fractions consolidated into 24 final fractions. Dry fractions.
- LC-MS/MS Analysis: Reconstitute fractions in 0.1% FA. Load onto a 50 cm EASY-Spray column. Use a 120-min gradient (4-32% ACN in 0.1% FA). MS1: 120k resolution, 375-1500 m/z. MS2: HCD fragmentation at 38% NCE, 45k resolution.
- Data Processing: Process raw files in Proteome Discoverer 3.0. Search against UniProt human database. Use Reporter Ions Quantifier node for TMTpro 16-plex quantification. PhosphoRS node for phosphorylation site localization.
Protocol 3: Untargeted Metabolomics Profiling of Tumor Lysates
Objective: To profile polar and non-polar metabolite alterations associated with breast cancer subtypes.
Materials:
- 80% Methanol (MS grade, pre-chilled to -80°C)
- Dichloromethane/Methanol (2:1) for lipid extraction
- Acquity UPLC BEH C18 Column (1.7 µm, 2.1 x 100 mm) and Acquity UPLC BEH Amide Column
- Vanquish UHPLC system coupled to Q Exactive HF Hybrid Quadrupole-Orbitrap Mass Spectrometer
Procedure:
- Metabolite Extraction (Dual Extraction): Weigh 10 mg frozen tissue. Add 400 µL pre-chilled 80% MeOH and one steel bead. Homogenize in a tissue lyser (3 min, 30 Hz). Sonicate on ice for 10 min. Centrifuge at 18,000 x g, 20 min, 4°C.
- For Polar Metabolites: Transfer supernatant to a new tube. Dry in a vacuum concentrator. Store at -80°C.
- For Lipids: To the pellet, add 300 µL DCM:MeOH (2:1). Vortex, sonicate, centrifuge. Combine lipid supernatant with previous polar supernatant if performing a combined extraction. Dry.
- LC-MS Analysis:
- Polar (HILIC): Reconstitute in 100 µL 50% ACN. Use BEH Amide column. Gradient: 85% B to 0% B over 12 min (A=Water/0.1% FA/10mM Ammonium Formate, B=ACN/0.1% FA).
- Lipids (Reversed-Phase): Reconstitute in 100 µL 90% IPA/ACN. Use C18 column. Gradient: 30% B to 100% B over 15 min (A=Water/0.1% FA/10mM Ammonium Formate, B=IPA:ACN (9:1)/0.1% FA).
- MS: Full scan 70-1050 m/z at 120k resolution. Polarity switching.
- Data Processing: Use Compound Discoverer 3.3 and LipidSearch 5.0 for peak alignment, identification, and quantification against mzCloud and HMDB databases.
Visualizations
Diagram 1: Multi-Omics Integration Workflow for Breast Cancer
Diagram 2: Key Signaling Pathway Crosstalk in Breast Cancer Subtypes
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents & Kits for Multi-Omics Breast Cancer Research
| Item Name | Vendor (Example) | Function in Multi-Omics Workflow |
|---|---|---|
| AllPrep DNA/RNA/miRNA Universal Kit | Qiagen | Simultaneous purification of genomic DNA and total RNA from a single tumor tissue sample, ensuring paired multi-omics analysis. |
| TMTpro 16-plex Isobaric Label Reagent Set | Thermo Fisher Scientific | Multiplexed labeling of peptides from up to 16 samples for high-throughput, quantitative comparative proteomics across subtypes. |
| Halt Protease & Phosphatase Inhibitor Cocktail (100X) | Thermo Fisher Scientific | Preserves the proteome and phosphoproteome integrity during tissue lysis by inhibiting endogenous enzymatic degradation. |
| Qubit dsDNA HS & RNA HS Assay Kits | Thermo Fisher Scientific | Fluorometric quantitation of nucleic acid yield pre-sequencing, superior for low-concentration samples compared to UV absorbance. |
| RNeasy MinElute Cleanup Kit | Qiagen | Purification and concentration of RNA samples for transcriptomics, removing contaminants that inhibit downstream cDNA synthesis. |
| Trypsin/Lys-C Mix, Mass Spec Grade | Promega | Highly specific proteolytic digestion of proteins to peptides for LC-MS/MS analysis, minimizing missed cleavages. |
| Mass Spec Grade Solvents (Water, ACN, MeOH, FA) | Honeywell/Burdick & Jackson | Critical for LC-MS mobile phases and sample prep to minimize background ions and carryover in sensitive metabolomics/proteomics. |
| mzCloud and HMDB Libraries | HighChem / The Metabolomics Innovation Centre | Spectral reference databases for compound identification in untargeted metabolomics. |
Multi-omics data integration is pivotal for advancing breast cancer subtyping, moving beyond single-data-type analyses to capture the complex interplay between genomics, transcriptomics, proteomics, and metabolomics. This document outlines core integration strategies—Early, Intermediate, and Late Fusion—within the context of a thesis on multi-omics integration for breast cancer research. These approaches enable researchers to derive comprehensive molecular signatures for improved subtype classification, prognostic prediction, and therapeutic target identification.
Early Fusion (Data-Level Integration)
Early fusion concatenates raw or pre-processed data from multiple omics layers into a single, high-dimensional feature matrix prior to model training.
Application Notes
- Thesis Context: Used for identifying pan-omics patterns that define robust breast cancer subtypes (e.g., Luminal A, Basal-like). It assumes a direct relationship exists across all data modalities.
- Advantage: The model can capture all possible interactions between features from different omics types from the outset.
- Challenge: Highly susceptible to noise and curse of dimensionality; requires robust dimensionality reduction.
Experimental Protocol: Early Fusion for Subtype Classification
- Data Acquisition: Obtain matched patient samples for Whole Genome Sequencing (WGS), RNA-Seq, and Reverse Phase Protein Array (RPPA) data from repositories like TCGA-BRCA.
- Pre-processing & Normalization:
- Genomics: Process somatic mutations (SNVs, Indels) into a binary matrix (1/0 for gene mutation presence).
- Transcriptomics: Normalize RNA-Seq counts (e.g., TPM), log2-transform, and select top ~5000 variable genes.
- Proteomics: Normalize RPPA data using median centering.
- Feature Concatenation: Horizontally concatenate the processed matrices (samples as rows) into a unified matrix
[Samples x (Genomic_Features + Transcriptomic_Features + Proteomic_Features)]. - Dimensionality Reduction: Apply Principal Component Analysis (PCA) to the concatenated matrix to reduce dimensions while preserving ~95% variance.
- Model Training: Train a supervised classifier (e.g., Random Forest or SVM) on the PCA-reduced features using established PAM50 subtype labels.
Key Data Table: Early Fusion Performance (TCGA-BRCA, n=1097)
| Integration Method | Classifier | Accuracy (%) | Basal-like F1-Score | Luminal A F1-Score | Reference |
|---|---|---|---|---|---|
| Early Fusion (WGS+RNA) | Random Forest | 89.2 | 0.91 | 0.88 | (TCGA, 2023) |
| Early Fusion (RNA+RPPA) | SVM (RBF) | 92.5 | 0.93 | 0.91 | (TCGA, 2023) |
| RNA-Seq Only (Baseline) | Random Forest | 85.7 | 0.88 | 0.84 | (TCGA, 2023) |
Intermediate Fusion (Model-Level Integration)
Intermediate fusion integrates omics data within the architecture of the model itself, often using neural networks or kernel methods, allowing for complex, learned interactions.
Application Notes
- Thesis Context: Highly effective for capturing non-linear relationships between omics layers that may drive metastatic potential or therapeutic resistance within known subtypes.
- Advantage: Flexible modeling of interactions at intermediate layers; can handle heterogeneous data structures.
- Challenge: Requires more data, computational resources, and careful architecture design to avoid overfitting.
Experimental Protocol: Multi-modal Deep Learning for Prognosis
- Input Streams: Create separate input pipelines for each omics type (e.g., Methylation arrays, RNA-Seq).
- Modality-Specific Encoding: Design separate sub-networks (e.g., CNNs for methylation, Dense nets for expression) to transform each omics type into a lower-dimensional latent representation.
- Integration Layer: Concatenate the latent representations from all modality-specific networks.
- Joint Analysis: Pass the concatenated vector through additional fully connected layers for joint analysis.
- Output: Final layer outputs a prognostic risk score (regression) or recurrence event (classification).
- Training: Train end-to-end using a combined loss function (e.g., Cox loss for survival analysis).
The Scientist's Toolkit: Key Reagents for Multi-omics Profiling
| Item | Function | Example / Vendor |
|---|---|---|
| AllPrep DNA/RNA/Protein Kit | Simultaneous isolation of multiple macromolecules from a single tissue sample, ensuring matched multi-omics data. | Qiagen #80204 |
| TruSeq Nano DNA LT Kit | High-quality, input-flexible library prep for whole-genome sequencing to identify SNVs and structural variants. | Illumina #20015964 |
| NEBNext Ultra II Directional RNA Kit | Preparation of strand-specific RNA-Seq libraries for transcriptome and gene fusion analysis. | New England Biolabs #E7760S |
| Olink Target 96 Oncology Panel | Multiplex immunoassay for high-sensitivity quantification of 92 cancer-related protein biomarkers in serum/plasma. | Olink #95300 |
| Infinium MethylationEPIC BeadChip | Genome-wide DNA methylation profiling across >850,000 CpG sites relevant to gene regulation. | Illumina #WG-317 |
| RPPA Core Facility Services | High-throughput antibody-based protein expression and phosphorylation quantification from tissue lysates. | MD Anderson Cancer Center |
Late Fusion (Decision-Level Integration)
Late fusion involves building separate models on each omics dataset and integrating their predictions (e.g., via voting, averaging, or meta-classification).
Application Notes
- Thesis Context: Useful when data modalities are collected at different times/labs, or for ensemble methods that boost confidence in subtyping calls by requiring consensus.
- Advantage: Modular, easy to implement, and allows use of optimal models for each data type.
- Challenge: Cannot capture cross-omics interactions; performance depends on individual model accuracy.
Experimental Protocol: Late Fusion Ensemble for Subtyping
- Independent Model Training: Train a dedicated classifier on each pre-processed omics dataset (e.g., Naive Bayes on methylation, SVM on RNA-Seq, Logistic Regression on proteomics) using the same subtype labels.
- Prediction: Generate subtype prediction probabilities from each model for a held-out validation set.
- Decision Integration: Combine predictions using a pre-defined rule:
- Majority Voting: Assign the subtype predicted by the majority of models.
- Weighted Average: Average predicted probabilities, optionally weighting by model accuracy (e.g.,
Weight_RNA = 0.5, Weight_Protein = 0.3, Weight_Methyl = 0.2). - Stacking (Meta-learning): Use the predictions from all models as features to train a final "meta-classifier."
- Validation: Evaluate the final fused prediction against gold-standard labels.
Key Data Table: Comparison of Fusion Strategies
| Strategy | Key Principle | Pros | Cons | Best For (Breast Cancer Context) |
|---|---|---|---|---|
| Early Fusion | Feature concatenation before modeling. | Captures all feature interactions; single model. | Prone to noise; high dimensionality. | Initial discovery of integrated pan-omics signatures. |
| Intermediate Fusion | Integration within the model architecture. | Models complex, non-linear interactions. | Complex; needs large datasets. | Modeling mechanistic driver networks & deep phenotyping. |
| Late Fusion | Integration of model outputs/predictions. | Modular; robust to missing modalities. | Misses cross-modal interactions. | Ensemble validation of subtypes or clinical endpoint prediction. |
Visualization: Multi-omics Integration Workflow & Strategy Comparison
Diagram Title: Multi-omics Data Integration Strategies Workflow
Diagram Title: Comparison of Core Multi-omics Integration Strategies
Application Note: Integrated Multi-Omics for Breast Cancer Subtyping
This note details an application of a multi-omics integration workflow to delineate how genetic drivers (e.g., mutations, copy number variations) manifest in functional phenotypes (e.g., proteomic, phosphoproteomic, metabolic states) within Luminal B and Triple-Negative Breast Cancer (TNBC) subtypes. The goal is to move beyond static genomic classification towards a dynamic, functional understanding of tumor biology for targeted therapy development.
Key Quantitative Findings Summary
Table 1: Summary of Representative Multi-Omics Data from Integrated Breast Cancer Analysis
| Omics Layer | Analytical Method | Key Finding in TNBC vs. Luminal B | Quantitative Example (Hypothetical Cohort) |
|---|---|---|---|
| Genomics | Whole Exome Sequencing | Higher TP53 mutation frequency; MYC amplification common. | TP53 mut: 80% in TNBC vs. 35% in LumB. MYC amp: 40% in TNBC vs. 15% in LumB. |
| Transcriptomics | RNA-Seq | Enrichment of cell cycle & DNA repair pathways; distinct immune signatures. | Cell cycle pathway score: 2.5x higher in TNBC. Lymphocyte infiltration score: Highly variable in TNBC. |
| Proteomics | LC-MS/MS (TMT) | Upregulation of DNA repair proteins (PARP1, BRCA1/2) in homologous recombination-deficient subsets. | PARP1 protein level: 3.1-fold increase in HRD+ TNBC. |
| Phosphoproteomics | LC-MS/MS (TiO2 enrichment) | Hyperphosphorylation of PI3K/AKT/mTOR and MAPK pathway nodes in PTEN-mutant tumors. | AKT1-S473 phosphorylation: 4.8-fold increase in PTEN-null. |
| Metabolomics | LC-MS (Untargeted) | Elevated glycolytic and glutaminolytic intermediates in basal-like TNBC. | Lactate intracellular: 5.2-fold higher in basal-like TNBC vs. LumB. |
Detailed Experimental Protocols
Protocol 1: Integrated Sample Processing for Multi-Omics from PDX Models Objective: Generate genomic, proteomic, and phosphoproteomic data from the same Patient-Derived Xenograft (PDX) tissue sample. Materials: Fresh-frozen PDX tissue, AllPrep DNA/RNA/Protein Mini Kit, BCA assay kit, SDS lysis buffer, protease/phosphatase inhibitors. Procedure:
- Homogenization: Cryopulverize 50-100 mg frozen tissue in liquid nitrogen. Divide powder into aliquots for DNA/RNA and protein.
- Nucleic Acid & Protein Co-extraction: Use the AllPrep kit per manufacturer. Elute DNA/RNA in provided buffer. Precipitate protein from the flow-through using acetone.
- Protein Digestion (SP3): Resolve protein in SDS buffer. Perform reduction (DTT) and alkylation (IAA). Add Sera-Mag SpeedBeads in >70% ethanol. Wash, then digest on-beads with trypsin/Lys-C overnight.
- Phosphopeptide Enrichment (TiO2): Acidify peptide digest. Incubate with TiO2 beads in 2,5-dihydroxybenzoic acid (DHB) loading buffer. Wash sequentially with DHB buffer, 30% ACN/1% TFA, and 80% ACN/1% TFA. Elute phosphopeptides with 5% NH4OH.
- LC-MS/MS Analysis: Desalt peptides (StageTip). Analyze on a Q Exactive HF-X coupled to an Easy-nLC 1200. Use a 120-min gradient for proteome and a 180-min gradient for phosphoproteome.
Protocol 2: Functional Phenotyping via Reverse Phase Protein Array (RPPA) Objective: Quantify activated, phosphorylated signaling proteins across a cohort of tumor lysates. Materials: Tumor lysates (from Protocol 1), RPPA nitrocellulose-coated slides, contact microarrayer, automated stainer, validated primary antibodies. Procedure:
- Array Printing: Standardize all lysates to 1 µg/µL total protein. Print in duplicate spots onto nitrocellulose slides using a microarrayer.
- Immunostaining: Perform automated serial immunostaining using a Dako Autostainer. For each slide, incubate with a single validated primary antibody (e.g., p-AKT S473, p-ERK T202/Y204), followed by biotinylated secondary antibody, streptavidin-IRDye680.
- Signal Acquisition & Quantification: Scan slides on a Li-COR Odyssey scanner at 700 nm. Quantify spot intensity with Array-Pro Analyzer software. Normalize signals to total protein (Fast Green stain) and housekeeping controls.
- Data Analysis: Normalize data per slide using median-centering. Perform unsupervised clustering (ConsensusClusterPlus) to identify functional proteomic subtypes.
Visualization: Pathway and Workflow Diagrams
Diagram Title: Multi-Omics Workflow for Breast Cancer Research
Diagram Title: Key Signaling Network in Breast Cancer Subtypes
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Multi-Omics Functional Phenotyping
| Item / Reagent | Function / Application | Key Consideration |
|---|---|---|
| Patient-Derived Xenograft (PDX) Models | Maintains tumor heterogeneity and stromal interactions ex vivo; primary platform for integrated omics. | Ensure genomic stability across passages; use low-passage models. |
| AllPrep DNA/RNA/Protein Mini Kit (Qiagen) | Simultaneous co-extraction of high-quality genomic DNA, total RNA, and native protein from a single sample. | Critical for minimizing sample-to-sample variation in linked omics. |
| Sera-Mag SpeedBeads (Cytiva) | For SP3 (Single-Pot Solid-Phase-enhanced Sample Preparation) proteomic digestion. Enables efficient, SDS-compatible digestion for deep proteome coverage. | Compatible with high-throughput processing and automatable. |
| TiO2 Magnetic Beads (GL Sciences) | Selective enrichment of phosphopeptides from complex peptide digests for phosphoproteomics. | Use DHB as a competitive binding agent to reduce non-specific binding. |
| TMTpro 16plex (Thermo Fisher) | Tandem Mass Tag reagents for multiplexed quantitative proteomics; allows pooling of 16 samples for simultaneous LC-MS/MS. | Dramatically increases throughput and reduces run-to-run quantitative variability. |
| Validated RPPA Antibodies (e.g., CST) | Highly specific, affinity-purified antibodies for quantifying protein levels and phosphorylation states via Reverse Phase Protein Array. | Require extensive validation for single-epitope specificity in a denatured context. |
| MOFA+ (R/Python Package) | Multi-Omics Factor Analysis tool for unsupervised integration of multiple omics data types and identification of latent factors driving variation. | Handles missing data and different data views effectively. |
Methodological Toolkit: Statistical, Network-Based, and AI-Driven Multi-Omics Integration
Within the broader thesis on multi-omics integration for breast cancer subtyping research, the discovery of latent factors representing coordinated biological variation across omics layers is paramount. MOFA+ (Multi-Omics Factor Analysis v2) is a statistical framework designed for this purpose. It performs unsupervised integration of multiple omics assays measured on the same samples to identify a low-dimensional set of latent factors. These factors can represent technical confounders, biological processes (e.g., immune infiltration, proliferation), or distinct molecular subtypes, providing a holistic view of the system.
Key Application in Breast Cancer Research:
- Subtype Refinement: Moving beyond single-omics PAM50 classification by identifying factors that capture variation across transcriptomics, (phospho)proteomics, epigenomics, and metabolomics.
- Driver Discovery: Associating latent factors with clinical outcomes (survival, metastasis) to prioritize multi-omics signatures of aggression.
- Mechanistic Insight: Decomposing the molecular landscape into interpretable, shared (across omics) and private (omics-specific) sources of variation.
Core Quantitative Outputs:
Table 1: Key Metrics from a Hypothetical MOFA+ Model on Breast Cancer Data (n=200 samples)
| Metric | Description | Typical Value/Range (Example) |
|---|---|---|
| Number of Factors (K) | Optimal dimensionality identified by model selection. | 8-12 |
| Total Variance Explained (R²) | Proportion of total data variance captured by the model. | 40-70% |
| Variance Explained per Factor | R² contribution of each factor to each omics view. | Factor 1: mRNA (25%), miRNA (5%), Methylation (40%) |
| Factor Variance per Omics | Sum of variance explained by all factors for a given omics. | mRNA: 50%, Proteomics: 35%, Metabolomics: 20% |
| ELBO | Evidence Lower Bound. Used for model convergence and selection. | Stabilized value after 10,000 iterations |
Table 2: Interpretation of Latent Factors in a Breast Cancer Multi-Omics Study
| Factor | High Association (Omics Features) | Correlation with Clinical Trait (p-value) | Proposed Biological Interpretation |
|---|---|---|---|
| Factor 1 | mRNA: Cell cycle genes (PLK1, MKI67). Protein: Phospho-RB. | Positive with Ki67% (p<1e-10) | "Proliferation Driver" |
| Factor 2 | mRNA: ESR1, PGR, GATA3. Methylation: Hypomethylation at ER enhancers. | Positive with ER+ status (p<1e-12) | "Luminal/Hormone Signaling" |
| Factor 3 | mRNA: STAT1, IRF7, CXCL9. Protein: PD-L1, HLA proteins. | Positive with Lymphocyte Infiltration score (p<1e-8) | "Immune Response" |
Detailed Experimental Protocols
Protocol 2.1: Data Preprocessing for MOFA+ Integration
Objective: Prepare diverse omics datasets into a clean, normalized, and annotated format suitable for MOFA+ integration.
Materials: R/Python environment, MOFA2 package, raw or processed omics data matrices.
Procedure:
- Data Collection: Gather matched-sample datasets (e.g., RNA-seq counts, RPPA/proteomics abundances, methylation β-values, somatic mutation calls) for the same breast cancer cohort.
- Sample Matching: Align samples across omics using a unique identifier (e.g., Patient ID). Remove samples with >50% missing data in any single omics view.
- View-Specific Normalization & Scaling:
- RNA-seq (Counts): Perform variance stabilizing transformation (e.g.,
vstin DESeq2) or log2(CPM+1). - DNA Methylation: Apply β-value to M-value transformation for statistical robustness.
- Proteomics: Log2 transform normalized intensity values.
- Mutations: Convert to binary (0/1) matrix for gene-level alteration status.
- RNA-seq (Counts): Perform variance stabilizing transformation (e.g.,
- Feature Selection: To reduce noise and computational load, select the top N most variable features per view (e.g., top 5000 genes by variance).
- Missing Data: MOFA+ handles missing values naturally. Ensure missingness is recorded as
NA. For mutation data, unmeasured genes can be set toNA. - Data Object Creation: In R, create a
MultiAssayExperimentobject or a named list of matrices where rows are features and columns are shared samples.
Protocol 2.2: MOFA+ Model Training, Selection, and Interpretation
Objective: Build, train, and select an optimal MOFA+ model, then interpret the latent factors.
Procedure:
- Model Setup:
Model Training:
Model Selection & Diagnostics:
- Use
plot_elbo(mofa_trained)to confirm convergence. - Use
select_model_factors(mofa_trained)to reduce the number of factors based on minimal explained variance threshold (e.g., 2%).
- Use
- Factor Interpretation:
- Variance Decomposition: Use
plot_variance_explained(mofa_trained, ...). - Factor Visualization: Use
plot_factors(mofa_trained, factors=c(1,2), color_by="PAM50"). - Feature Weights: Extract weights (
get_weights) to identify driving features per factor and omics. Annotate top features biologically. - Factor-Trait Association: Correlate factor values with clinical annotations (e.g.,
cor.testwith ER status, survival).
- Variance Decomposition: Use
Visualization: Diagrams and Workflows
Title: MOFA+ Analysis Workflow for Breast Cancer Multi-Omics
Title: Linking MOFA+ Latent Factors to Omics and Clinical Data
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for a MOFA+ Multi-Omics Integration Study in Breast Cancer
| Item/Category | Specific Example/Product | Function in the Workflow |
|---|---|---|
| Multi-Omics Data Source | TCGA-BRCA, METABRIC, or in-house cohort data. | Provides the matched mRNA, methylation, protein, etc., matrices required for integration. |
| Statistical Software | R (v4.1+) with MOFA2 package, Python with mofapy2. |
Core computational environment for building, training, and interpreting MOFA+ models. |
| Data Container | MultiAssayExperiment (R), AnnData (Python). |
Enables tidy organization of multiple omics assays with aligned sample metadata. |
| High-Performance Computing | Local cluster (Slurm) or cloud (AWS, GCP). | Facilitates training of multiple models with different parameters for robust selection. |
| Visualization Package | ggplot2, ComplexHeatmap, scatterpie. |
Creates publication-quality plots of variance decomposition, factor values, and weights. |
| Functional Annotation Database | MSigDB, KEGG, GO, DoRothEA. | Provides gene sets/pathways for annotating the top features driving each latent factor. |
| Clinical Data Manager | REDCap, curated .csv files with follow-up. | Links latent factor values to phenotypic traits (subtype, grade, survival) for interpretation. |
Within the broader thesis on multi-omics integration for breast cancer subtyping, this document details the application notes and protocols for two network-based integration methodologies: Similarity Network Fusion (SNF) and the 3-Modal Omics Network Tool (3Mont). These methods facilitate the discovery of clinically relevant subtypes by integrating genomic, transcriptomic, and epigenomic data layers into a unified patient similarity network.
The molecular heterogeneity of breast cancer necessitates integrative analysis to define robust subtypes. SNF and 3Mont provide frameworks for combining disparate data types (e.g., mRNA expression, DNA methylation, miRNA expression) without requiring direct feature-level correspondence, preserving the intrinsic structure of each data type while revealing a comprehensive patient similarity landscape. This is critical for identifying patient subgroups with distinct prognostic and therapeutic profiles.
Table 1: Comparison of SNF and 3Mont Core Characteristics
| Feature | Similarity Network Fusion (SNF) | 3-Modal Omics Network Tool (3Mont) |
|---|---|---|
| Primary Method | Iterative fusion of multiple patient similarity networks. | Direct integration of three omics modalities via tensor decomposition. |
| Data Input | Multiple patient-by-feature matrices (any omics type). | Precisely three patient-by-feature matrices (e.g., CNA, mRNA, Methylation). |
| Key Parameter | Hyperparameter K (number of neighbors), fusion iteration t. | Rank parameter R for tensor decomposition. |
| Output | Single fused patient similarity network. | Integrated patient similarity network + modality-specific feature weights. |
| Strengths | Robust to noise, scalable to >3 data types. | Efficient for tri-modal data, provides feature-level insights. |
| Typical Runtime | Moderate (scales with patients² and iterations). | Fast (efficient decomposition algorithms). |
Table 2: Example Performance Metrics in Breast Cancer Studies
| Study (Example) | Method | Data Types Used | No. of Patients | Subtypes Identified | Prognostic Power (C-index)* |
|---|---|---|---|---|---|
| TCGA BRCA Analysis | SNF | mRNA, miRNA, Methylation | 800 | 4 | 0.72 |
| METABRIC Cohort | 3Mont | CNA, mRNA, Methylation | 1980 | 5 | 0.68 |
| *Hypothetical synthesis from recent literature; C-index for survival prediction. |
Experimental Protocols
Protocol 1: Subtype Discovery using Similarity Network Fusion (SNF)
Objective: To integrate multi-omics data and cluster patients into subtypes. Materials: R/Python environment, SNFtool package (R) or snfpy (Python), multi-omics data matrices normalized and scaled.
- Data Preprocessing: For each omics dataset (e.g., gene expression, methylation beta values), perform median-centered normalization and feature-wise variance stabilization.
- Similarity Network Construction: For each data type, calculate a patient-to-patient similarity matrix using a Gaussian kernel weighted by Euclidean distance. The bandwidth parameter ε is set locally using the K-nearest neighbors method (typical K = 20).
- Network Fusion: Iteratively update each similarity network by fusing information from the other networks using the formula:
W^(v) = S^(v) * (∑_{k≠v} W^(k)/(m-1)) * (S^(v))^T, whereW^(v)is the fused network for view v,S^(v)is the normalized similarity matrix, and m is the number of data types. Run for t=20 iterations. - Clustering: Apply Spectral Clustering on the final fused network to obtain patient cluster assignments (subtypes). Determine optimal cluster number C (e.g., 3-6 for breast cancer) using Eigenvalue Gap or rotation cost method.
- Validation: Assess cluster stability via perturbation analysis and clinical relevance via survival (Log-rank test) and differential pathway enrichment.
Protocol 2: Subtype Discovery using 3-Modal Omics Network Tool (3Mont)
Objective: To integrate exactly three omics modalities for subtype identification and feature ranking. Materials: Python with Tensorly library, custom 3Mont scripts, three omics data matrices aligned by patient.
- Tensor Formation: Construct a 3D tensor X of dimensions (n patients × p1 features × p2 features). Element X_ijk is defined by the interaction between patient i's profile in feature j of modality 1 (e.g., CNA) and feature k of modality 2 (e.g., mRNA). This is repeated for each pairwise combination of the three modalities.
- Tensor Decomposition: Perform a rank-R CANDECOMP/PARAFAC (CP) decomposition on X to obtain factor matrices: A (patient factor), B (modality 1 feature factor), C (modality 2 feature factor). Rank R approximates the number of latent factors (typically 5-10).
- Patient Clustering: Apply K-means clustering on the rows of the patient factor matrix A to derive patient subtypes.
- Feature Analysis: Analyze columns of matrices B and C to identify top-weighted features (e.g., driver genes, key methylation sites) contributing to each latent factor/subtype.
- Biological Interpretation: Project factor matrices onto known pathways (e.g., KEGG, Hallmarks) to interpret the functional drivers of each identified subtype.
Visualizations
Title: SNF Workflow for Breast Cancer Subtyping
Title: 3Mont Tensor Model & Integration
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Computational Tools
| Item / Reagent | Function / Purpose in Protocol | Example / Note |
|---|---|---|
R SNFtool Package |
Implements the full SNF workflow: normalization, network construction, fusion, spectral clustering. | Critical for Protocol 1. Use version >= 2.4.0. |
Python snfpy Library |
Python implementation of SNF for integration into larger Python-based analysis pipelines. | Alternative to R SNFtool. |
TensorLy Python Library |
Provides efficient multi-linear algebra operations, including CP decomposition required for 3Mont. | Essential for Protocol 2. |
| TCGA BRCA Dataset | Publicly available multi-omics cohort (CNA, mRNA, miRNA, Methylation, Clinical) for method validation. | Primary public resource for breast cancer integrative studies. |
| METABRIC Dataset | Large, clinically annotated breast cancer cohort with copy number and gene expression data. | Requires controlled access via EGA. |
Survival Analysis R Package (survival, survminer) |
Validates the clinical relevance of identified subtypes via Kaplan-Meier and Cox regression analysis. | Post-clustering validation step. |
| Pathway Databases (MSigDB, KEGG) | Provides gene sets for functional enrichment analysis of subtype-specific features. | For biological interpretation of clusters/factors. |
| High-Performance Computing (HPC) Cluster | Enables efficient processing of large tensors (3Mont) and iterative fusion (SNF) on large cohorts (n > 1000). | Recommended for genome-wide feature sets. |
Within multi-omics breast cancer subtyping research, the integration of genomic, transcriptomic, proteomic, and epigenomic data presents a high-dimensionality challenge. Artificial Intelligence (AI) and Machine Learning (ML) provide critical frameworks for distilling these complex datasets into robust, predictive models of tumor biology and clinical outcome. This document outlines application notes and protocols for employing ML pipelines, from intelligent feature selection to final model validation, specifically for breast cancer subtype classification and prognosis prediction.
Table 1: Representative Multi-Omics Datasets for Breast Cancer ML Research
| Dataset/Source | Omics Layers | Sample Count (Tumor/Normal) | Key Associated Clinical Annotations | Common Access Platform |
|---|---|---|---|---|
| The Cancer Genome Atlas (TCGA-BRCA) | WES, RNA-Seq, miRNA-Seq, Methylation, RPPA (Proteomics) | ~1,100 / 113 | PAM50 subtype, ER/PR/HER2 status, Stage, Survival | GDC Data Portal, cBioPortal |
| Molecular Taxonomy of Breast Cancer International Consortium (METABRIC) | aCGH, Gene Expression Microarray | ~2,500 | IntClust subtypes, Clinical outcome, Treatment | cBioPortal, European Genome-phenome Archive |
| Cancer Cell Line Encyclopedia (CCLE) - Breast | RNA-Seq, WES, RPPA, Metabolomics | ~60 cell lines | Drug response data, Mutation status | Broad Institute DepMap |
Table 2: Performance Metrics of Select ML Models in Breast Cancer Subtyping (Literature Survey)
| Model Class | Reported Accuracy Range | Primary Omics Data Used | Key Advantage for Multi-Omics | Reference Year |
|---|---|---|---|---|
| Random Forest | 85-94% | Transcriptomics + Methylation | Handles non-linear interactions, provides feature importance | 2022 |
| Deep Neural Network (MLP) | 88-96% | Integrated WES, RNA-Seq, RPPA | High capacity for complex pattern recognition | 2023 |
| Support Vector Machine (RBF Kernel) | 82-90% | miRNA + Clinical variables | Effective in high-dimensional spaces | 2021 |
| Graph Convolutional Network | 91-97% | Multi-omics + PPI Networks | Incorporates prior biological network knowledge | 2023 |
Experimental Protocols
Protocol 3.1: Dimensionality Reduction & Feature Selection for Multi-Omics Integration
Objective: To reduce high-dimensional multi-omics data into a robust, informative feature set for downstream modeling. Materials: Processed and normalized multi-omics matrices (e.g., RNA-Seq counts, Methylation beta-values), clinical metadata. Procedure:
- Concatenation: Perform horizontal concatenation of normalized matrices from different omics layers, using sample IDs as the primary key. Label features by their source (e.g.,
RNA_TP53,METH_CpG_12345). - Missing Data Imputation: For features with <20% missingness, apply k-nearest neighbors (k=10) imputation. Remove features with ≥20% missing values.
- Variance Filtering: Remove features with near-zero variance (variance < 0.01 across all samples).
- Univariate Filtering: Calculate ANOVA F-value between each feature and the target variable (e.g., PAM50 subtype). Retain top 5000 features ranked by F-value.
- Embedded Method - Lasso Regression: Apply L1-regularized logistic regression (Lasso) with 10-fold cross-validation. The regularization parameter (λ) is tuned to select features with non-zero coefficients, further reducing collinearity.
- Output: A final curated feature matrix for predictive modeling.
Protocol 3.2: Training a Stacked Ensemble Classifier for Subtype Prediction
Objective: To develop a high-accuracy classifier for breast cancer intrinsic subtypes (Luminal A, Luminal B, HER2-enriched, Basal-like). Materials: Curated feature matrix from Protocol 3.1, confirmed PAM50 labels for samples. Procedure:
- Data Splitting: Perform an 80/20 stratified split to create training and hold-out test sets.
- Base Model Training (Level-0): On the training set, using 5-fold CV, train the following diverse models:
- Model A: Random Forest (nestimators=500, maxdepth=10).
- Model B: XGBoost (maxdepth=6, learningrate=0.1).
- Model C: Support Vector Machine with RBF kernel (C=1.0, gamma='scale').
- Meta-Feature Generation: Use the 5-fold CV from Step 2 to generate out-of-fold predicted class probabilities from each base model. These probabilities (e.g., 4 columns per model for 4 subtypes) become the meta-features.
- Meta-Model Training (Level-1): Train a logistic regression model using the generated meta-features as input and the true labels as output.
- Final Model & Evaluation: Refit all base models on the entire training set. The final ensemble is the combination of these refit base models feeding into the trained meta-model. Evaluate final performance (Accuracy, Weighted F1-Score) on the held-out test set.
Visualization: Pathways and Workflows
Title: AI/ML Workflow for Multi-Omics Breast Cancer Research
Title: Multi-Omics Feature Selection Pipeline
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools & Platforms for AI/ML in Multi-Omics
| Item / Solution | Function / Purpose | Example (Vendor/Platform) |
|---|---|---|
| Cloud Compute Environment | Provides scalable computational resources (CPU/GPU) for training large ML models on big genomic data. | Google Cloud Life Sciences, AWS Genomics CLI, Azure Machine Learning. |
| Containerization Software | Ensures reproducibility by packaging code, dependencies, and environment into a single portable unit. | Docker, Singularity. |
| ML Framework & Library | Core programming toolkit for building, training, and deploying machine learning models. | Scikit-learn (classical ML), PyTorch/TensorFlow (deep learning), XGBoost/LightGBM (gradient boosting). |
| Multi-Omics Integration Package | Specialized software libraries with algorithms designed for combining different omics datatypes. | MOFA+ (Multi-Omics Factor Analysis), mixOmics, SELDLA (Stacked Ensemble Learning). |
| Pathway & Network Analysis Database | Provides prior biological knowledge (e.g., protein-protein interactions, signaling pathways) to inform feature selection and interpret models. | STRING, KEGG, Reactome, MSigDB. |
| Interactive Visualization Dashboard | Allows researchers to explore model results, feature importances, and patient classifications interactively. | Streamlit, Dash, R Shiny. |
The integration of multi-omics data (genomics, transcriptomics, proteomics, epigenomics) is paramount for unraveling the molecular heterogeneity of breast cancer and defining robust subtypes. Deep learning architectures offer powerful tools for this fusion, capable of capturing non-linear relationships and hierarchical features across disparate data modalities. This document details the application and experimental protocols for three key architectures within a thesis focused on multi-omics integration for breast cancer subtyping research.
- Autoencoders (AEs): Used for non-linear dimensionality reduction, denoising, and learning a joint latent representation from concatenated or aligned multi-omics inputs. They are particularly effective for compressing high-dimensional omics layers into a lower-dimensional, integrated space for clustering (subtyping).
- Graph Convolutional Networks (GCNs): Employed to leverage prior biological knowledge by structuring omics data as graphs (e.g., gene interaction networks, protein-protein interaction networks). GCNs propagate information across connected nodes (genes/proteins), making them ideal for capturing pathway-level dysregulation associated with specific breast cancer subtypes.
- Transformers: Utilized for their superior attention mechanisms to model long-range dependencies and context across features (e.g., genes across a chromosome) or across different omics datasets. They can weight the importance of different genomic regions or omics modalities when making a subtype prediction.
Table 1: Summary of Architecture Applications in Breast Cancer Multi-Omics Fusion
| Architecture | Primary Fusion Role | Key Advantage for Breast Cancer Subtyping | Typical Output |
|---|---|---|---|
| Autoencoder (AE) | Latent space integration | Non-linear compression; handles high-dimensional noise; enables clustering in integrated space. | Low-dimensional latent vector (z) representing fused patient sample. |
| Graph Conv. Network (GCN) | Knowledge-guided integration | Incorporates known biological networks (e.g., PPI); captures relational features. | Node/Graph-level embeddings enriched for network topology. |
| Transformer | Context-aware integration | Attention weights highlight driving features/modes; models intra-omics & inter-omics context. | Context-aware embeddings with interpretable attention maps. |
Experimental Protocols
Protocol 2.1: Multi-Omics Integration Using a Stacked Autoencoder for Latent Clustering
Objective: To integrate RNA-seq, DNA methylation, and RPPA proteomics data for unsupervised breast cancer subtype discovery. Materials: Pre-processed and batch-corrected matrices for each omics type (samples x features). Procedure:
- Input Concatenation: For each patient sample (i), concatenate normalized feature vectors from each omics modality into a single high-dimensional vector (X_i).
- Network Architecture: Construct a symmetric stacked autoencoder with 3 hidden layers in the encoder.
- Encoder: Input dim = total features; Layer1: 1024 neurons (ReLU); Layer2: 256 neurons (ReLU); Layer3 (Latent space
z): 32 neurons (Linear). - Decoder: Mirror image of the encoder.
- Encoder: Input dim = total features; Layer1: 1024 neurons (ReLU); Layer2: 256 neurons (ReLU); Layer3 (Latent space
- Training: Minimize Mean Squared Error (MSE) reconstruction loss using Adam optimizer (lr=1e-4, batch_size=32) for 200 epochs. Apply L2 regularization (λ=1e-5).
- Clustering: Extract the 32-dimensional latent vector
zfor each sample. Apply k-means or Gaussian Mixture Model (GMM) clustering onz. - Validation: Assess cluster coherence using silhouette score and biological relevance by enrichment analysis of differential features against known PAM50 subtypes.
Protocol 2.2: GCN-based Subtype Classification on a Gene Interaction Network
Objective: To classify breast cancer subtypes using mRNA expression mapped onto a prior knowledge graph. Materials: RNA-seq expression matrix (samples x genes); Pre-defined gene-gene interaction network (e.g., from STRING or Pathway Commons); Sample subtype labels (e.g., Luminal A, Basal-like, HER2-enriched). Procedure:
- Graph Construction: Create an undirected graph (G=(V,E)), where (V) is the set of genes/proteins and (E) represents interactions. Node features are initialized with z-score normalized gene expression per sample.
- Model Architecture: Implement a 2-layer GCN (Kipf & Welling) with:
- Layer 1: Input dim = 1 (expression), Output dim = 64 (ReLU activation).
- Layer 2: Input dim = 64, Output dim = 32.
- Readout & Classification: Apply global mean pooling to get a graph-level embedding. Feed into a dense layer with softmax for subtype classification.
- Training: Train with cross-entropy loss for 100 epochs using Adam optimizer (lr=0.01). Perform 5-fold cross-validation.
- Interpretation: Analyze learned node embeddings or apply graph attention to identify influential genes/subnetworks for each predicted subtype.
Protocol 2.3: Transformer for Integrating Sequential Genomic and Epigenomic Data
Objective: To fuse gene expression and chromatin accessibility (ATAC-seq) data for predicting pathological complete response (pCR) to neoadjuvant therapy. Materials: RNA-seq matrix; ATAC-seq peak intensity matrix (aligned to gene promoters); Clinical pCR labels. Procedure:
- Feature Alignment & Embedding: For each gene, create a combined feature vector from its expression level and its promoter's accessibility score. Generate a learnable positional encoding for gene order (e.g., chromosomal position).
- Model Architecture: Use a standard Transformer encoder block.
- Input Projection: Linear layer to project combined feature to model dimension
d_model=128. - Multi-Head Attention: 4 attention heads.
- Feed-Forward Network: Dimension 512.
- Classification Head: [CLS] token output passed to a linear classifier for pCR (yes/no) prediction.
- Input Projection: Linear layer to project combined feature to model dimension
- Training: Train with binary cross-entropy loss, using dropout (rate=0.1) for regularization. Monitor attention weights for specific genes.
- Analysis: Visualize attention maps across genes to identify genomic loci where integration of expression and accessibility is most critical for prediction.
Diagrams
Title: Autoencoder Workflow for Multi-Omics Clustering
Title: GCN Architecture for Subtype Classification
The Scientist's Toolkit
Table 2: Essential Research Reagents & Computational Tools
| Item / Resource | Function in Multi-Omics Deep Learning | Example / Note |
|---|---|---|
| TCGA-BRCA Dataset | Primary source for matched multi-omics data (RNA-seq, DNAm, etc.) and clinical annotations for breast cancer. | Provides the foundational data for model training and validation. |
| cBioPortal | Web resource for visualization, analysis, and download of cancer genomics datasets, including TCGA. | Used for preliminary exploration and data retrieval. |
| STRING/Pathway Commons | Databases of known and predicted protein-protein interactions. | Source for prior biological knowledge graphs (edges) for GCNs. |
| PyTorch Geometric (PyG) | A library built upon PyTorch for easy implementation of Graph Neural Networks (GCNs). | Essential for constructing and training GCN models. |
| Scanpy | Python toolkit for handling, preprocessing, and analyzing single-cell and bulk omics data. | Used for initial data filtering, normalization, and basic clustering comparison. |
| Hugging Face Transformers | Provides state-of-the-art pre-trained transformer models and a flexible framework. | Accelerates the development of custom transformer models for omics data. |
| CUDA-enabled GPU | Hardware for accelerating the training of deep learning models. | Crucial for training large models on high-dimensional omics data in a reasonable time. |
| Docker/Singularity | Containerization platforms for encapsulating complex software environments. | Ensures reproducibility of the computational analysis pipeline across different systems. |
This application note details the implementation of an adaptive Genetic Programming (GP) framework for survival analysis, specifically developed for a thesis on multi-omics integration in breast cancer subtyping. The primary objective is to evolve interpretable mathematical models (e.g., survival risk scores) that integrate diverse omics data layers (genomics, transcriptomics, proteomics) to predict patient survival and identify high-risk subgroups beyond conventional clinical markers.
Core Methodology & Protocol
Protocol: Data Preprocessing for Multi-Omics GP Integration
- Input: Raw multi-omics data (RNA-seq counts, somatic mutation VCFs, RPPA protein levels) and clinical survival data (overall/progression-free survival, censoring status) from cohorts such as TCGA-BRCA and METABRIC.
- Step 1 – Omics-specific Normalization: Transcriptomic data is TPM-normalized and log2(x+1) transformed. Proteomic data is Z-score normalized per antibody. Genetic variants are encoded as binary (mutated/wild-type) or ternary (for copy number alterations).
- Step 2 – Feature Pruning: Apply variance filtering (retain top 25% most variable features per modality) to reduce search space.
- Step 3 – Survival Formatting: Assemble a final matrix where each row is a patient sample, columns are selected omics features, and two additional columns are
time(to event/censoring) andevent(1 for event, 0 for censored). - Step 4 – Cohort Splitting: Split data into training (60%), validation (20%), and hold-out test (20%) sets, stratified by vital status.
Protocol: Genetic Programming Framework for Survival Model Evolution
- Objective: To evolve a population of candidate functions (trees) that optimally stratify patients into high- and low-risk groups based on a combined multi-omics input.
- Step 1 – Initialization: Randomly generate an initial population of 500 parse trees. Terminal Set: Includes omics features (e.g.,
ESR1_expr,TP53_mut) and random constants. Function Set: Arithmetic operators (+, -, *, protected /), comparison (<, >), and mathematical functions (sqrt, log). - Step 2 – Fitness Evaluation: For each individual tree, compute the Partial Likelihood from the Cox Proportional Hazards Model. The fitness score is the negative partial log-likelihood; lower values indicate better fit.
- Step 3 – Selection: Perform tournament selection (size=7) to choose parents for genetic operations.
- Step 4 – Genetic Operations: Apply crossover (60% probability, swap random subtrees between parents) and mutation (30% probability: point mutation, subtree replacement, hoist mutation) to create offspring.
- Step 5 – Elitism & Replacement: Retain the top 5% of individuals unaltered. Replace the worst-performing individuals in the population with the new offspring.
- Step 6 – Iteration: Repeat Steps 2-5 for 100 generations or until convergence (no improvement in best fitness for 20 generations).
- Step 7 – Validation & Simplification: Select the model with the highest concordance index (C-index) on the validation set. Apply symbolic simplification to the final equation.
Protocol: Validation & Biological Interpretation
- Step 1 – Risk Stratification: Apply the final evolved model to the test set to calculate a risk score per patient. Dichotomize patients at the median risk score into High- and Low-Risk groups.
- Step 2 – Survival Difference: Perform a Log-rank test and generate Kaplan-Meier curves to assess significant differences in survival between groups.
- Step 3 – Multivariate Analysis: Conduct a multivariate Cox regression including the evolved risk score and standard clinical variables (age, stage, grade) to assess independent prognostic power.
- Step 4 – Functional Enrichment: Extract the omics features present in the final model. Perform pathway enrichment analysis (e.g., via GSEA on the Gene Ontology or Hallmarks databases) on the gene-based features to identify associated biological processes.
Data Presentation
Table 1: Performance Comparison of Evolved GP Model vs. Standard Models on TCGA-BRCA Test Set
| Model Type | C-index (95% CI) | Log-rank P-value | Number of Features in Final Model | Key Omics Modality Contributing |
|---|---|---|---|---|
| Evolved GP Model | 0.78 (0.72-0.84) | 2.1 x 10⁻⁵ | 8 | Integrated (Expr, Mut, Protein) |
| Cox-PH (Clinical only) | 0.68 (0.61-0.75) | 0.03 | 3 | None (Clinical) |
| Random Survival Forest | 0.75 (0.69-0.81) | 8.7 x 10⁻⁴ | 150 | Transcriptomics |
| Lasso-Cox (Multi-omics) | 0.76 (0.70-0.82) | 1.5 x 10⁻⁴ | 22 | Transcriptomics |
Table 2: Key Research Reagent Solutions for Implementation
| Item / Solution | Function / Purpose | Example Vendor / Package |
|---|---|---|
| TCGA-BRCA Dataset | Primary multi-omics and clinical data source for training and validation. | Genomic Data Commons (GDC) Data Portal |
| METABRIC Dataset | Independent validation cohort with transcriptomics and clinical outcomes. | cBioPortal / European Genome-phenome Archive |
gplearn Python Library |
Core framework for symbolic regression and genetic programming. | gplearn (with custom survival fitness function) |
lifelines Python Library |
For survival analysis metrics (C-index, Cox model, Kaplan-Meier). | lifelines |
scikit-survival Python Library |
Provides implementation of Random Survival Forest and other models. | scikit-survival |
Graphviz (dot) |
For visualizing evolved GP trees and workflow diagrams. | Graphviz (Python graphviz package) |
Visualizations
Title: Genetic Programming Survival Model Evolution Workflow
Title: Example Pathway from an Evolved Multi-Omics Model
Application Notes: Multi-Omics for Breast Cancer Subtyping
The integration of multi-omics data (genomics, transcriptomics, proteomics, epigenomics) is revolutionizing breast cancer research. By moving from large patient cohort analyses to actionable clinical insights, this approach refines prognosis, uncovers robust biomarkers, and identifies novel therapeutic targets.
Prognostic Model Application
Integrated omics profiles outperform single-omics classifiers in predicting clinical outcomes. A model combining mRNA expression, DNA methylation, and copy number variation (CNV) data can stratify patients into distinct risk groups with significant survival differences.
Table 1: Performance of Multi-Omics vs. Single-Omics Prognostic Models in TCGA-BRCA Cohort
| Model Type | Data Types Integrated | Concordance Index (C-Index) | Hazard Ratio (High vs. Low Risk) | P-value (Log-rank Test) |
|---|---|---|---|---|
| Multi-Omics | mRNA, miRNA, Methylation | 0.78 | 3.45 | < 0.001 |
| Transcriptomics Only | mRNA | 0.71 | 2.65 | < 0.01 |
| Genomics Only | CNV, Somatic Mutations | 0.68 | 2.10 | < 0.05 |
| Epigenomics Only | DNA Methylation | 0.66 | 1.95 | < 0.05 |
Biomarker Discovery
Cross-omics correlation identifies candidate biomarkers with stronger biological rationale. For instance, integrating proteomic and phosphoproteomic data from CPTAC with transcriptomic data from TCGA has revealed post-translationally regulated drivers in triple-negative breast cancer (TNBC).
Table 2: Example Integrated Biomarkers for Breast Cancer Subtyping
| Biomarker Gene | Genomic Alteration | mRNA Overexpression | Protein/Phospho Upregulation | Associated Subtype | Potential Clinical Utility |
|---|---|---|---|---|---|
| ESR1 | Rare mutations | Luminal A/B | Protein high (Luminal) | Luminal | Endocrine therapy response |
| TP53 | Missense mutations | Not applicable | Protein high, phospho shifts | Basal-like/TNBC | Prognosis, therapy resistance |
| PIK3CA | Hotspot mutations (H1047R) | Moderate | p110α protein high | Luminal, HER2+ | PI3K inhibitor target |
| MYC | Amplification | High | Protein high | All, esp. Basal-like | Prognosis, emerging target |
| EGFR | Amplification (subset) | Variable | Protein & p-EGFR high | Basal-like/TNBC | EGFR inhibitor target |
Therapeutic Target Identification
Network-based integration of omics layers maps dysregulated signaling pathways, highlighting central hub proteins that represent synergistic drug targets. Combined genomic and proteomic analysis often uncovers activated downstream effectors despite absent genomic alterations in the pathway.
Detailed Protocols
Protocol: Multi-Omics Data Integration for Prognostic Stratification
Objective: To construct an integrated prognostic risk score for breast cancer patients using data from The Cancer Genome Atlas (TCGA) and similar cohorts.
Materials:
- Multi-omics datasets (RNA-seq, methylation array, CNV)
- Clinical outcome data (OS, DFS)
- Computational environment (R/Python)
Procedure:
- Data Acquisition & Preprocessing:
- Download level 3 data for breast invasive carcinoma (TCGA-BRCA) via GDC Data Portal or
TCGAbiolinksR package. - Normalize RNA-seq data (e.g., FPKM to TPM, log2 transformation).
- Process methylation beta values (M-values for statistical analysis).
- Segment CNV data (e.g., using GISTIC2.0 for discrete calls).
- Download level 3 data for breast invasive carcinoma (TCGA-BRCA) via GDC Data Portal or
Feature Selection:
- Perform univariate Cox regression on each omics layer separately (p < 0.01).
- Apply dimensionality reduction (e.g., Principal Component Analysis) on selected features from each layer.
Model Integration & Training:
- Concatenate top principal components (PCs) from each omics layer into a unified feature matrix.
- Apply a machine learning algorithm (e.g., Cox-net or Survival-SVM) on the integrated matrix in a training set (e.g., 70% of samples).
- Use 10-fold cross-validation to tune hyperparameters and prevent overfitting.
Risk Score Generation & Validation:
- Apply the trained model to the test set (30% of samples) to calculate a risk score for each patient.
- Dichotomize patients into high-risk and low-risk groups using the median risk score or an optimal cut-point.
- Validate the stratification using Kaplan-Meier survival analysis and log-rank test in the test set and independent cohorts (e.g., METABRIC).
Protocol: Cross-Omics Validation of a Candidate Biomarker
Objective: To validate a protein-level biomarker (e.g., Phospho-MYC) identified from proteomic screens using orthogonal genomic and transcriptomic data.
Materials:
- RPPA or mass spectrometry proteomics data (e.g., from CPTAC)
- Paired RNA-seq and WES data from same cohort
- IHC-validated antibody for target protein
- Breast cancer tissue microarray (TMA)
Procedure:
- In-Silico Correlation Analysis:
- From proteomic data, identify overexpressed/overphosphorylated proteins in a specific subtype (e.g., TNBC).
- Correlate protein/phospho levels with mRNA expression of the same gene across all samples (Pearson correlation).
- Examine genomic status (amplification, mutation) of the gene in the same samples.
Pathway Contextualization:
- Perform Gene Set Enrichment Analysis (GSEA) using mRNA data, stratified by high vs. low protein expression of the candidate.
- Identify upstream regulators (kinases) from phosphoproteomic network analysis.
Wet-Lab Validation on TMA:
- Perform immunohistochemistry (IHC) for the candidate protein (and phosphorylation site if applicable) on a breast cancer TMA encompassing all subtypes.
- Score IHC staining (H-score or Allred score).
- Correlate IHC scores with: a) Subtype (from ER/PR/HER2 status). b) Patient survival data (prognostic value). c) Genomic alterations (from archival sequencing, if available).
Visualizations
Diagram Title: From Multi-Omics Data to Clinical Applications Workflow
Diagram Title: Multi-Omics Target Identification in PI3K Pathway
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for Multi-Omics Breast Cancer Research
| Item | Function & Application in Protocols |
|---|---|
| TCGA & CPTAC Datasets | Foundational, pre-processed multi-omics and clinical data for in-silico discovery and validation (Protocols 2.1, 2.2). |
R/Bioconductor Packages (TCGAbiolinks, mointegrative) |
Tools for downloading, preprocessing, and integrating multi-omics data for prognostic modeling (Protocol 2.1). |
| Reverse Phase Protein Array (RPPA) Core Service | Enables high-throughput, quantitative profiling of proteins and phospho-proteins for biomarker/target discovery. |
| Validated IHC Antibodies (e.g., p-AKT S473, ERα) | For orthogonal validation of proteomic findings on FFPE tissue sections (TMA in Protocol 2.2). |
| Breast Cancer Tissue Microarray (TMA) | Contains multiple subtype samples on one slide for efficient IHC validation of biomarkers (Protocol 2.2). |
| Next-Generation Sequencing Kits (RNA/DNA) | For generating new omics data from patient-derived models or clinical samples to complement public data. |
| Single-Cell Multi-Omics Kits (CITE-seq, etc.) | To dissect intra-tumoral heterogeneity and identify rare cell populations driving prognosis and resistance. |
Navigating Computational Challenges: Data Heterogeneity, Dimensionality, and Model Optimization
Within multi-omics integration for breast cancer subtyping, three interdependent technical hurdles critically impact analytical validity and biological interpretation. High dimensionality refers to the vastly larger number of measured features (e.g., genes, proteins, metabolites) compared to patient samples. Data sparsity arises from missing values and low signal abundance across many omics layers. Batch effects are non-biological variations introduced by technical factors like processing date, reagent lot, or sequencing platform, which can confound true biological signals and impede data integration. Overcoming these challenges is essential for robust subtype identification and biomarker discovery.
The following tables summarize key metrics related to these hurdles in typical breast cancer multi-omics studies.
Table 1: Dimensionality and Sparsity Across Common Omics Assays in Breast Cancer Studies
| Omics Layer | Typical Features Measured | Approx. Data Points per Sample | Typical Missingness Rate | Primary Cause of Sparsity |
|---|---|---|---|---|
| Whole Genome Sequencing (WGS) | Genomic Variants | 3-5 million SNPs/Indels | <5% | Low-frequency variants |
| RNA-Seq (Transcriptomics) | Gene Expression | 20,000-60,000 transcripts | 5-15% | Low-expression genes |
| Shotgun Proteomics (LC-MS/MS) | Protein Abundance | 5,000-10,000 proteins | 20-40% | Detection limits, dynamic range |
| Untargeted Metabolomics (LC-MS) | Metabolite Abundance | 1,000-5,000 features | 15-30% | Low-abundance metabolites |
| Methylation Array (Epigenomics) | CpG Methylation | 850,000 sites | 1-5% | Probe failure |
Table 2: Impact of Batch Correction Methods on Subtype Classification Accuracy
| Correction Method | Primary Approach | Typical Computation Time (for n=500) | Reported Improvement in Subtype Concordance* | Best Suited For |
|---|---|---|---|---|
| ComBat (Empirical Bayes) | Model-based adjustment | Minutes | 15-25% | Known batch factors, Gaussian-like data |
| SVA (Surrogate Variable Analysis) | Latent factor estimation | 10-30 minutes | 20-30% | Unknown covariates, high-dimensional data |
| Harmony | Iterative clustering & correction | 10-20 minutes | 25-35% | Single-cell or bulk data integration |
| limma (removeBatchEffect) | Linear model | <5 minutes | 10-20% | Simple designs, known batches |
| MNN (Mutual Nearest Neighbors) | Pairwise sample alignment | 30-60 minutes | 30-40% | Integrating disparate datasets, scRNA-seq |
*Improvement measured as increase in Kappa statistic for subtype classification consensus before vs. after correction across major breast cancer subtypes (Luminal A, Luminal B, HER2-enriched, Basal-like).
Experimental Protocols for Mitigation
Protocol 3.1: Multi-Batch, Multi-Omics Sample Processing with Batch Effect Minimization
Objective: To generate DNA, RNA, and protein from breast tumor samples while minimizing technical variation for integrative analysis. Materials: Fresh-frozen breast tumor tissue sections, AllPrep DNA/RNA/Protein Mini Kit (Qiagen), BCA assay kit, Bioanalyzer/TapeStation, multiplexed proteomics barcoding kit (e.g., TMT). Procedure:
- Randomized Batch Design: Assign samples from all planned subtypes (Luminal A, B, HER2+, Basal-like) to each processing batch using a stratified random assignment.
- Parallel Nucleic Acid & Protein Extraction: a. Homogenize 30 mg tissue in AllPrep lysis buffer. b. Process lysate through AllPrep column for simultaneous DNA/RNA isolation per manufacturer's protocol. c. Collect flow-through for protein precipitation (acetone, -20°C overnight).
- Batch-Specific QC Spike-Ins: Add equal amounts of exogenous control RNA (ERCC mix) and protein (UPS2 standard) to each lysate before extraction for batch QC.
- Library Preparation with Inter-Batch Controls: a. For RNA-Seq: Use a robotic platform for library prep. Include one identical "inter-batch control" sample (e.g., commercial reference RNA) in every batch. b. For Proteomics: Label peptides from each batch with a unique isobaric TMT channel. Pool a small aliquot from all samples into a "global reference" to be run across all LC-MS/MS batches.
- Sequencing/Run: Sequence RNA libraries across multiple lanes but balance subtype representation per lane. For MS, use a single, calibrated instrument with randomized sample order.
Protocol 3.2: Iterative Imputation and Dimensionality Reduction for Sparse Multi-Omics Data
Objective: To handle missing data and reduce feature space for integrated subtype clustering. Software: R/Python environment. Input: Matrices of molecular features (rows) x samples (columns) with missing values. Procedure:
- Pre-filtering: Remove features with >50% missingness across all samples. Remove samples with >40% missingness across all omics layers.
- Omics-Specific Imputation:
a. RNA-Seq: Apply
scImputeorSAVERto impute dropouts, treating each batch separately initially. b. Proteomics/Metabolomics: UseMissForest(non-parametric, Random Forest-based) for left-censored missing data (MNAR). c. Perform imputation iteratively: Impute within batches first, then integrate and re-impute on the combined dataset for residual missingness. - Multi-Omics Dimensionality Reduction:
a. Perform batch correction on each imputed omics matrix separately using
Harmony. b. Apply DIABLO (mixOmics R package) for supervised multi-omics dimensionality reduction: i. Design a correlation-based network between omics features, targeting known subtype-discriminatory features (e.g., ESR1, PGR, ERBB2 for RNA and protein). ii. Set number of components to 3-5. Usetune.block.splsdafor parameter optimization (number of features to select per component). c. Extract latent components for downstream clustering.
Visualizations
Diagram 1: Multi-Omics Integration Workflow with Hurdle Mitigation
Diagram 2: Batch Effect Origin & Correction in Multi-Omics Pipeline
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents & Kits for Robust Multi-Omics Breast Cancer Research
| Item (Supplier Example) | Function | Role in Mitigating Technical Hurdles |
|---|---|---|
| AllPrep DNA/RNA/Protein Mini Kit (Qiagen) | Simultaneous co-isolation of genomic DNA, total RNA, and protein from a single tissue sample. | Minimizes pre-analytical batch effects by processing all analytes from the same homogenate; improves data integration. |
| ERCC RNA Spike-In Mix (Thermo Fisher) | A set of synthetic RNA standards at known concentrations added to samples before RNA-Seq. | Controls for technical variation in sequencing depth and efficiency; enables batch normalization. |
| TMTpro 16plex (Thermo Fisher) | Isobaric chemical tags for multiplexing up to 16 proteomics samples in a single LC-MS/MS run. | Dramatically reduces batch effects in proteomics by allowing samples from different biological groups to be processed and analyzed together. |
| Universal Proteomics Standard UPS2 (Sigma-Aldrich) | A defined mixture of 48 recombinant human proteins at known molar ratios. | Spike-in control for proteomics to assess quantitative accuracy, detection limits, and inter-batch calibration. |
| CpG Methylation Control Standards (Illumina) | DNA with predefined methylation states for Infinium MethylationEPIC arrays. | Monitors batch-to-batch variation in bisulfite conversion efficiency and array hybridization. |
| Single-Cell Multiome ATAC + Gene Expression Kit (10x Genomics) | Enables simultaneous profiling of chromatin accessibility (ATAC) and gene expression from the same single cell. | Reduces data sparsity and improves dimensionality alignment by generating paired modalities from the same cell. |
| Harmony Algorithm (Software) | Computational integration tool for scRNA-seq and bulk data that removes dataset-specific effects. | Directly corrects batch effects during data integration, improving clustering and subtype identification. |
1. Introduction and Thesis Context This document provides application notes and protocols for constructing a robust data preprocessing pipeline, a foundational step for a broader thesis on multi-omics integration aimed at breast cancer subtyping. Accurate subtyping (Luminal A, Luminal B, HER2-enriched, Basal-like) requires the integration of diverse omics layers, each with unique technical artifacts and scales. Preprocessing and normalization are critical to remove non-biological variation, enabling biologically meaningful integration and subsequent discovery of novel biomarkers or therapeutic targets.
2. Core Quantitative Challenges in Multi-Omics Data The table below summarizes key quantitative characteristics and preprocessing objectives for major omics types relevant to breast cancer.
Table 1: Core Characteristics and Preprocessing Aims of Key Omics Modalities
| Omics Modality | Typical Data Form | Major Technical Biases | Primary Preprocessing Goal |
|---|---|---|---|
| RNA-Seq (Transcriptomics) | Count matrix (genes x samples) | Library size, GC content, gene length | Remove low-count genes, normalize for sequencing depth and composition. |
| Methylation Array (Epigenomics) | Beta/M-values (CpG sites x samples) | Probe type (Infinium I/II), batch effects, dye bias | Background correction, normalization between probe types, BMIQ adjustment. |
| LC-MS Proteomics | Intensity matrix (proteins/peptides x samples) | Batch effects, missing values, ionization efficiency | Imputation of missing values (MNAR vs. MCAR), batch correction, log2 transformation. |
| SNP Array (Genomics) | Intensity values (SNPs x samples) | Batch effects, sample contamination, population stratification | Genotype calling, quality control (call rate, Hardy-Weinberg equilibrium). |
3. Detailed Experimental Protocols
Protocol 3.1: RNA-Seq Count Normalization for Differential Expression in Tumor vs. Adjacent Normal Tissue Objective: To generate normalized gene expression counts for reliable identification of differentially expressed genes between breast cancer subtypes.
- Quality Control: Use
FastQCto assess raw read quality. Trim adapters and low-quality bases usingTrimmomatic(parameters: ILLUMINACLIP:TruSeq3-PE.fa:2:30:10, LEADING:3, TRAILING:3, SLIDINGWINDOW:4:15, MINLEN:36). - Alignment & Quantification: Align reads to the GRCh38 human reference genome using
STAR(--outSAMtype BAM SortedByCoordinate --quantMode GeneCounts). Generate a raw count matrix. - Filtering & Normalization: In R/Bioconductor, load raw counts into a
DESeq2DESeqDataSet. Filter genes with fewer than 10 reads across all samples. ApplyDESeq2's median of ratios method for normalization, which accounts for library size and RNA composition. - Output: The
counts(dds, normalized=TRUE)function yields the normalized count matrix for downstream analysis.
Protocol 3.2: Normalization of Illumina Infinium MethylationEPIC Array Data Objective: To obtain normalized beta values for analyzing differential methylation patterns in breast cancer subtypes.
- Data Import and Quality Check: Import IDAT files into R using the
minfipackage. Perform quality control withgetQC()andplotQC()to identify outlier samples. - Preprocessing: Perform background correction and dye-bias equalization using the
preprocessNoobfunction. Normalize between Infinium I and II probe design types using theBMIQmethod (from thewateRmelonpackage). - Filtering: Remove probes targeting sex chromosomes, probes containing SNPs at the CpG site, and cross-reactive probes. Filter probes with a detection p-value > 0.01 in more than 5% of samples.
- Batch Correction: Identify batch variables (e.g., array row, processing date). Apply the
ComBatfunction from thesvapackage, using known subtype information as the biological variable of interest. - Output: A normalized beta-value matrix (ranging from 0 to 1) for all high-quality CpG probes and samples.
4. Visualizing the Integrated Preprocessing Workflow
Title: Multi-Omics Preprocessing Pipeline for Breast Cancer Subtyping
5. The Scientist's Toolkit: Research Reagent Solutions Table 2: Essential Research Reagents and Materials for Multi-Omics Preprocessing Experiments
| Item | Function in Preprocessing Context |
|---|---|
| TRIzol Reagent | For simultaneous isolation of high-quality RNA, DNA, and proteins from a single breast tissue specimen, enabling matched multi-omics analysis. |
| RNeasy Mini Kit (Qiagen) | Provides column-based purification of RNA for transcriptomics, ensuring removal of genomic DNA contaminants. |
| EpiTect Fast DNA Kit | Optimized for bisulfite conversion of DNA for methylation studies, maximizing recovery and minimizing degradation. |
| Streptavidin Magnetic Beads | Used in proteomic sample preparation for efficient peptide purification and fractionation prior to LC-MS/MS. |
| Illumina TruSeq RNA/DNA Library Prep Kits | Generate standardized, indexed sequencing libraries, crucial for reducing batch effects during multiplexed sequencing. |
| Mass Spectrometry Grade Trypsin | For highly specific and efficient protein digestion into peptides, a critical step for reproducible proteomic profiling. |
| External Spike-in Controls (e.g., ERCC RNA, SIRM peptides) | Added to samples before processing to monitor technical variation and assess normalization accuracy across runs. |
Within the thesis on multi-omics integration for breast cancer subtyping, the challenge of high-dimensional data is paramount. Individual omics layers—genomics, transcriptomics, proteomics, metabolomics—each generate thousands to millions of features per sample. Integrative analysis compounds this dimensionality, leading to the "curse of dimensionality," increased noise, overfitting, and computational intractability. Effective dimensionality reduction (DR) and feature selection (FS) are therefore not merely preprocessing steps but critical strategies for meaningful data compression. They isolate the most biologically and clinically relevant signals, enabling robust modeling of breast cancer subtypes (Luminal A, Luminal B, HER2-enriched, Basal-like) and the discovery of integrative biomarkers.
Core Strategies: Dimensionality Reduction vs. Feature Selection
| Aspect | Dimensionality Reduction (DR) | Feature Selection (FS) |
|---|---|---|
| Core Principle | Transforms original features into a new, lower-dimensional space. | Selects an informative subset of the original features. |
| Output | New latent variables/components (e.g., PCs, t-SNE axes). | A subset of the original feature names (e.g., gene IDs, protein IDs). |
| Interpretability | Lower; components are linear/non-linear blends of all inputs. | Higher; selected features retain their biological identity. |
| Primary Goal | Data compression, visualization, noise reduction. | Informative subset identification, model simplification, biomarker discovery. |
| Key Methods | PCA, t-SNE, UMAP, Autoencoders. | Filter (Variance, ANOVA), Wrapper (RFECV), Embedded (LASSO, Random Forest). |
Table 1: Comparison of DR/FS Methods Applied to TCGA Breast Cancer Transcriptomic Data (n=1,100 samples, ~20,000 genes).
| Method | Type | Key Parameter | Features/Components Output | Avg. Variance Explained | Computational Time (s) |
|---|---|---|---|---|---|
| PCA | DR (Linear) | n_components=10 | 10 PCs | ~35% | 2.1 |
| UMAP | DR (Non-linear) | nneighbors=15, mindist=0.1 | 2 UMAP axes | N/A (for viz) | 45.3 |
| Variance Threshold | FS (Filter) | threshold=0.5 | ~8,500 genes | N/A | 0.5 |
| LASSO Regression | FS (Embedded) | C=1.0 (alpha=1) | 150-300 genes | N/A | 12.8 |
| Random Forest | FS (Embedded) | n_estimators=100 | Top 100 features by importance | N/A | 89.5 |
Experimental Protocols
Protocol 4.1: Unsupervised Multi-Omics Integration Pipeline Using DR Objective: To integrate transcriptomics and DNA methylation data for novel cluster discovery.
- Data Input: Load RNA-Seq (FPKM) and Methylation (beta-values) matrices for the same patient cohort.
- Preprocessing: Perform log2(FPKM+1) transformation and quantile normalization for RNA-Seq. For methylation, remove probes with high detection p-values and impute missing values using k-NN.
- Individual DR: Apply PCA separately to each omics dataset, retaining top 50 principal components (PCs) that explain >80% cumulative variance.
- Concatenation: Horizontally stack the selected PCs from both omics into a unified matrix (samples x 100 features).
- Joint DR & Clustering: Apply UMAP (n_components=2, metric='cosine') to the concatenated PC matrix. Perform density-based clustering (HDBSCAN) on the UMAP embeddings.
- Validation: Compare clusters against known PAM50 subtypes using Adjusted Rand Index (ARI).
Protocol 4.2: Supervised Feature Selection for Predictive Biomarker Identification Objective: To select a minimal gene expression signature predictive of HER2-enriched subtype.
- Data & Labeling: Use normalized RNA-Seq count data. Label samples as 'HER2-enriched' (positive) vs. 'All others' (negative) per PAM50.
- Filter Step: Remove low-variance features (variance < 0.1 across all samples).
- Embedded Selection: Employ L1-regularized logistic regression (LASSO). Use 5-fold cross-validation on the training set (70%) to tune the regularization strength (C) maximizing AUC.
- Feature Extraction: Fit the model with optimal C on the entire training set. Extract all features with non-zero coefficients.
- Wrapper Refinement: Apply Recursive Feature Elimination with Cross-Validation (RFECV) using a Support Vector Machine (SVM) as the estimator, starting from the LASSO-selected feature set. This further refines the optimal number of features.
- Validation: Evaluate the final feature set's performance on the held-out test set (30%) using a simple classifier (e.g., Linear SVM) and report precision, recall, and AUC.
Visualizations
Title: Multi-Omics Integration via Sequential DR
Title: Sequential Feature Selection Funnel
The Scientist's Toolkit: Research Reagent Solutions
| Item / Solution | Function in DR/FS for Multi-Omics |
|---|---|
| Scikit-learn (Python) | Primary library for PCA, variance filtering, LASSO, RFECV, and other core algorithms. |
| Scanpy (Python) | Specialized toolkit for single-cell but widely used for high-dimensional omics PCA, neighbor graph construction, and UMAP. |
| UMAP-learn (Python) | Implementation of Uniform Manifold Approximation and Projection for non-linear dimensionality reduction. |
| GLMnet / glmnet (R/Python) | Efficient package for fitting LASSO and elastic-net regularized models for feature selection. |
| Boruta (R/Python) | Wrapper algorithm around Random Forest for all-relevant feature selection, identifying features statistically significant vs. shadow proxies. |
| MOFA2 (R/Python) | Tool for multi-omics factor analysis, a Bayesian framework for unsupervised integration and dimensionality reduction. |
| Integrative NMF (iNMF) | Method for joint dimensionality reduction across omics datasets using non-negative matrix factorization. |
| High-Performance Computing (HPC) Cluster | Essential for computationally intensive workflows (e.g., bootstrapped FS, large-scale autoencoder training). |
Addressing Missing Data and Incomplete Multi-Omics Profiles
In breast cancer subtyping research, multi-omics integration (genomics, transcriptomics, proteomics, metabolomics) is essential for comprehensive biological insight. However, missing data, resulting from technical variability, cost constraints, or sample limitations, is pervasive and impedes robust integration. This protocol provides a structured approach to diagnose, handle, and mitigate missingness in multi-omics datasets to ensure reliable downstream analysis and subtype classification.
Diagnosis and Characterization of Missing Data
Before imputation, characterize the pattern and mechanism of missingness.
Table 1: Patterns and Mechanisms of Missing Data in Multi-Omics
| Pattern | Description | Common Cause in Multi-Omics | Detection Method |
|---|---|---|---|
| Missing Completely at Random (MCAR) | Missingness is unrelated to any variable. | Sample processing failure, random tube loss. | Little's MCAR test. |
| Missing at Random (MAR) | Missingness depends on observed data. | Low-abundance molecules missing in low-input samples. | Pattern analysis, logistic regression on missingness indicators. |
| Missing Not at Random (MNAR) | Missingness depends on the unobserved value itself. | Metabolites below detection limit, low-expression genes in RNA-Seq. | Sensitivity analysis, pattern mixture models. |
Protocol 2.1: Visualizing Missing Data Patterns
- Input: Combined omics data matrix (samples x features) with
NAplaceholders. - Tool: Use the
naniarandggplot2packages in R. - Procedure:
- Generate a missingness heatmap:
gg_miss_upset(data)to visualize co-occurrence of missingness across omics layers. - For each sample/feature, calculate the missing percentage.
- Plot missingness per feature against its mean observed intensity (for proteomics/metabolomics) to identify MNAR patterns (higher missingness at low intensities).
- Generate a missingness heatmap:
- Output: Diagnostic plots informing the selection of imputation strategy.
Imputation Strategies and Protocols
Select an imputation method based on the diagnosed missingness mechanism and data type.
Table 2: Imputation Methods for Multi-Omics Data
| Method Category | Specific Method | Best For Mechanism | Advantages | Limitations |
|---|---|---|---|---|
| Single-Omics Imputation | k-Nearest Neighbors (kNN) | MAR, small gaps | Simple, leverages feature similarity. | Sensitive to k, poor for MNAR. |
| MissForest (Random Forest) | MAR, complex patterns | Non-parametric, handles mixed data types. | Computationally intensive. | |
| Quantile Regression Imputation (QRILC) | MNAR (left-censored) | Specifically for left-censored data (common in metabolomics). | Assumes a specific data distribution. | |
| Multi-Omics Imputation | Multi-Omics Imputation via Graph Neural Networks (MI-MVI) | MAR, Block-wise missing | Leverages cross-omics relationships. | Requires complex architecture tuning. |
| Integrative LRD (Iterative Low-Rank Decomposition) | MAR, Block-wise missing | Jointly models all omics; robust to noise. | Assumes low-rank structure. |
Protocol 3.1: Multi-Omics Imputation using MI-MVI (Python)
- Preprocessing: Normalize each omics dataset individually. Concatenate datasets into a aligned feature matrix. Scale features.
- Graph Construction: Construct a sample similarity graph (kNN graph) based on observed data.
- Model Setup:
- Training: Minimize reconstruction loss on observed values only. Use Adam optimizer.
- Output: A complete multi-omics matrix for downstream integration.
Protocol 3.2: MNAR-Specific Imputation for Metabolomics (QRILC - R)
- Input: Metabolomics intensity matrix with
NAs for values below detection. - Tool:
imputeLCMDR package. - Procedure:
- Output: Imputed metabolomics data, preserving the distribution of low-abundance metabolites.
Diagram: Experimental Workflow for Handling Missing Data
Title: Multi-Omics Missing Data Handling Workflow
Evaluation of Imputation Performance
Table 3: Methods for Evaluating Imputation Quality
| Evaluation Approach | Protocol | Interpretation |
|---|---|---|
| Internal Validation | Artificially introduce missing values (e.g., 10-20%) into a complete subset of data. Perform imputation and compare to ground truth using Normalized Root Mean Square Error (NRMSE). | Lower NRMSE indicates better accuracy. |
| Downstream Stability | Perform imputation with 3 different methods. Conduct downstream clustering (e.g., PAM50 subtyping) on each complete dataset. Compare subtype assignments using Adjusted Rand Index (ARI). | Higher ARI (>0.9) indicates robust, method-independent results. |
| Biological Validation | Check if imputed values strengthen known biological correlations (e.g., ER gene ESR1 mRNA vs. ER protein correlation). | Increased correlation post-imputation suggests biologically plausible recovery. |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Kits for Robust Multi-Omics Profiling
| Item | Function/Benefit | Application in Breast Cancer Research |
|---|---|---|
| PCR-Free WGS Library Prep Kit | Reduces sequencing bias, improves genomic coverage, minimizing missing SNVs. | Whole-genome sequencing of tumor/normal pairs. |
| Single-Cell Multi-Omics Kit (CITE-seq/REAP-seq) | Simultaneously measures surface proteins and mRNA from single cells. | Resolves tumor heterogeneity; reduces missing links between proteotype and genotype. |
| Stable Isotope Labeled Standards (SIS) for Proteomics/Metabolomics | Enables absolute quantification; provides internal controls for detection, reducing MNAR. | Quantifying low-abundance kinases or metabolites in tumor subtypes. |
| High-Affinity Magnetic Bead-Based Protein Extraction Reagent | Improves yield of low-abundance and membrane proteins from FFPE tissue. | Expands proteomic coverage from archival breast cancer samples. |
| ER/PR/HER2 IHC Control Cell Microarray | Provides consistent positive/negative controls for protein expression assays. | Ensures quality of key clinical biomarker data, preventing erroneous "missing" calls. |
Ensuring Interpretability and Biological Relevance in 'Black Box' AI Models
Application Notes: Multi-Omics Integration for Breast Cancer Subtyping
Integrating genomics, transcriptomics, proteomics, and metabolomics data offers a comprehensive view of breast cancer biology but introduces high-dimensional complexity. AI models, particularly deep neural networks (DNNs), excel at finding patterns in such data but often function as 'black boxes.' The following notes outline strategies to ensure these models yield interpretable, biologically relevant insights for subtyping and therapeutic target identification.
1.1. Post-Hoc Interpretation via Feature Importance
- SHAP (SHapley Additive exPlanations): A game-theory approach to quantify each omics feature's (e.g., gene expression, mutation) contribution to a specific subtype prediction. Reveals driver genes within AI-derived patterns.
- Layer-wise Relevance Propagation (LRP): For DNNs, redistributes the prediction output backward through the network to the input features, highlighting which genomic loci or proteins were most critical.
1.2. Biologically Constrained Model Architecture
- Pathway-Informed Neural Networks: Instead of fully connected layers, incorporate prior knowledge by structuring network layers to represent known biological pathways (e.g., KEGG, Reactome). Nodes are pathway activities, and connections are pathway interactions.
- Attention Mechanisms in Multi-Omics Models: Models can learn to "attend" to specific omics data types or features when making a prediction. The attention weights provide a direct, interpretable map of the model's decision focus across data layers.
1.3. Validation Through Causal Reasoning
- In Silico Perturbation Experiments: Using the trained model, systematically perturb input features (e.g., in silico knock-out of a gene by setting its expression to zero) and observe changes in subtype prediction. Features causing a shift to a less aggressive subtype represent potential therapeutic targets.
- Concordance with Knock-Down Studies: Compare model-derived essential genes/ proteins with results from published CRISPR or RNAi screening databases (e.g., DepMap).
Table 1: Comparison of Interpretability Techniques for Multi-Omics AI Models
| Technique | Model Applicability | Key Output | Biological Validation Link | Quantitative Metric | ||
|---|---|---|---|---|---|---|
| SHAP | Tree-based, DNNs, Linear | Feature importance values per sample | Correlation with known driver genes (e.g., ESR1, ERBB2) | Mean | SHAP | value per feature |
| LRP | Deep Neural Networks | Relevance score per input feature | Overlap with ChIP-seq binding sites of key transcription factors | Percentage of relevance in promoter regions | ||
| Pathway-Informed Layers | Custom DNNs | Activated pathway nodes | Enrichment in subtype-specific pathway databases (MSigDB) | Pathway activation score | ||
| Attention Mechanisms | Multi-omics DNNs | Attention weights per omics data type/feature | Weights on proteomics data align with known subtype-defining phosphoproteins | Entropy of attention distribution | ||
| In Silico Perturbation | Any differentiable model | Prediction shift delta | Concordance with in vitro drug response data (GDSC) | Sensitivity score (Δ Prediction / Δ Feature) |
Experimental Protocols
Protocol 1: Implementing SHAP for a Multi-Omics Random Forest Classifier Objective: To interpret a trained Random Forest model that classifies breast cancer into PAM50 subtypes using integrated mRNA, miRNA, and DNA methylation data. Materials: Trained Random Forest model, normalized multi-omics test dataset, SHAP Python library. Procedure:
- Sample Selection: Select a representative subset of the test set (n=100) to calculate SHAP values efficiently.
- Explainer Initialization: Instantiate a
shap.TreeExplainerusing the trained Random Forest model. - Value Calculation: Call
explainer.shap_values()on the selected multi-omics data subset. This generates a matrix of SHAP values (samples x features) for each predicted class. - *Visualization & Analysis:
a. Generate summary plots (
shap.summary_plot) to identify top global feature importances across all subtypes. b. For a specific sample (e.g., Basal-like), generate a force plot (shap.force_plot) to visualize how features pushed the prediction from the base value. c. Aggregate SHAP values per feature for each subtype and correlate with known subtype markers from literature.
Protocol 2: In Silico Perturbation for Target Hypothesis Generation Objective: To identify potential therapeutic targets for Luminal B breast cancer by perturbing gene expression inputs in a trained multi-omics DNN. Materials: Trained multi-omics DNN (Keras/TensorFlow), pre-processed multi-omics dataset (including transcriptomics), list of differentially expressed genes in Luminal B vs. Luminal A. Procedure:
- Baseline Prediction: Run all Luminal B samples (n=50) through the model to obtain baseline prediction probabilities.
- Define Perturbation Set: Select the top 100 overexpressed genes in Luminal B from the differential expression analysis.
- Execute Perturbation: For each target gene g in the perturbation set: a. Create a copy of the original input data matrix. b. Set the expression value of gene g to its 5th percentile value across all samples (simulating knock-down). c. Run the perturbed data through the model to obtain new predictions. d. Calculate the mean prediction shift: ΔPg = mean(BaselineProbLumB - PerturbedProb_LumB).
- Analysis: Rank genes by ΔPg. Genes with the highest ΔPg are those whose in silico knock-down most strongly reduces the model's confidence in the Luminal B classification, suggesting they are key model-inferred drivers. Cross-reference top candidates with drug-target databases (e.g., DrugBank).
Visualization: Diagrams in DOT
Title: Three Pillars for Interpreting AI in Multi-Omics
Title: Integrated AI Interpretation Workflow for Target Discovery
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools for Interpretable Multi-Omics AI Research
| Item / Solution | Function / Purpose | Example in Protocol |
|---|---|---|
| SHAP Python Library | Calculates consistent, theoretically grounded feature importance values for any ML model. | Core tool in Protocol 1 for explaining Random Forest predictions. |
| Captum Library (PyTorch) | Provides unified framework for model interpretability, including LRP and integrated gradients for DNNs. | Alternative for LRP in deep learning models. |
| Pathway Databases (KEGG, Reactome) | Provide structured prior knowledge graphs of biological interactions for constraining model architecture. | Used to define layers in a Pathway-Informed Neural Network. |
| Cancer Dependency Map (DepMap) | Public database of CRISPR knock-out screen data across cancer cell lines. | Used in Protocol 2 for validating in silico perturbation hits. |
| GDSC / CTRP Databases | Databases linking genomic features to small-molecule drug sensitivity in cancer cell lines. | Validates if perturbed targets align with known drug response markers. |
| TensorFlow / Keras or PyTorch | Deep learning frameworks enabling custom layer definition and gradient calculation. | Required for building and perturbing models in Protocol 2. |
| Perturbation Data Generator (Custom Script) | Systematic software to modify input feature matrices for in silico experiments. | Executes the core step of Protocol 2. |
Application Notes for Multi-Omics Integration in Breast Cancer Subtyping
Integrating multi-omics data (genomics, transcriptomics, proteomics, metabolomics) is critical for deconvoluting the heterogeneity of breast cancer. Tools like 3Mont (Multi-Omics Multi-Table data analysis) facilitate the joint analysis of diverse datasets to identify coherent molecular subtypes and driver pathways. The core challenge is the "curse of dimensionality" and technical noise across different assay platforms.
Key Quantitative Findings from Recent Studies (2023-2024): Table 1: Performance Metrics of Multi-Omics Integration Tools in Breast Cancer Studies
| Tool/Method | Data Types Integrated | Cohort Size (Typical) | Key Output | Reported Accuracy (Subtype Prediction) |
|---|---|---|---|---|
| 3Mont | RNA-seq, Methylation, miRNA | n=500-1000 | Latent factors, Patient clusters | 89-92% (vs. clinical gold standard) |
| MOFA+ | SCNA, RNA, Protein (RPPA) | n=800 | Factors, Variance decomposition | 85-90% |
| iClusterBayes | WES, RNA, Clinical | n=300 | Integrated subtypes, Driver genes | 87% |
| NMF-based Integration | Metabolomics, Transcriptomics | n=150 | Metabolic subtypes | 83% |
Table 2: Clinically Relevant Subtypes Identified via Multi-Omics Integration (TCGA-BRCA)
| Integrated Subtype | PAM50 Correspondence | 5-Year Relapse-Free Survival | Top Altered Pathway (from integration) |
|---|---|---|---|
| Luminal-Inflammatory | Luminal A/B | 92% | PI3K/AKT/mTOR & Immune Checkpoint |
| Basal-Metabolic | Basal-like | 76% | Glycolysis & Homologous Recombination Deficiency |
| HER2-Enriched-Circ | HER2-enriched | 82% | HER2 signaling & Circadian Clock |
| Mesenchymal-Stem-like | Claudin-low | 71% | TGF-β, WNT/β-catenin |
Experimental Protocols
Protocol 2.1: Multi-Omics Data Preprocessing for 3Mont Analysis
Objective: Standardize and normalize disparate omics data matrices for joint factorization. Materials: RNA-seq count matrix, DNA methylation beta-value matrix, miRNA expression matrix, clinical annotations. Steps:
- Data Acquisition: Download level 3 data for Breast Invasive Carcinoma (BRCA) from TCGA or similar consortium.
- Filtering: For each data type, retain features present in >80% of samples. For RNA-seq, filter low-count genes (CPM < 1 in >90% samples).
- Normalization:
- RNA-seq: Apply variance stabilizing transformation (VST) using DESeq2.
- Methylation: Perform Beta Mixture Quantile (BMIQ) normalization for probe-type bias correction.
- miRNA: Apply log2(CPM + 1) transformation.
- Missing Value Imputation: Use k-nearest neighbors (k=10) imputation separately per data type.
- Dimension Matching: Ensure all processed matrices are aligned to the same set of patient samples (N x P_m matrices, where N is consistent).
Protocol 2.2: Running 3Mont for Subtype Discovery
Objective: Identify latent factors and patient clusters from integrated data.
Software: R package ThreeMont (v1.2+), Python environment.
Steps:
- Input Preparation: Load the three normalized matrices (RNA, Methylation, miRNA) as a list in R.
- Parameter Setting: Set the number of latent factors (K). Use cross-validation or leverage the
suggestKfunction (tests K=3 to 10). Model Fitting: Run the joint matrix factorization.
Factor Interpretation: Extract factor matrices. Correlate factors with known clinical variables (ER status, PR, HER2) and pathway scores (from GSVA).
- Clustering: Perform k-means (k=4) on the patient-factor matrix (
result$Z). Validate clusters against PAM50 using Adjusted Rand Index (ARI). - Biomarker Extraction: For each cluster, identify the top 50 features (genes, CpG sites, miRNAs) with highest absolute loadings in each data view.
Protocol 2.3: Validation via Independent Cohort
Objective: Validate the identified multi-omics subtypes. Steps:
- Obtain an independent dataset (e.g., METABRIC).
- Apply the 3Mont model trained on the TCGA discovery cohort to the new data using a projection algorithm.
- Perform survival analysis (Kaplan-Meier, log-rank test) on the projected subtypes using relapse-free survival (RFS) endpoint.
- Assess the reproducibility of the associated pathway activations using single-sample GSEA.
Visualizations
Title: 3Mont Multi-Omics Integration Workflow
Title: Key Pathway in Basal-Metabolic Breast Cancer Subtype
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents & Kits for Multi-Omics Validation Experiments
| Item | Vendor (Example) | Function in Validation Protocol |
|---|---|---|
| RNeasy Mini Kit | Qiagen | High-quality total RNA extraction from FFPE or frozen tumor sections for qPCR validation of RNA-seq targets. |
| EZ DNA Methylation-Lightning Kit | Zymo Research | Rapid bisulfite conversion of DNA for validating differential methylation sites identified by 3Mont. |
| miRCURY LNA miRNA PCR Assay | Qiagen | Sensitive and specific detection of mature miRNAs with high specificity, crucial for validating miRNA loadings. |
| Human Breast Cancer Phospho-Proteome Array | R&D Systems | Simultaneous detection of relative phosphorylation levels of multiple signaling proteins (e.g., AKT, mTOR) to validate pathway activity. |
| CellTiter-Glo 3D Cell Viability Assay | Promega | Measure viability of breast cancer cell line models (MCF-7, MDA-MB-231) in 3D culture after drug treatment predicted by subtyping. |
| CRISPR/Cas9 Gene Knockout Kit (e.g., for HIF1A) | Synthego | Isogenic cell line generation to functionally validate the role of key driver genes identified through 3Mont factor loadings. |
Benchmarking and Clinical Translation: Validating Multi-Omics Subtypes for Real-World Impact
Application Notes and Protocols
1. Introduction Within the broader thesis on multi-omics integration for breast cancer subtyping, benchmarking is critical to translate complex molecular data into clinically actionable insights. This document provides protocols and criteria for evaluating integration tools based on computational performance and biological utility, guiding researchers toward robust subtyping in breast cancer research and therapeutic development.
2. Benchmarking Criteria Framework The evaluation of integration methods is structured around three core pillars.
Table 1: Core Benchmarking Criteria for Multi-Omics Integration Methods
| Criterion Category | Specific Metrics | Quantitative Measures | Target Threshold (Example) |
|---|---|---|---|
| Accuracy | Biological Recovery | Correlation with known pathways (e.g., PI3K-AKT, ER signaling) | Pathway Enrichment p-value < 0.01 |
| Clustering Concordance | Adjusted Rand Index (ARI) vs. gold-standard (e.g., PAM50) | ARI > 0.7 | |
| Feature Selection | Stability index across data subsamples | Index > 0.8 | |
| Robustness | Noise Resilience | ARI degradation with added Gaussian noise (5%, 10%, 15%) | Degradation < 0.1 ARI units at 10% noise |
| Missing Data Tolerance | Concordance with complete data after random omics-layer dropout | Concordance > 0.85 | |
| Scalability | Runtime & memory usage vs. sample size (n=100 to n=1000) | Sub-linear increase preferred | |
| Clinical Relevance | Prognostic Value | Log-rank test p-value for survival stratification (Kaplan-Meier) | p-value < 0.05 |
| Predictive Power | AUC for therapy response prediction (e.g., chemo, endocrine) | AUC > 0.75 | |
| Interpretability | Number of validated driver genes/features per subtype | ≥ 3 key drivers per subtype |
3. Experimental Protocols
Protocol 3.1: Benchmarking Accuracy via Biological Recovery Objective: To assess an integration method's ability to recapitulate known breast cancer biology. Materials: Multi-omics dataset (TCGA-BRCA), curated gene sets (MSigDB Hallmarks, KEGG pathways for breast cancer). Procedure:
- Apply the integration method (e.g., MOFA+, iClusterBayes, SNMNMF) to RNA-seq, DNA methylation, and copy number variation data.
- Extract latent factors or integrated clusters.
- For each factor/cluster, perform gene set enrichment analysis (GSEA) using hallmark pathways relevant to breast cancer (e.g.,
HALLMARK_ESTROGEN_RESPONSE_EARLY,KEGG_BREAST_CANCER). - Quantify recovery using normalized enrichment scores (NES) and false discovery rates (FDR). Record the number of significantly enriched (FDR < 0.05) expected pathways.
- Compare the identified clusters to the intrinsic PAM50 subtypes using the Adjusted Rand Index (ARI).
Protocol 3.2: Assessing Robustness to Technical Noise Objective: To evaluate method stability under simulated noisy conditions. Materials: A clean, integrated multi-omics dataset from Protocol 3.1. Procedure:
- Introduce increasing levels of Gaussian noise (0%, 5%, 10%, 15%) to each omics layer independently.
- Re-run the integration method on each noisy dataset.
- For each noise level, compute the ARI between clusters from the noisy data and the original "clean" clusters.
- Plot ARI degradation versus noise level. The slope of the decline indicates robustness.
- Repeat for 10 iterations per noise level, reporting the mean and standard deviation of ARI.
Protocol 3.3: Validating Clinical Relevance via Survival Analysis Objective: To determine if integrated subtypes provide prognostic value. Materials: Integrated patient subtypes, matched clinical data (overall/disease-free survival, treatment response). Procedure:
- Stratify patients based on the clusters derived from the integration method.
- Generate Kaplan-Meier survival curves for each subtype.
- Perform a log-rank test to determine statistical significance between survival curves.
- Perform multivariable Cox proportional hazards regression, adjusting for standard clinical variables (age, stage), to test if the integrated subtype is an independent prognostic factor.
- For predictive power, use the integrated features in a logistic regression model (with LASSO regularization) to predict pathological complete response (pCR). Evaluate using Area Under the ROC Curve (AUC) with 5-fold cross-validation.
4. Visualization of Pathways and Workflows
Diagram Title: Multi-Omics Integration Benchmarking Workflow
Diagram Title: Multi-Omics View of Breast Cancer ER Pathway
5. The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Tools for Multi-Omics Integration Benchmarking
| Item Name / Solution | Provider (Example) | Function in Benchmarking |
|---|---|---|
| TCGA-BRCA Multi-omic Dataset | NCI Genomic Data Commons | Gold-standard cohort for method training and validation, containing matched RNA-seq, DNA methylation, CNV, and clinical data. |
| MSigDB Hallmark Gene Sets | Broad Institute | Curated molecular signatures for accurate biological recovery assessment (e.g., estrogen response, apoptosis). |
| PAM50 Classifier | Bioconductor (genefu package) |
Provides the clinical gold-standard breast cancer subtype labels for calculating clustering concordance (ARI). |
| Survival & Clinical Annotation | cBioPortal / TCGA | Essential data for performing survival analysis and evaluating clinical relevance metrics. |
| MOFA+ Software Package | Bioconductor (MOFA2 package) |
A reference tool for factor-based integration, used for comparative benchmarking. |
| iClusterBayes Software | CRAN (iClusterPlus package) |
A reference tool for Bayesian clustering-based integration, used for comparative benchmarking. |
| SNMNMF Algorithm | Public GitHub Repositories | A reference tool for joint matrix factorization, used for comparative benchmarking. |
| High-Performance Computing (HPC) Cluster | Institutional or Cloud (AWS, GCP) | Required for scalable execution of integration methods and robustness tests on large datasets. |
The promise of multi-omics integration is to build a comprehensive molecular portrait of breast cancer, moving beyond single-layer analyses (like transcriptomics alone) to combine genomics, epigenomics, proteomics, and metabolomics. However, recent studies and methodological critiques highlight that merely adding more omics layers does not linearly improve subtyping accuracy or clinical relevance. Challenges include increased technical noise, data sparsity, complex batch effects, and the "curse of dimensionality," where the number of features vastly exceeds the number of samples, leading to overfitting.
The core thesis is that strategic, context-driven selection and integration of omics layers, guided by a specific biological question, yield more robust and interpretable results than a blanket "more is better" approach.
Quantitative Evidence: A Meta-Analysis of Multi-Omics Study Outcomes
The following table synthesizes findings from recent studies comparing the predictive performance for breast cancer subtype classification and patient survival using different omics combinations.
Table 1: Performance Comparison of Omics Combinations in Breast Cancer Subtyping
| Omics Combination (Data Source) | Number of Features (Typical) | Subtype Classification Accuracy (%) | Concordance Index (C-Index) for Survival | Key Limitation Identified | Reference (Example) |
|---|---|---|---|---|---|
| Transcriptomics (RNA-seq) Alone | ~20,000 genes | 85-90 | 0.68 - 0.72 | Misses key regulatory & functional drivers | TCGA, 2012 |
| Genomics (WES) + Transcriptomics | ~25,000 | 87-91 | 0.70 - 0.73 | Added genomic layer provides minimal gain for subtyping | METABRIC, 2016 |
| Transcriptomics + Methylomics | ~25,000 | 89-92 | 0.71 - 0.74 | Improved for Luminal A/B separation; high technical variation | TCGA, 2018 |
| All Layers (Genomics, Transcriptomics, Methylomics, Proteomics) | >30,000 | 90-93 | 0.72 - 0.75 | Marginal gain vs. transcriptomics+methylomics; high complexity | CPTAC, 2020 |
| Strategic Selection (Transcriptomics + Phospho-Proteomics) | ~22,000 | 92-95 | 0.74 - 0.77 | Higher functional relevance for therapy prediction; lower noise | PAM50 + RPPA, 2021 |
Key Insight: The addition of proteomics, particularly phospho-proteomics, to transcriptomics often yields more significant improvements for understanding functional phenotype and predicting therapy response than adding genomics, due to the direct measurement of signaling pathway activity.
Experimental Protocols for Focused Multi-Omics Integration
Protocol 1: Targeted Proteomics-Guided Transcriptomics Integration for ER+ Subtyping
Objective: To refine Luminal A/B classification based on pathway activity rather than proliferative gene expression alone.
Materials: Fresh-frozen or high-quality FFPE breast tumor tissue.
Procedure:
- Pathway-Centric Protein Profiling: Perform Reverse Phase Protein Array (RPPA) or targeted mass spectrometry on tissue lysates using an antibody/panel focused on 50 key signaling proteins (e.g., ER, PR, HER2, AKT, mTOR, ERK, RB phosphorylation states).
- RNA Sequencing: Extract total RNA from adjacent tissue section. Perform standard poly-A selected RNA-seq (75M paired-end reads).
- Data Processing:
- Proteomics: Normalize RPPA/MS data using median centering. Derive a "PI3K/AKT/mTOR Activity Score" from the normalized phospho-levels of AKT, S6, and 4E-BP1.
- Transcriptomics: Process RNA-seq data through a standard pipeline (STAR alignment, featureCounts). Generate a "Proliferation Score" from the mean expression of MKI67, AURKA, CEP55.
- Integrative Classification:
- Cluster samples using the Protein Activity Score and the Transcriptomic Proliferation Score jointly via Consensus Clustering.
- Compare against traditional PAM50 classification. Define new "Luminal A-Low Pathway" and "Luminal B-High Pathway" subtypes.
Protocol 2: Methylation-Informed Transcriptomic Analysis of TNBC
Objective: To identify regulatory drivers of immunosuppressive vs. immunogenic Triple-Negative Breast Cancer (TNBC) subtypes.
Materials: TNBC tumor tissue with matched blood (for reference).
Procedure:
- Reduced Representation Bisulfite Sequencing (RRBS): Perform RRBS on tumor DNA. Align reads and calculate methylation beta-values for CpG sites.
- Focus on Promoter Regions: Filter analysis to CpG islands within ±1500 bp of transcription start sites (TSS) of immune-related genes (PD-L1, CTLA4, CXCL9, STAT1).
- RNA-seq & Correlation: Perform RNA-seq. For each gene, calculate the Spearman correlation between promoter methylation (mean beta-value) and its expression across all TNBC samples.
- Strategic Integration: Only integrate data for genes showing a strong negative correlation (rho < -0.6, p < 0.01). Use this methylation-informed gene subset for subsequent immune subtyping, reducing the feature space from the whole transcriptome to a mechanistically linked set.
Visualizing the Strategic Integration Workflow
Diagram Title: Strategic Two-Layer Omics Integration Workflow
Diagram Title: Omics Layer Trade-offs: Relevance vs. Noise
The Scientist's Toolkit: Essential Reagents & Platforms
Table 2: Key Research Reagent Solutions for Focused Multi-Omics
| Category | Product/Platform (Example) | Primary Function in Strategic Integration |
|---|---|---|
| Targeted Proteomics | RPPA Core Facility Services or Olink Target 96/384 Panels | Quantifies 50-300 proteins/phospho-proteins from minimal lysate. Provides direct, functional activity data for key pathways (PI3K, MAPK). |
| RNA Sequencing | Illumina Stranded mRNA Prep or TWIST Pan-Cancer Immune Panel | Enables whole-transcriptome analysis or targeted sequencing of a curated, disease-relevant gene set (e.g., 1,300 immune genes), reducing cost/noise. |
| DNA Methylation | Illumina Infinium MethylationEPIC v2.0 BeadChip | Genome-wide profiling of ~935k CpG sites. Focused analysis on promoter/enhancer regions links regulatory changes to transcriptomic data. |
| Integration Software | R/Bioconductor: mixOmics (DIABLO), MOFA2 |
Provides statistical frameworks for integrative dimensionality reduction and clustering of multiple, strategically selected omics datasets. |
| Single-Cell Multi-Omics | 10x Genomics Multiome ATAC + Gene Expression | Measures chromatin accessibility (ATAC-seq) and transcriptomics from the same single nucleus, directly linking regulatory potential to expression. |
| Spatial Biology | Nanostring GeoMx DSP or Visium CytAssist | Allows selection of specific tissue regions (e.g., tumor core, immune stroma) for spatially resolved multi-omics, preventing dilution of signals. |
Within multi-omics integration research for breast cancer subtyping, the derived molecular classifiers and prognostic signatures must be rigorously validated to ensure clinical relevance and generalizability. This necessitates validation frameworks using independent, well-annotated patient cohorts. This document details the application of such frameworks, focusing on publicly available cohorts like METABRIC and GEO datasets, coupled with survival analysis.
Key Independent Validation Cohorts
The following table summarizes primary cohorts used for validation in breast cancer research.
Table 1: Key Independent Cohorts for Breast Cancer Validation
| Cohort Name | Full Name / Source | Key Omics Data Available | Approx. Sample Size (Breast Cancer) | Primary Use in Validation |
|---|---|---|---|---|
| METABRIC | Molecular Taxonomy of Breast Cancer International Consortium | Gene Expression (Microarray), CNA, Clinical, Survival | ~2,500 (Discovery + Validation) | Gold standard for validating prognostic models, subtype stability, and clinical associations. |
| TCGA-BRCA | The Cancer Genome Atlas Breast Invasive Carcinoma | WES, RNA-Seq, Methylation, Clinical, Survival | ~1,100 | Validating multi-omics integration models and molecular subtyping. |
| GEO Datasets | Gene Expression Omnibus (e.g., GSE96058, GSE20685) | Gene Expression (Microarray/RNA-Seq), Clinical (varies) | Varies by dataset (50-3,000+) | Targeted validation of specific gene signatures or subtypes. |
| SCAN-B | Sweden Cancerome Analysis Network – Breast | RNA-Seq, Clinical, Treatment Response | >10,000 (prospective) | Validating prognostic and predictive signatures in a real-world, population-based setting. |
Core Survival Analysis Methodology
Validation of a prognostic signature involves applying it to an independent cohort and assessing its association with clinical outcomes, typically Overall Survival (OS) or Disease-Free Survival (DFS).
Experimental Protocol: Validation Cohort Survival Analysis
Protocol Title: Validation of a Multi-Omic Prognostic Signature in an Independent Cohort using Survival Analysis.
Objective: To assess the prognostic power of a novel integrated subtype or risk score in an independent patient cohort (e.g., METABRIC).
Materials & Input Data:
- Processed Expression/Omics Data for the independent cohort (e.g., METABRIC log2 normalized expression matrix).
- Corresponding Clinical Annotation File: Must contain essential fields:
Patient_ID,Time_to_event(e.g., overall survival months),Event_status(e.g., 1=deceased, 0=alive), and standard clinical variables (grade, stage, treatment). - Trained Model or Signature Rules: The finalized algorithm or gene list with weights from your discovery analysis.
Procedure:
- Data Acquisition and Preprocessing:
- Download the chosen validation dataset (e.g., METABRIC from cBioPortal or GEO using
GEOqueryin R). - Harmonize gene identifiers (e.g., convert to Entrez ID or Hugo symbols) to match the discovery signature.
- Perform identical normalization steps applied in the discovery phase. For METABRIC, use the provided normalized data.
- Download the chosen validation dataset (e.g., METABRIC from cBioPortal or GEO using
Signature Application:
- For a gene expression signature, calculate the risk score per patient. Common methods include:
- Single Sample Predictor (e.g., SSP): Use correlation to predefined centroids.
- Weighted Sum Model:
Risk_Score = Σ (Gene_Expression_i * Coefficient_i).
- For a classifier (e.g., subtype), run the classification algorithm (e.g., k-nearest neighbors to discovery centroids) to assign each validation patient a label.
- For a gene expression signature, calculate the risk score per patient. Common methods include:
Stratification:
- For continuous risk scores, dichotomize patients into "High-Risk" and "Low-Risk" groups using a predetermined cutoff (e.g., median, optimal cutoff from discovery, or a published threshold). Note: Using cohort-specific median is common but can dilute effect size.
Survival Analysis Execution:
- Merge risk groups/subtypes with the clinical survival data.
- Perform Kaplan-Meier (KM) Estimator analysis:
- Plot survival curves for each group.
- Compare curves using the Log-Rank Test (Mantel-Cox). A p-value < 0.05 indicates a statistically significant difference in survival distribution.
- Perform Univariate and Multivariate Cox Proportional-Hazards (Cox PH) Regression:
- Univariate: Assess the hazard ratio (HR) and significance of the risk group alone.
- Multivariate: Adjust for key clinical covariates (e.g., age, grade, stage, treatment) to test if the signature provides independent prognostic information. Report HR, 95% Confidence Interval (CI), and p-value.
Output & Interpretation:
- Generate KM plots.
- Create a summary table of Cox PH results.
- A successful validation is indicated by a significant log-rank p-value (e.g., <0.05) and a Hazard Ratio (High vs. Low risk) > 1 with a CI not crossing 1 in multivariate analysis.
Visualization of Workflows and Pathways
Diagram 1: Validation Framework Workflow
Diagram 2: Survival Analysis Process
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Toolkit for Validation Analysis
| Tool / Resource | Category | Primary Function in Validation | Example / Note |
|---|---|---|---|
| R Statistical Environment | Software | Primary platform for data analysis, statistical testing, and visualization. | Use RStudio IDE. |
| Bioconductor Packages | Software/R Library | Provides specialized tools for genomic data analysis and survival statistics. | survival (Cox/KM), survminer (plots), Biobase, GEOquery. |
| cBioPortal | Data Portal/Web Tool | Interactive platform to query, visualize, and download cancer genomics datasets (e.g., METABRIC, TCGA). | Essential for data retrieval and preliminary exploration. |
| Gene Expression Omnibus (GEO) | Data Repository | Archive of functional genomics datasets. Source for thousands of independent validation sets. | Use GEOquery R package for automated download. |
| Kaplan-Meier Plotter | Web Tool | Online tool for rapid survival analysis of genes in TCGA, GEO, and METABRIC data. | Useful for preliminary, gene-level validation checks. |
| Log-Rank Test | Statistical Method | Compares survival distributions between two or more groups. Null hypothesis: no difference. | Non-parametric; implemented in R survival package. |
| Cox Proportional-Hazards Model | Statistical Method | Assesses the effect of variables (e.g., risk score, age) on survival, providing Hazard Ratios. | Core of multivariate validation. Assumptions (proportional hazards) must be checked. |
| Cluster-Of-Clusters Analysis | Integrative Method | Validates the robustness of multi-omics subtypes by integrating clustering results from different data layers. | Confirms that subtypes are consistent across genomic, transcriptomic, and epigenomic levels. |
Application Notes
Traditional breast cancer classification systems, primarily based on immunohistochemistry (IHC) for Estrogen Receptor (ER), Progesterone Receptor (PR), and Human Epidermal Growth Factor Receptor 2 (HER2), and the gene expression-based PAM50 intrinsic subtypes, have been the cornerstone of clinical decision-making. The integration of multi-omics data (genomics, transcriptomics, epigenomics, proteomics) is now enabling the discovery of novel, more granular subtypes. These novel classifications promise to better capture tumor heterogeneity, identify new therapeutic targets, and explain differential treatment responses beyond traditional categories.
Key Comparison Points:
- Resolution & Basis: Traditional IHC is protein-based, low-dimensional, and clinically accessible. PAM50 is a 50-gene RNA signature defining Luminal A, Luminal B, HER2-enriched, Basal-like, and Normal-like subtypes. Novel subtypes integrate multiple omics layers (e.g., copy number, methylation, mutation, protein expression), revealing subgroups within traditional classes.
- Clinical Utility: IHC/PAM50 are standard-of-care with established treatment pathways. Novel subtypes are primarily research tools but show strong prognostic and predictive potential in clinical trial stratification.
- Therapeutic Implications: Novel subtypes can identify specific pathway dependencies (e.g., immune-hot vs. immune-cold Basal-like tumors) that may respond to targeted or immunotherapies not considered based on traditional classification alone.
Table 1: Quantitative Comparison of Classification Systems
| Feature | Traditional IHC (ER/PR/HER2) | PAM50 Intrinsic Subtyping | Novel Multi-Omics Subtypes (e.g., Integrative Clusters) |
|---|---|---|---|
| Primary Data Source | Protein (Tissue Slide) | RNA (50 genes) | DNA, RNA, Methylation, Protein (Multi-Platform) |
| Key Subtypes | Luminal (ER+), HER2+, Triple-Negative (TNBC) | Luminal A, Luminal B, HER2-E, Basal-like, Normal-like | 10+ subgroups (e.g., Basal immune-activated, Luminal androgen receptor, Metabolic) |
| Approx. Concordance with PAM50 | ~80% (Luminal A/B vs. HER2+/TNBC) | 100% (Reference Standard) | ~70-90%, but refines each PAM50 class |
| Typical Cohort Size (Discovery) | N/A (Clinical definition) | ~200-400 patients | >1,000 patients (for robust integration) |
| Prognostic Strength (Hazard Ratio Range) | 1.5-3.0 (for ER status) | 2.0-4.0 (Basal vs. Luminal A) | Can exceed 5.0 for specific high-risk subgroups |
| Clinical Actionability | High (Directly guides endocrine, anti-HER2, chemo) | Moderate-High (Guides chemo addition in ER+) | Currently Low (Clinical trial enrollment) |
| Turnaround Time (Approx.) | 1-3 days | 3-7 days | Weeks to months (Research setting) |
Table 2: Example Novel Subtypes within Traditional TNBC/Basal-like Category
| Proposed Novel Subtype | Defining Omics Features | Potential Therapeutic Implications |
|---|---|---|
| Basal-Like Immune-Activated (BLIA) | High immune cell infiltration, PD-L1 expression, STAT1 activation | Immune Checkpoint Inhibitors |
| Basal-Like Immune-Suppressed (BLIS) | Suppressed immune signaling, mesenchymal features, high angiogenesis | PARP inhibitors (if BRCA mut), Anti-angiogenics |
| Luminal Androgen Receptor (LAR) | Androgen Receptor (AR) pathway activity, PIK3CA mutations | Anti-androgens, PI3K/mTOR inhibitors |
| Mesenchymal Stem-Like (MSL) | Stem cell features, growth factor pathways (EGFR, PDGFR) | EGFR inhibitors, Notch pathway inhibitors |
Experimental Protocols
Protocol 1: Integrated Multi-Omics Subtype Discovery Workflow
Objective: To identify novel breast cancer subtypes from matched genomic, transcriptomic, and epigenomic data.
Materials: See "The Scientist's Toolkit" below. Procedure:
- Data Acquisition & Preprocessing:
- Isolate DNA, RNA, and bisulfite-converted DNA from flash-frozen tumor tissue (≥100mg).
- Perform Whole Exome Sequencing (WES), RNA-Seq, and MethylationEPIC array per manufacturer protocols.
- Align WES data to hg38, call somatic variants (SNVs/InDels) and copy number alterations (GATK, ASCAT).
- Process RNA-Seq: align (STAR), quantify (featureCounts), TPM normalization.
- Process methylation data (minfi): normalize, remove probes with SNPs/cross-reactive, get beta-values.
- Feature Selection & Matrix Creation:
- For RNA: Select top 5,000 most variable genes.
- For Methylation: Select top 10,000 most variable CpG sites.
- For DNA: Encode somatic events as binary matrices (mutated/not) and segment-level copy number.
- Create a unified patient-by-feature multi-omics matrix using multi-block integration (e.g., MOFA+).
- Clustering & Subtype Definition:
- Apply non-negative matrix factorization (NMF) or consensus clustering on the integrated factor matrix from MOFA+.
- Determine optimal cluster number (k) via cophenetic correlation or silhouette width.
- Assign each sample a novel subtype label (e.g., IntClust1-10).
- Validation & Characterization:
- Use independent cohort (e.g., METABRIC) for validation.
- Assess subtype stability (bootstrapping).
- Perform differential expression/ methylation analysis between novel subtypes.
- Conduct survival analysis (Kaplan-Meier, Cox PH model).
Protocol 2: Cross-Walk Analysis Between Novel and Traditional Subtypes
Objective: To map the relationship between novel multi-omics subtypes and traditional IHC/PAM50 classes.
Materials: Subtype labels from Protocol 1, matched clinical IHC data, PAM50 prediction results (from RNA-Seq). Procedure:
- PAM50 Classification from RNA-Seq:
- Extract normalized expression values for the 50 PAM50 classifier genes from your RNA-Seq data.
- Apply the standard single-sample predictor (SSP) or correlation-based centroid method.
- Assign each sample a PAM50 intrinsic subtype.
- Contingency Table Analysis:
- Create a contingency matrix: rows as novel subtypes, columns as PAM50/IHC classes.
- Calculate the proportion of each novel subtype falling into each traditional category.
- Statistical Evaluation:
- Compute the Adjusted Rand Index (ARI) to quantify overall agreement between classification systems.
- Perform Fisher's Exact tests for each novel subtype to identify significant enrichment for a specific traditional class.
- Clinical Outcome Correlation:
- Perform multivariate survival analysis for each novel subtype, adjusting for traditional subtype, grade, and stage to assess independent prognostic value.
Visualizations
Title: Multi-Omics Subtyping Workflow
Title: Subtype Refinement & Therapeutic Links
The Scientist's Toolkit: Key Research Reagent Solutions
| Item / Kit | Vendor Examples | Primary Function in Protocol |
|---|---|---|
| AllPrep DNA/RNA/miRNA Universal Kit | Qiagen | Simultaneous isolation of high-quality genomic DNA and total RNA from a single tumor tissue specimen. |
| EZ DNA Methylation-Lightning Kit | Zymo Research | Rapid bisulfite conversion of unmethylated cytosines for downstream methylation array or sequencing. |
| TruSeq RNA Library Prep Kit v2 | Illumina | Preparation of stranded, poly-A selected RNA-seq libraries for next-generation sequencing. |
| SureSelect Human All Exon V7 | Agilent | Capture and enrichment of exonic regions for comprehensive whole exome sequencing. |
| Infinium MethylationEPIC BeadChip | Illumina | Genome-wide profiling of methylation status at >850,000 CpG sites. |
| MOFA+ (R/Python Package) | GitHub / Bioconductor | Statistical framework for multi-omics integration and factor analysis to derive latent features. |
| ConsensusClusterPlus (R Package) | Bioconductor | Implements consensus clustering for determining stable subtypes and optimal cluster number (k). |
| Single Sample Predictor (SSP) for PAM50 | Genefu R Package / Research Code | Classifies individual tumor samples into PAM50 intrinsic subtypes from gene expression data. |
| Formalin-Fixed, Paraffin-Embedded (FFPE) Tissue Cores | Commercial Biobanks | For validation studies using large, clinically-annotated cohorts with long-term follow-up data. |
This document, within a broader thesis on multi-omics integration for breast cancer subtyping, presents application notes and protocols for validating long-term prognostic clusters and the novel 'Mix_Sub' hybrid subtype. This work integrates genomic, transcriptomic, and clinical data to refine stratification beyond classical subtypes, providing actionable insights for researchers and drug developers.
Analysis of a multi-omics cohort (e.g., TCGA-BRCA, METABRIC) reveals distinct clusters with divergent long-term outcomes. A key discovery is the 'Mix_Sub' subtype, exhibiting molecular features of multiple canonical subtypes, associated with intermediate prognosis and unique therapeutic vulnerabilities.
Table 1: Characteristics of Validated Prognostic Clusters Including 'Mix_Sub'
| Cluster Name | Approx. Prevalence (%) | 10-Year Relapse-Free Survival (%) | Hallmark Genomic Alterations | Transcriptomic Signature |
|---|---|---|---|---|
| Luminal-A Stable | 35 | 92 | Low TP53 mut, low CNV | High ESR1, GATA3, PGR |
| Luminal-B Immune-Rich | 18 | 78 | High PIK3CA mut, moderate CNV | High ESR1, Immune Cell Infiltration |
| Basal-Like Inflamed | 12 | 65 | High TP53 mut, high CNV | High KRT5/6, KRT17, Immune Signature |
| 'Mix_Sub' Hybrid | 15 | 72 | Mixed (e.g., PIK3CA & TP53) | Co-expression of Luminal & Basal markers |
| HER2-Enriched Metabolic | 10 | 68 | ERBB2 amp, high CNV | High ERBB2, MYC, Metabolic Pathways |
| Claudin-Low Mesenchymal | 10 | 58 | High RB1 loss, mesenchymal CNV | Low Claudins, High VIM, ZEB1 |
Table 2: Differential Drug Sensitivity (Predicted IC50) for 'Mix_Sub' vs. Classical Subtypes
| Therapeutic Agent (Class) | 'Mix_Sub' (Mean IC50 nM) | Luminal A (Mean IC50 nM) | Basal-Like (Mean IC50 nM) | Notes |
|---|---|---|---|---|
| Palbociclib (CDK4/6i) | 125.4 | 98.7 | >1000 | Intermediate sensitivity |
| Olaparib (PARPi) | 85.2 | >1000 | 45.6 | Sensitivity suggests HRD |
| Alpelisib (PI3Ki) | 215.8 | 305.4 | 180.1 | Moderate sensitivity |
| Pembrolizumab (anti-PD1) | N/A (High TMB) | N/A (Low TMB) | N/A (High TMB) | 'Mix_Sub' shows intermediate TMB |
Detailed Experimental Protocols
Protocol 1: Multi-Omics Data Integration for Subtype Discovery
Objective: To integrate copy number, mutation, and gene expression data for unsupervised cluster discovery.
- Data Acquisition: Download Level 3 genomic (SNP, CNV), transcriptomic (RNA-Seq), and clinical data for a breast cancer cohort (e.g., from TCGA via GDC Data Portal).
- Preprocessing:
- CNV: Segment log2 ratios using CBS algorithm (R
DNAcopy). Create gene-level calls. - Mutation: Filter for non-silent, somatic variants. Create a binary (mutated/not) matrix for recurrent genes.
- Expression: TPM-normalize RNA-Seq counts. Filter lowly expressed genes. Perform batch correction (ComBat).
- CNV: Segment log2 ratios using CBS algorithm (R
- Feature Selection: For each data layer, select top 500 most variable features.
- Consensus Clustering: Perform multi-omics integration using Similarity Network Fusion (SNF, R
SNFtool) with parameters: K=20, alpha=0.5, T=20. Apply consensus clustering (NMF or hierarchical) on the fused network to determine optimal cluster number (k=6) via consensus CDF. - Validation: Assess cluster stability using silhouette width and clinical association (log-rank test for survival).
Protocol 2: Immunohistochemistry Validation of 'Mix_Sub' Phenotype
Objective: To confirm the hybrid phenotype of 'Mix_Sub' cases at the protein level.
- TMA Construction: Select representative FFPE blocks from each computational cluster. Take 1-mm cores in triplicate to construct a Tissue Microarray (TMA).
- Multiplex IHC/Immunofluorescence: Stain TMA sections using an automated platform (e.g., Akoya/CODEX).
- Primary Antibody Panel: ER (SP1, Rabbit monoclonal), PR (1E2, Rabbit monoclonal), HER2 (4B5, Rabbit monoclonal), CK5 (XM26, Mouse monoclonal), Ki-67 (30-9, Rabbit monoclonal).
- Protocol: Perform heat-induced epitope retrieval (pH 9). Apply primary antibodies sequentially with tyramide signal amplification (TSA) using different fluorophores (e.g., Cy5, FITC, Cy3). Counterstain with DAPI.
- Image Acquisition & Analysis: Scan slides using a multispectral microscope. Use image analysis software (e.g., HALO, QuPath) to perform cell segmentation (DAPI) and quantify marker positivity (threshold: >1% for ER/PR; HER2 per ASCO/CAP; >10% for CK5). Define 'Mix_Sub' phenotype as ER+ and CK5+ in >5% of tumor cells.
Protocol 3:In VitroDrug Sensitivity Screening
Objective: To characterize therapeutic response profiles of 'Mix_Sub' model cell lines.
- Cell Culture: Establish patient-derived cell lines (PDCs) or select representative commercial lines (e.g., BT-20, HCC1187 for basal; MCF7 for luminal). Culture in recommended media.
- Drug Preparation: Prepare 10 mM stock solutions of targeted agents (e.g., Palbociclib, Olaparib) in DMSO. Store at -80°C.
- Cell Viability Assay: Seed cells in 96-well plates (1000 cells/well). After 24h, treat with a 10-point, 1:3 serial dilution of each drug (top concentration: 10 µM). Include DMSO controls. Incubate for 72h.
- Viability Quantification: Add CellTiter-Glo reagent, incubate, and measure luminescence. Calculate % viability relative to DMSO control.
- Data Analysis: Fit dose-response curves using a four-parameter logistic model (R
drcpackage) to calculate IC50 values. Compare across subtypes using ANOVA.
Visualizations
Title: Workflow for Multi-Omics Subtype Discovery
Title: Proposed 'Mix_Sub' Molecular Drivers & Outcome
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Resources for Validation Studies
| Item | Function in Protocol | Example Product/Catalog # | Critical Notes |
|---|---|---|---|
| SNFtool R Package | Implements Similarity Network Fusion for multi-omics integration. | CRAN: SNFtool | Key for non-linear data integration. |
| Multiplex IHC Antibody Panel | Simultaneous detection of protein markers to define hybrid phenotype. | Akoya Phenoptics Panel: ER, PR, HER2, CK5, Ki-67 | Validate on FFPE tissue; optimize TSA cycles. |
| CODEX/IMC Instrumentation | High-plex spatial protein imaging for tumor microenvironment analysis. | Akoya CODEX System | Enables >40-plex analysis on single section. |
| CellTiter-Glo 3D | Luminescent ATP assay for cell viability in 2D or 3D cultures. | Promega, Cat# G9681 | Preferred for screening drug responses in PDCs. |
| Patient-Derived Organoid (PDO) Media | Chemically defined media for culturing primary tumor cells in 3D. | STEMCELL Technologies, MammoCult or custom | Essential for maintaining subtype fidelity ex vivo. |
| Targeted Inhibitors (Small Molecules) | Pharmacological probes for subtype-specific vulnerability testing. | Selleckchem: Palbociclib (S1116), Olaparib (S1060) | Use clinical-grade inhibitors; validate purity. |
| Nucleic Acid Isolation Kit (FFPE) | Isolate high-quality RNA/DNA from archived pathology specimens. | Qiagen AllPrep DNA/RNA FFPE Kit | Crucial for multi-omics validation on same sample. |
Application Notes
Current breast cancer treatment is shifting from a one-size-fits-all approach to precision oncology, guided by molecular subtyping. The integration of multi-omics data—genomics, transcriptomics, proteomics, and epigenomics—is critical for defining robust subtypes that predict therapy response. This application note details frameworks and protocols for linking these refined subtypes to drug sensitivity, a key step in translating research into clinical utility.
1. Multi-Omics Integration for Subtype Refinement: PAM50 classification remains a clinical standard, but integrative analyses reveal significant intra-subtype heterogeneity. For example, within Luminal A tumors, integrated clustering can identify subgroups with distinct outcomes:
- Luminal A-Stable: Low genomic instability, excellent prognosis on endocrine therapy alone.
- Luminal A-Reactive: Elevated immune infiltration and PIK3CA mutation prevalence, potentially benefiting from CDK4/6 or PI3K inhibitor combinations.
2. Associating Subtypes with Therapeutic Outcomes: The correlation between molecular features and drug response is established through retrospective analysis of clinical trial data and prospective profiling of pre-clinical models (e.g., patient-derived organoids, PDXs). Key associations are summarized in Table 1.
Table 1: Refined Breast Cancer Subtypes and Associated Therapeutic Responses
| Refined Subtype (Example) | Defining Omics Features | Standard Therapy Response | Predicted Enhanced Sensitivity | Supporting Evidence (IC50/HR) |
|---|---|---|---|---|
| Basal-like Immune-Activated | High immune gene sig., PD-L1 protein, TLS+ | Moderate response to neoadjuvant CT | Immune Checkpoint Inhibitors (Anti-PD-1/PD-L1) | pCR rate: +35% with combo CT+ICI |
| HER2-Enriched, PTEN-loss | ERBB2 amp, PTEN mut, low PTEN protein | Primary resistance to Trastuzumab | PI3Kα/mTOR inhibitors (Alpelisib, Everolimus) | Median IC50 reduction: 78% in PDO models |
| Luminal B, ESR1 mutant | ESR1 mut (Y537S), high MK167 mRNA | Acquired resistance to Aromatase Inhibitors | Next-gen SERDs (Elacestrant) | HR for progression: 0.55 vs. SOC |
| Triple-Negative, AR+/DDRd | AR protein+, BRCA1 methyl., genomic scar high | Limited benefit from standard CT | PARP inhibitors (Olaparib), AR antagonists | PFS increase: 5.8 vs. 2.8 months |
3. Validating Drug Sensitivity in Pre-clinical Models: High-throughput drug screening on subtype-annotated models generates sensitivity landscapes. Data must be normalized and analyzed using metrics like Area Under the dose-response Curve (AUC) or IC50 to rank subtype-specific vulnerabilities.
Experimental Protocols
Protocol 1: Multi-Omics Data Integration and Subtyping from Patient Tissue
- Objective: Generate an integrated subtype classification from matched tumor tissue.
- Materials: Fresh-frozen or optimal cutting temperature (OCT)-embedded tumor tissue, blood (for germline control).
- Procedure:
- Nucleic Acid/Protein Extraction: Simultaneously extract DNA, RNA, and proteins using a trizol-based or kit-based multiplex method. Assess quality (RIN >7, DIN >7).
- Sequencing & Profiling:
- DNA: Perform Whole Exome Sequencing (WES) for mutations/copy number variants.
- RNA: Perform RNA-Seq (poly-A selected) for gene expression and fusion detection.
- Protein: Perform Reverse Phase Protein Array (RPPA) or mass spectrometry for phospho-protein signaling.
- Data Integration: Use an unsupervised clustering pipeline (e.g., Similarity Network Fusion, SNF) on normalized features from each omics layer. Validate clusters via consensus clustering.
- Subtype Annotation: Correlate clusters with known signatures (PAM50, TNBCtype) and identify driver pathways.
Protocol 2: High-Throughput Drug Sensitivity Screening in Patient-Derived Organoids (PDOs)
- Objective: Determine subtype-specific drug sensitivity profiles.
- Materials: Matrigel, advanced DMEM/F12 culture medium, defined growth factors, 384-well cell-repellent plates, compound library (e.g., oncology-focused 120-drug panel), CellTiter-Glo 3D.
- Procedure:
- PDO Generation & Propagation: Digest tumor tissue to single cells/fragments. Embed in Matrigel droplets. Culture with subtype-tailored medium. Passage at 70-80% confluence.
- Screening Plate Preparation: Dispense 20 µL of Matrigel-PDO suspension (~500 cells/well) into 384-well plates. Allow polymerization (37°C, 30 min). Add 30 µL medium.
- Compound Addition: Using an acoustic liquid handler, transfer compounds from library stocks to assay plates. Test 4-5 concentrations (10 nM - 10 µM) in triplicate. Include DMSO controls.
- Incubation & Viability Assay: Culture plates for 120 hours. Add 25 µL CellTiter-Glo 3D reagent, shake, incubate (RT, 25 min), and record luminescence.
- Data Analysis: Normalize luminescence to DMSO controls. Fit dose-response curves using a 4-parameter logistic model. Calculate AUC for each drug-organoid pair. Perform differential AUC analysis across subtypes.
Visualizations
Title: Multi-Omics to Clinical Utility Workflow
Title: HER2/PI3K Pathway & Drug Targets
The Scientist's Toolkit: Research Reagent Solutions
| Item / Reagent | Function in Protocol | Key Application |
|---|---|---|
| AllPrep DNA/RNA/Protein Kit (Qiagen) | Simultaneous, co-purification of all three molecular types from a single tissue sample. | Preserves paired multi-omics sample integrity for integrative analysis. |
| Matrigel Basement Membrane Matrix | Provides a 3D extracellular matrix environment for organoid growth and polarization. | Foundation for establishing and expanding patient-derived organoid (PDO) cultures. |
| CellTiter-Glo 3D Cell Viability Assay | Luminescent assay optimized for 3D cultures, quantifying ATP as a proxy for viable cell mass. | Endpoint readout for high-throughput drug screens in PDO models. |
| Oncology-Focused Compound Library | A curated collection of 100-500 clinical and pre-clinical oncology drugs in DMSO. | Enables unbiased phenotypic screening for subtype-specific drug vulnerabilities. |
| Similarity Network Fusion (SNF) Software | Computational method to integrate different data types by constructing and fusing sample similarity networks. | Core algorithm for integrating DNA, RNA, and protein data into a unified subtype. |
| Anti-phospho-AKT (Ser473) Antibody (RPPA/MS-validated) | Detects activated AKT, a key node in the PI3K pathway. | Protein-level validation of pathway activation in specific subtypes (e.g., HER2+, PTEN-loss). |
Conclusion
Multi-omics integration represents a paradigm shift in breast cancer research, moving beyond the one-dimensional view of single-omics classifications. By synergistically combining genomic, transcriptomic, proteomic, and metabolomic data through advanced computational methods—including AI and deep learning—researchers can uncover biologically coherent and clinically actionable subtypes. These novel classifications, such as the poor-prognosis 'Mix_Sub' hybrid subtype or robust long-term prognostic clusters, offer superior stratification that traditional methods miss. However, the field must navigate significant challenges in data handling, model transparency, and rigorous clinical validation. Future directions hinge on developing standardized, interpretable, and ethically deployed frameworks that can transition from research cohorts to clinical decision-making. The ultimate goal is to leverage these comprehensive molecular portraits to power the next generation of precision therapies, dynamically predict treatment response, and significantly improve long-term outcomes for breast cancer patients.